BEYOND THE NUMBERS
Over 4,300 Arkansas Beneficiaries Lost Medicaid This Month for Not Meeting Rigid Work Requirements
Over 4,300 Arkansas Medicaid beneficiaries lost their coverage on September 1, likely becoming uninsured, because they didn’t report at least 80 hours of work or work-related activities for June, July, and August, the state reports. These people, the first Medicaid beneficiaries in any state to lose coverage because they couldn’t comply with complex work requirements, represent about 17 percent of the first cohort subject to Arkansas’ requirement. They’re locked out of Medicaid for the rest of 2018 even if they report 80 hours of work or work-related activities in future months or become exempt from the requirement due to illness or other reasons.
Roughly 5,000 other beneficiaries now have two months of non-compliance with the work requirement and will lose coverage if they don’t report that they’ve complied for another month this year. And over 6,100 have one month of non-compliance and will lose coverage if they have two more. Thousands of these beneficiaries are likely to lose coverage in the coming months.
Many of these beneficiaries likely complied with the requirement or qualified for an exemption but struggled with the problem-ridden online portal — the only way that Arkansas lets beneficiaries report. Adding to the portal-related challenges, the state acknowledged that it experienced a computer problem that may have limited access to the website during the crucial reporting window and is extending the reporting deadline for one month for those affected if they request a “good cause” exemption due to the computer issues. As with other good cause exemptions, however, beneficiaries have the burden of knowing the exemption exists and emailing a request to the agency, which may prove hard for beneficiaries with limited Internet and email access.
The good cause exemptions, intended to protect beneficiaries who can’t comply with the requirements due to life events such as hospitalization, serious illness, or domestic violence, have proven ineffective at protecting vulnerable beneficiaries. The state granted only 45 good cause exemptions for July even though almost 12,000 beneficiaries didn’t comply with the reporting requirement that month.
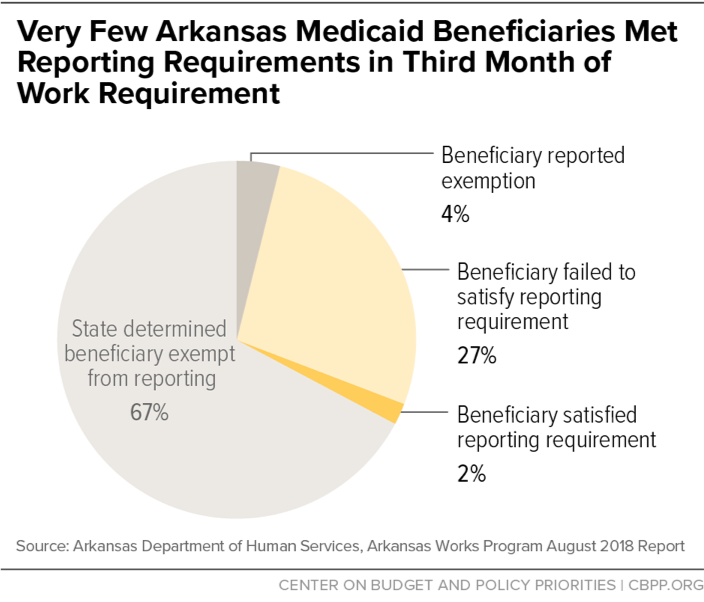
As we’ve explained, research suggests that only a small minority of Medicaid beneficiaries potentially subject to the state’s work requirement aren’t already working and wouldn’t qualify for an exemption. Yet a much larger number of beneficiaries are accruing months of non-compliance and losing coverage, which suggests that the complex policy and reporting requirements are tripping up many eligible beneficiaries. Recent interviews with 18 Arkansas Medicaid beneficiaries support this conclusion:
- Twelve of the 18 weren’t aware of the new work requirement.
- Most of the interviewees who, based on their age, should have received a letter from the state letting them know they were subject to the work requirement weren’t sure they received one. And those who did were confused or overwhelmed by the new requirements.
- Many reported the online portal would be a challenge for them or their family members to use because they lacked a smartphone or Internet access.
- Most importantly, none of the interviewees reported that the policy had led them — or would lead them — to change their work-related activities, as most of them were already working, actively seeking work, or exempt.
Governor Asa Hutchinson claimed yesterday that more than 1,000 beneficiaries have found work since the work requirements took effect in June, but there’s no evidence that that occurred due to the work requirement. Some beneficiaries start new jobs every month regardless of the threat of losing coverage. The state’s data show that in August, almost 2,000 beneficiaries in the state’s Medicaid expansion population — most of whom aren’t yet subject to the requirement — left Medicaid because their incomes rose above program limits.
Even if some beneficiaries sought help finding a job due to the work requirement, that impact must be balanced against the fact that 4,300 beneficiaries lost coverage — many of whom likely are working or qualify for an exemption. A far better approach for Arkansas would be to implement a robust voluntary workforce program, which would provide job training and other services to the small group of beneficiaries who aren’t working and can work without causing thousands to lose health insurance.