Policy Brief: Medicaid Key to Building Comprehensive Substance Use Care System for Low-Income People
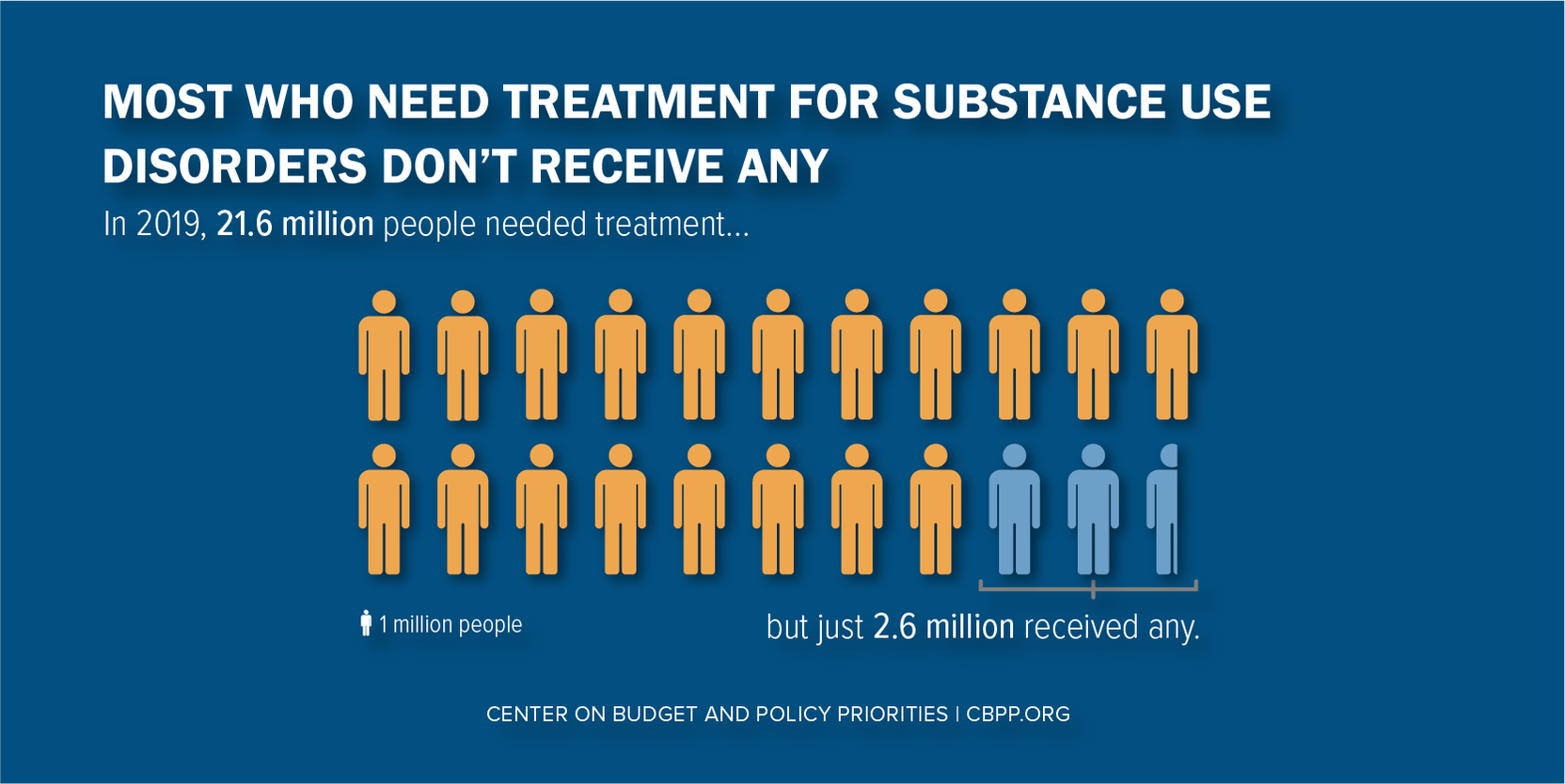
Robust and reliable funding for substance use disorder (SUD) services is essential for closing the treatment gap, where fewer than 13 percent of the 21 million-plus people who need substance use services get any.[1] (See Figure 1.) A comprehensive system of SUD care would provide a full continuum of treatment and recovery services to people living with all types of substance use disorders, integrate care for their co-occurring physical and mental health conditions, advance racial equity in treatment access and quality, and connect people with services to meet their social needs. Medicaid should be the foundation for funding comprehensive care for people with low incomes.
Inaccessible SUD care can lead to the placement of children into foster care, job loss, racial disparities in outcomes — and preventable deaths. An average of 95,000 people died each year from excessive alcohol use between 2011 and 2015, the Centers for Disease Control and Prevention conservatively estimates. And drug overdose deaths set a new record of over 71,000 in 2019, and were likely even higher in 2020.
Medicaid can cover a rich array of clinical SUD treatment services, recovery supports, and other mental and physical health care.Medicaid can cover a rich array of clinical SUD treatment services, recovery supports, and other mental and physical health care. And in contrast to annually appropriated grant programs, Medicaid guarantees health coverage to all who qualify, so funding adjusts to meet rising need. To fully leverage Medicaid for this purpose, state and federal policymakers should start by taking the following steps.
States That Haven’t Yet Implemented Medicaid Expansion Should Do So
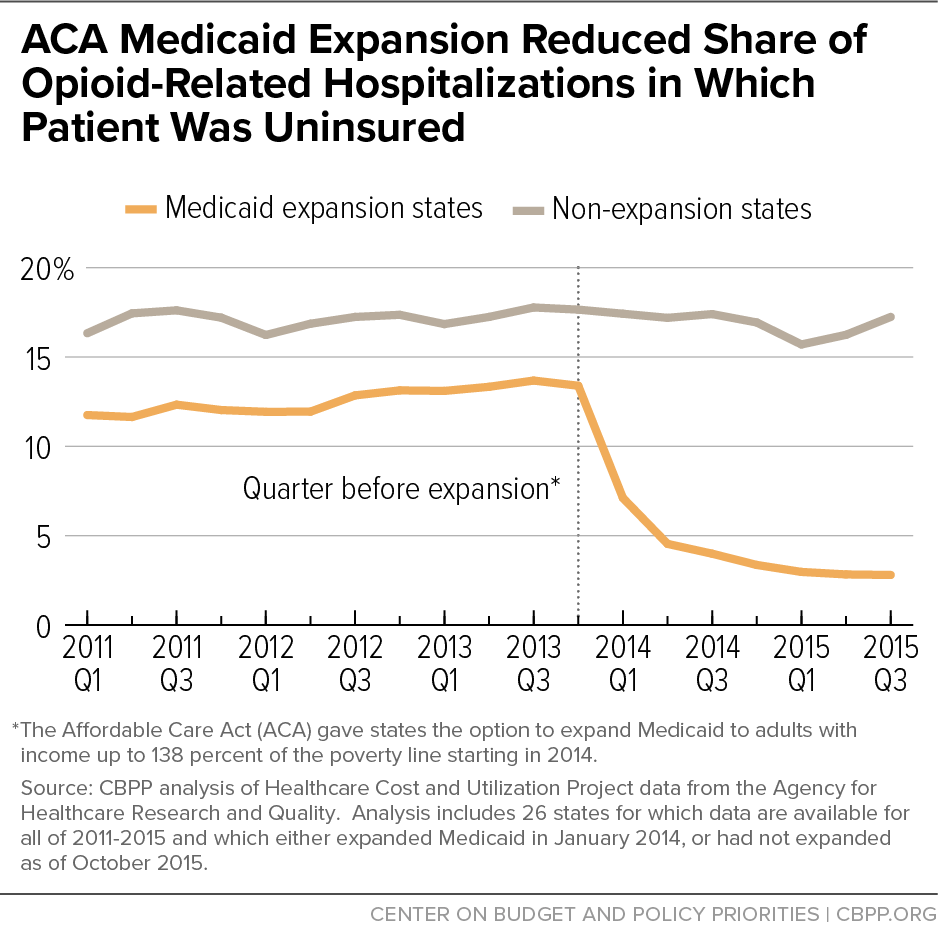
Many low-income people remain uninsured, particularly in states that have yet to expand Medicaid. (Twelve states have not yet adopted expansion; Missouri and Oklahoma have but have yet to implement it.) In the states that have expanded, the program has been a powerful tool for improving coverage and access to care for people with SUDs. The uninsured rate among people with opioid-related hospitalizations fell dramatically in states that expanded, from 13.4 percent in 2013 (just before expansion) to 2.9 percent two years later. (See Figure 2.)
While Medicaid expansion is already a great financial deal for states, the American Rescue Plan Act provides an additional financial incentive for the remaining states to quickly expand. If they do, the Act gives them a two-year, 5-percentage-point increase in their federal medical assistance percentage (FMAP) for all non-expansion enrollees, who account for most of a state’s Medicaid enrollees and costs. In addition to increasing coverage, the enhanced federal match gives states a big boost in federal funding that they could use to enhance SUD services, for example by covering additional services in their state Medicaid plans.
Ensure That State Medicaid Plans Cover Full Continuum of SUD Services
The American Society of Addiction Medicine’s (ASAM) nationally recognized criteria recommend that SUD continuum of care seamlessly transition people between different levels of care — from early interventions to outpatient services and residential and inpatient services — as their treatment and recovery needs change. The continuum should include services that reduce barriers to recovery, such as peer supports and supportive housing and supported employment, as well as treatment for co-occurring conditions, such as serious mental illness, diabetes, or HIV/AIDS.
States have multiple ways to fund these clinical care and recovery support services in their Medicaid programs. Yet only 12 states’ Medicaid plans covered services across all ASAM levels of clinical SUD services in 2018, according to the most recent comprehensive analysis. Federal policymakers should encourage states to cover the full continuum of SUD services in their Medicaid programs. States can leverage new Medicaid funding from the American Rescue Plan Act, including the expansion incentive and the one-year, 10-percentage-point increase in federal Medicaid funds intended to enhance home- and community-based services, which include many SUD services.
Encourage More Qualified SUD Providers to Participate in Medicaid
Even if state Medicaid programs cover a full range of SUD services, Medicaid beneficiaries may lack access to comprehensive care when there aren’t enough qualified SUD providers participating in Medicaid. This lack of provider capacity — an estimated 40 percent of counties lack an outpatient treatment program, for example — is due to several factors. There are far fewer psychiatrists, substance use counselors, and social workers than needed to serve people with SUDs, and even fewer SUD providers participate in Medicaid. Providers may lack resources to set up the infrastructure necessary to participate in Medicaid. And Medicaid payment rates, which states have broad discretion to set, are often too low.
Providers new to Medicaid may need help launching information and electronic medical records systems, setting up a process to review utilization of services, and tracking Medicaid quality measures that other programs often don’t require. Helping providers create these systems would not only allow them to participate in Medicaid but also enhance the quality of the services they provide. And states can boost provider reimbursement rates, including with the additional funding that the American Rescue Plan Act provides.
Ensure That Grants, Other Temporary Funding Complement Medicaid
Grants, which alone are neither sufficient nor the right mechanism to fund a full continuum of SUD services, play an essential role in filling funding gaps, building provider capacity, and promoting racial equity when coordinated with Medicaid and other funding. The same is true for other sources of capped or short-term funding, such as funds from opioid lawsuit settlements.
Whenever possible, federal and state policymakers should use grant funding to complement the services that state Medicaid programs cover rather than to pay for Medicaid-funded services. Better coordinating Medicaid and grant funding would help ensure that more people with substance use disorders can obtain the treatment and the comprehensive supports that they need.
Expand Access to Affordable Housing, Child Care, Other Unmet Social Needs
Low-income individuals, including many Medicaid beneficiaries, face higher risk of unmet social needs that interfere with their SUD recovery. These unmet needs often reflect systemic racism and contribute to racial disparities in treatment outcomes. A long history of discriminatory housing policies, present-day landlord discrimination, and criminalization of homelessness all create additional barriers to housing for people of color, and Black people in particular. While Medicaid can provide an important bridge to social services, direct investments in affordable housing, child care, voluntary employment services, and other supports are essential.
New resources included in the American Rescue Plan Act are a down payment on the investments needed to ensure that people with low incomes can access SUD services and maintain recovery. The Act will reduce severe levels of hardship for tens of millions of people most affected by the COVID-19 pandemic and recession — especially Black and Latinx families — by providing housing assistance that will prevent millions of impending evictions, funding that will make child care more affordable for many families, and food assistance to address widespread food insecurity.
Policymakers should build on the progress the Act provides by making sustained investments in housing, child care, and other social services to lower barriers to SUD recovery for years to come. For example, if they made Housing Choice Vouchers an entitlement program like Medicaid and SNAP — meaning that the program would automatically assist all eligible applicants — many more people in recovery would have access to stable housing. If policymakers fail to take these longer-term steps, the gains that the American Rescue Plan Act’s historic investments likely will achieve will diminish as funding returns to pre-pandemic levels, which were rife with inequities.
End Notes
[1] The full version of this report is available at https://www.cbpp.org/research/health/medicaid-is-key-to-building-a-system-of-comprehensive-substance-use-care-for-low.
More from the Authors

Areas of Expertise

Areas of Expertise
Recent Work:

Areas of Expertise