- Home
- Medicaid Work Requirements Will Harm Fam...
Medicaid Work Requirements Will Harm Families, Including Workers
Recent Trump Administration guidance allows states — for the first time — to take away Medicaid coverage from people who aren’t working or engaged in work-related activities for a specified number of hours each month. The Centers for Medicare & Medicaid Services (CMS) has approved work requirement policies in Kentucky and Indiana, and eight other states are already seeking approval for similar approaches. The new guidance follows unsuccessful attempts by congressional Republicans to allow states to tie Medicaid eligibility to employment as part of bills to “repeal and replace” the Affordable Care Act (ACA).[1]
Medicaid work requirements will cause many low-income adults to lose health coverage. Medicaid work requirements will cause many low-income adults to lose health coverage. They include people who are working or can’t work due to mental illness, serious chronic physical conditions, or opioid addiction or other substance use disorders but who can’t overcome bureaucratic hurdles to document that they meet work requirements or qualify for an exemption. Losing coverage will not only reduce access to care and worsen health outcomes, but likely make it more difficult for many people to find or keep a job.
-
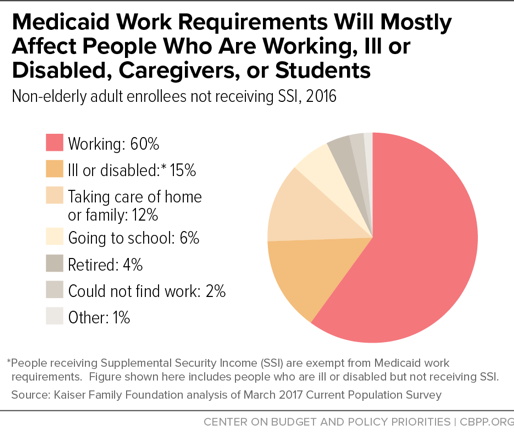
Work requirements will make it harder for most adult beneficiaries — the lion’s share of whom are already working or are ill, disabled, caregivers, or in school — to get and stay covered. Of the roughly 25 million people nationally who could be subject to Medicaid work requirements, 60 percent are already working (see Figure 1). Of the rest, half live in working families, and more than 80 percent are in school or report that they are unable to work due to illness, disability, or caregiving responsibilities. Yet states could require most of these 25 million enrollees to meet burdensome paperwork and documentation requirements to prove that they are working or volunteering sufficient hours each month or qualify for an exemption.
As a result, both working people and people who are supposed to be exempt from work requirements — including those unable to work due to disability or serious ilness — will lose coverage due to state work requirements. Working people may lose coverage for any one of several reasons: their work hours fluctuate from month to month and sometimes fall below required thresholds, they are between jobs but are seeking work, or they don’t successfully navigate the new paperwork requirements and red tape. Similarly, people with disabilities and serious illnesses may lose coverage because they don’t meet the critera for limited exemptions, don’t understand that they do qualify for an exemption, or struggle to provide the documentation proving that they qualify. Bearing out these concerns, studies of state Supplemental Nutrition Assistance Program (SNAP) and Temporary Assistance for Needy Families (TANF) programs have found that people with disabilities, serious illnesses, and substance use disorders may be disproportionately likely to lose benefits due to work requirements, even when they should be exempt.
-
Work requirements are unlikely to promote employment and may be counterproductive. Research on work requirements in other programs finds that they generally have only modest and temporary effects on employment, failing to increase long-term employment or reduce poverty. Results in Medicaid are likely to be just as disappointing and could be worse, since state Medicaid programs generally are not well equipped to provide work support services, which are already oversubscribed in most states, and the Administration guidance prohibits states from using federal Medicaid funding to provide these services. Moreover, health coverage is itself an important work support: having health care helps people work and look for work, and taking it away will likely make it harder for some to keep and find work.
-
The primary effects of work requirements will be less access to care, worse health outcomes, and less financial security. States themselves project significant coverage losses from work requirements, with Kentucky estimating that 15 percent of all adult Medicaid enrollees — at least 97,000 people — will lose coverage due to work requirements and other provisions of its waiver. Studies of both the ACA’s Medicaid expansion find that it increased access to care and improved enrollees’ financial security and health outcomes. For those losing coverage due to work requirements, these gains will be reversed.
This is one reason why major physician organizations — including the American Medical Association, American Academy of Family Physicians, American Academy of Pediatrics, American College of Obstetricians and Gynecologists, American College of Physicians, American Osteopathic Association, and American Psychiatric Association — oppose Medicaid work requirements.
Medicaid Criteria Changes Don’t Ensure Waivers Will Further Program Objectives
Policy Basics
Health
End Notes
[1] Hannah Katch, Jennifer Wagner, and Aviva Aron-Dine, “Medicaid Work Requirements Will Reduce Low-Income Families’ Access to Care and Worsen Health Outcomes,” Center on Budget and Policy Priorities, February 8, 2018, https://www.cbpp.org/research/health/medicaid-work-requirements-will-reduce-low-income-families-access-to-care-and-worsen.
More from the Authors