BEYOND THE NUMBERS
We updated this post on June 14, 2018.
As we’ve said, state Medicaid waivers that take coverage away from people who don’t work or engage in work activities for a set number of hours each month will lead to large coverage losses — even among those who comply with the requirements or should be exempt from them. Arkansas’ approach to implementing its requirements, which took effect on June 1, will make that problem even worse.
That’s because the state is requiring enrollees to demonstrate compliance through a problematic online portal that poses major hardships for enrollees, many of whom don’t have Internet access. Those who don’t comply, or don’t properly report their compliance, with the requirement for three months during the year will lose their coverage.
While many states have created online portals for individuals to apply, renew, or report changes, states have always created them in addition to other access points, giving enrollees multiple ways to interact with state agencies, including phone and in-person access at local eligibility offices. Making the online portal the exclusive means of communication, as Arkansas is doing, presents major challenges for enrollees:
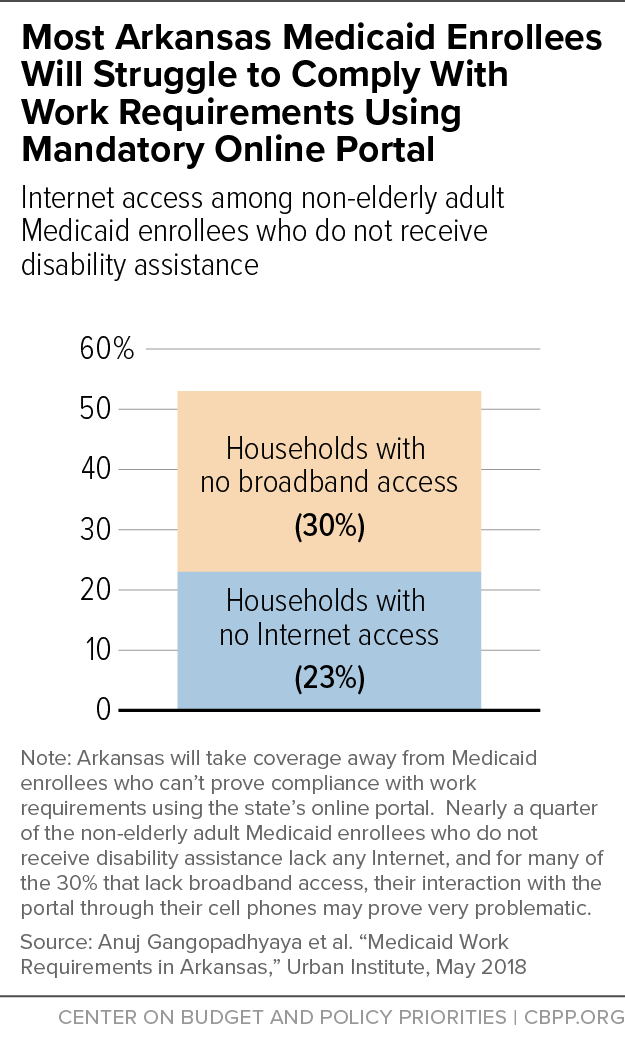
- Many Arkansans lack Internet access. An estimated 23 percent of non-elderly adult Medicaid enrollees who do not receive disability assistance lack Internet access, which means they don’t have access through a cell phone or an Internet service provider. Another 30 percent have no broadband Internet access, which suggests that many of these enrollees access the Internet only through their cell phones. (See chart.) For that 30 percent, the website could prove problematic, per the next bullet.
- The website is not mobile friendly. Google rates the site that enrollees must use to log in to the reporting portal as not mobile friendly, with text that appears too small on mobile devices, content that’s wider than the screen, and clickable elements that are set too close together to effectively use on a mobile device.
- Establishing an account for the website and logging in is difficult. To report compliance through the portal, enrollees must have an email address to log in and must link their account to their Medicaid case. Linking the case requires a reference number that’s found on mailed notices, which enrollees may not have received or have available.
- The website is not accessible for people with disabilities. Although the state claims that its portal complies with the Americans with Disabilities Act, the initial pages that an enrollee must click through to log in contain features that, among other shortcomings, make it hard for visually impaired persons to access. The pages are hard for a screen reader to process and have inadequate contrast, making navigation problematic.
- Enrollees must comply with strict reporting requirements. Enrollees must report work activity compliance for the previous month by the fifth of each month and renew exemptions as frequently as every two months. Even if enrollees can access a public computer with Internet or request assistance from their health plan, they have a narrow window to report.
Only about 4,000 of the first group of 11,000 enrollees subject to the work requirements on June 1 had created accounts as of then.
The state says it spent nearly $7 million to create the website and claims the portal and eligibility system will automatically connect, allowing exemption and compliance data to flow directly into the eligibility system without caseworker intervention. The experience of many states, including Arkansas, however, shows that implementing new complex policies and systems is rarely seamless and often causes eligible people to lose coverage.
The state hasn’t hired additional staff to answer questions or make accommodations for individuals with disabilities. “If you implement [work requirements] in the old-fashioned way of ‘Come into our county office,’” Arkansas Human Services Director Cindy Gillespie said, “we would have to hire so many people — and that just doesn’t make sense.” But by not investing in staff and other resources to support enrollees who should be exempt or need help complying with the requirements, Arkansas is creating a bureaucratic maze that will cause many eligible enrollees to lose coverage.