A provision in the House economic relief bill would give the 14 states that haven’t yet implemented Medicaid expansion under the Affordable Care Act (ACA) a strong new financial incentive to do so.[1] The COVID-19 pandemic and recession have made access to health care — including Medicaid — even more critical, and more than 4 million uninsured people in the states that haven’t expanded could gain coverage if all remaining states acted.
States that have expanded Medicaid have dramatically lowered their uninsured rates; the people gaining coverage are healthier and more financially secure as a result; and expansion has reduced long-standing racial disparities in health outcomes, coverage, and access to care. It also has produced net savings for many states. Not only does the federal government pay most of the cost of expansion coverage, but expansion produces offsetting state savings, such as reducing spending on uncompensated care and increasing revenue from the taxes that some states impose on health plans and providers.
Despite the evidence of expansion’s benefit to people and state budgets, some state officials in non-expansion states still claim that their state can’t afford the modest amount of money a state must contribute.[2] Under the provision in the House bill, states that newly expand Medicaid would receive a 5-pecentage-point increase in their federal medical assistance percentage (or FMAP) for two years. The additional federal dollars from this increase would exceed the full state cost of covering the expansion group in each of the holdout states.
If enacted, the House provision should settle the argument about whether a state can afford expansion and push the remaining states to adopt expansion quickly.
Under the ACA, the federal government pays 90 percent of the cost of the people enrolled in expansion coverage. By comparison, the FMAP for other Medicaid enrollees varies between 50 and 78 percent, depending on the state.
State and independent analyses, including in states such as Arkansas, Kentucky, Louisiana, Michigan, Montana, and Virginia, have consistently showed expansion produced net savings for many states.[3] That’s because, in addition to the generous FMAP, expansion allows states to spend less on programs related to the uninsured (such as uncompensated care) and collect more revenue from taxes on the managed care plans through which many Medicaid beneficiaries get their coverage. Indeed, expansion states saw “no significant changes in spending from state revenues associated with Medicaid expansion” compared to non-expansion states, according to a comprehensive analysis of state budget data in the New England Journal of Medicine. The analysis found “no evidence that Medicaid expansion forced states to cut back on spending on other priorities.”[4]
The House provision would make this deal even better for states. Newly expanding states would receive a 5-percentage-point increase in their FMAP for all non-expansion enrollees, who account for most of a state’s Medicaid enrollees and costs. The increase would begin the first day of the quarter that expansion begins and last for two years. If, for example, a state decided to expand and began coverage on July 1, 2021, the state would get the higher FMAP through June 2023. (See Appendix Table 1 for estimates of additional federal funds by state.)
This increase would come on top of the 6.2-percentage-point FMAP increase that all states will receive for the duration of the public health emergency under last year’s Families First Act, which will provide $86 billion in additional federal Medicaid dollars in 2020 and 2021.[5] (The Biden Administration has indicated it will continue the public health emergency at least through 2021.)
More than 4 million uninsured people could gain Medicaid coverage if the remaining states expanded.[6] In addition to rapid gains in health coverage, taking up the expansion would help the states:
- Bring relief to front-line workers and others most at risk during the pandemic and recession. Hundreds of thousands of people in the holdout states who could gain Medicaid coverage are at elevated risk of contracting, being hospitalized for, or dying from COVID-19. They include 640,000 people working in essential and front-line jobs such as grocery store workers and home health aides, 500,000 people with disabilities, and 926,000 people aged 50-64.[7] People with low incomes have higher rates of asthma, heart disease, and other health conditions that raise their risk of becoming seriously ill or dying from COVID-19; expansion can connect them with coverage and help them access needed care.
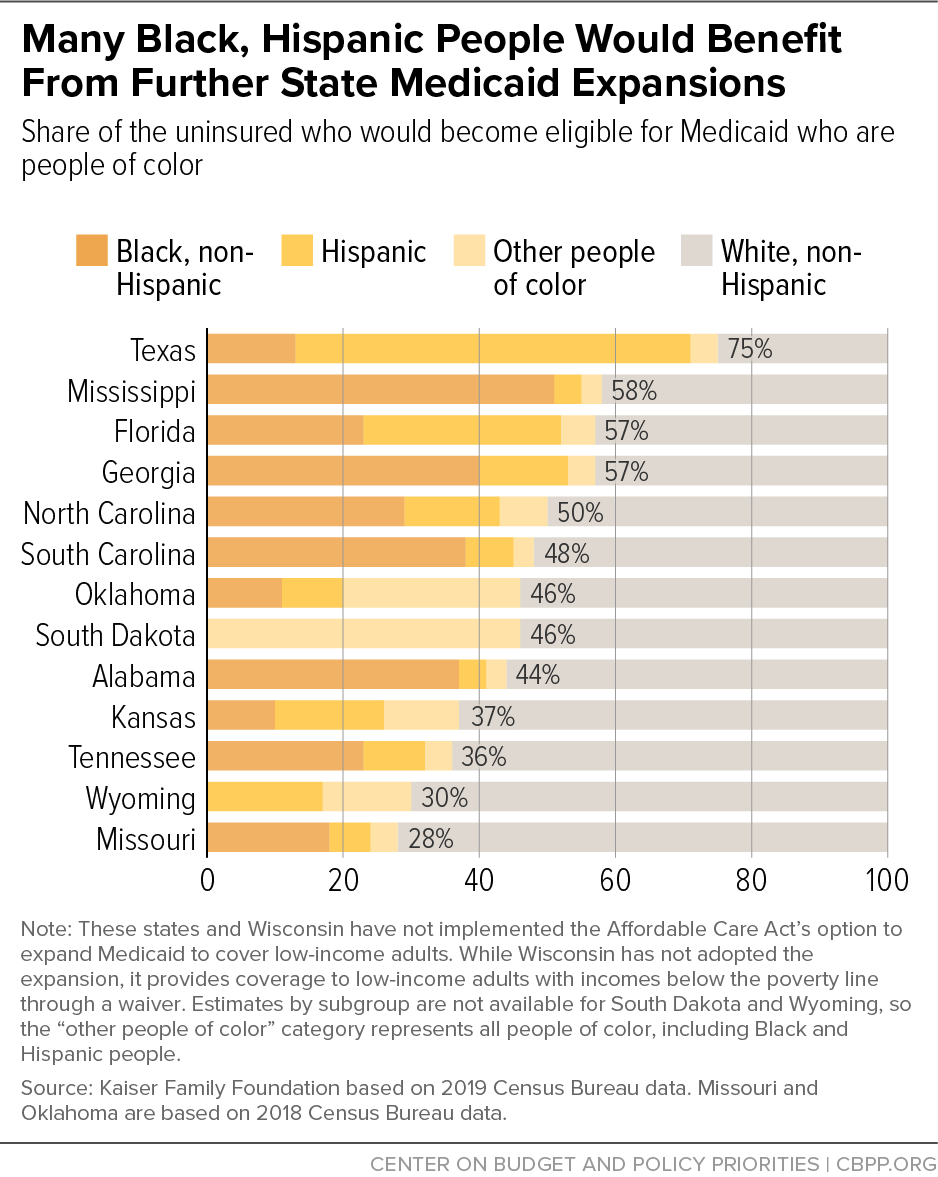
- Reduce long-standing racial disparities in coverage and access to care. Eleven of the 14 non-expansion states are in the South, and 60 percent of those who would gain coverage are people of color,[8] a group particularly harmed by COVID-19. (See Figure 1.) Black, Hispanic, and Indigenous people are being hospitalized and dying from the virus at the highest rates.[9] While expansion won’t eliminate these and other long-standing racial disparities, experience from other states shows that it narrows disparities in coverage and access to care and improves health outcomes among people of color.[10]
- Bring a significant amount of new federal funding into their state. Even without the House provision, expansion would provide a financial windfall to states that newly expand: if all the holdout states adopted the expansion, they would bring an additional $30 billion into their economies each year, the Urban Institute projects.[11]
As explained above, the House provision would provide an infusion of federal funding on top of what a state typically receives when it expands Medicaid. Those added federal dollars exceed what a state would receive if the temporary FMAP increase applied to the Medicaid expansion group; they also exceed the full cost of covering the expansion group over the first two years. This two-year window would take states through the period when demand for Medicaid will be highest due to the pandemic and recession. The added funds would free up state funds, allowing states to plug holes in other parts of their budgets caused by the economic crisis and avoid cuts to Medicaid, education, and other public services.
As existing expansion states have shown, a state that decides to adopt the expansion can implement it quickly and get people enrolled in coverage, especially if the state begins making system changes as soon as it announces its intention to expand. For example, Alaska’s expansion took effect just a month and a half after Governor Bill Walker announced the state’s intention to expand. In Maine, expansion enrollment began one week after Governor Janet Mills signed an executive order to start implementation. A new expansion state could also utilize some of the strategies that other states have used to enroll people quickly, such as automatically enrolling people from other federal programs like the Supplemental Nutrition Assistance Program (SNAP), enrolling parents based on their children’s Medicaid eligibility, and expanding presumptive eligibility.[12]
Given the pandemic and recession, it is more important than ever that the remaining states adopt the Medicaid expansion and extend health coverage to some of their most vulnerable residents. The House provision provides a powerful financial incentive for these states to move quickly. And while some expansion opponents might point to the two-year duration of the added federal funds as a reason not to expand, that concern would be unfounded. The House provision would give states that expand in the coming years a windfall of additional federal dollars in the near term, while the enhanced federal funds for Medicaid expansion itself ensure the program will be sustainable over the longer term.
| APPENDIX TABLE 1 |
| State |
Additional federal funding due to FMAP increase (in $millions) |
| Alabama |
940 |
| Florida |
3,540 |
| Georgia |
1,880 |
| Kansas |
330 |
| Mississippi |
890 |
| Missouri |
1,730 |
| North Carolina |
2,430 |
| Oklahoma |
860 |
| South Carolina |
960 |
| South Dakota |
180 |
| Tennessee |
1,660 |
| Texas |
5,970 |
| Wisconsin* |
1,000 |
| Wyoming |
120 |