BEYOND THE NUMBERS
Women Face Large Coverage Losses, Especially in Non-Expansion States, if Enhanced Premium Assistance Expires
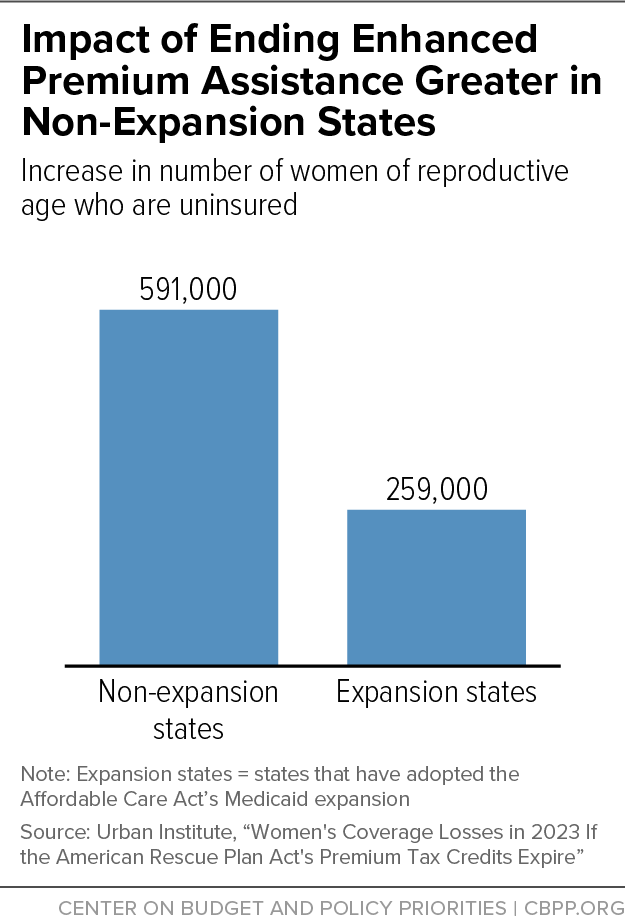
If Congress doesn’t extend enhanced premium assistance for people buying marketplace health coverage, 850,000 women of reproductive age will lose their coverage and become uninsured next year, a new Urban Institute report finds. More than two-thirds of them — about 590,000 — live in the 12 states that haven’t adopted the Affordable Care Act’s (ACA) Medicaid expansion (see chart).
The 850,000 newly uninsured women would join the 800,000 women of reproductive age who are in the Medicaid coverage gap, meaning they have no affordable coverage because their incomes are below the poverty level and they live in states that have refused to adopt the Medicaid expansion. People in the coverage gap have incomes too low to qualify for premium tax credits to buy ACA marketplace plans, and they are barred from Medicaid because their states have refused to adopt the expansion.
These facts highlight the urgent need for policymakers to both extend the premium tax credit enhancements in last year’s American Rescue Plan and close the coverage gap.
Two prior analyses — one from the Urban Institute and another from the Department of Health and Human Services — each estimated that overall, more than 3 million people would become uninsured if the premium tax credit enhancements expire as scheduled this year, and more than 10 million others would face steep increases in premium costs.
The new Urban study finds that in the 12 non-expansion states, the number of women of reproductive age who are uninsured would jump by more than 20 percent, far exceeding the 7 percent increase in expansion states. The largest percentage coverage loss if the enhancements expire would occur in Georgia, where the number of uninsured women of reproductive age would increase by 27 percent. Other states facing steep coverage losses include South Carolina and Florida, where the number of women of reproductive age who are uninsured would increase by 25 percent and 23 percent, respectively.
Here's why coverage losses would be concentrated in non-expansion states. Under the ACA, people with incomes below the poverty level (about $13,000 a year for an individual) aren’t eligible for subsidized marketplace coverage, but those between the poverty level and 138 percent of the poverty level are eligible for subsidized marketplace coverage if they aren’t eligible for Medicaid. That means in non-expansion states, many more people with incomes between 100 percent and 138 percent of the poverty level are in the marketplace than in expansion states, where people in those income ranges generally qualify for Medicaid. If the premium credits become less generous, some people with marketplace coverage and incomes between 100 percent and 138 percent of the poverty level will no longer be able to afford their coverage. In expansion states, people in that income range are typically eligible for Medicaid and therefore do not have marketplace coverage. But in non-expansion states, they generally aren’t, and many will end up uninsured when they drop marketplace coverage and can’t get Medicaid.
Overall, 2.2 million uninsured people in non-expansion states — 60 percent of whom are people of color — will continue to lack a pathway to coverage if policymakers don’t close the coverage gap.
Ensuring that people who can get pregnant have access to health coverage is all the more important after the recent Supreme Court decision overturning the legal right to abortion. If the premium tax credit enhancements expire, Urban estimates that in the states with the least access to abortion, 384,000 fewer women of reproductive age would have health coverage. By itself, ensuring access to affordable marketplace plans wouldn’t address the abortion access crisis or the many barriers low-income people face in accessing abortion; in 34 states, marketplace plans don’t cover abortion, often because of state bans. But closing the Medicaid coverage gap and extending the premium tax credit enhancements would enable people to get coverage for contraception and other reproductive health services — including preconception health care, which is critical to healthy birth outcomes.