Taking Away Medicaid for Not Meeting Work Requirements Harms People with Mental Health Conditions
Medicaid is the nation’s largest payer of mental health services, providing health coverage to 26 percent of adults with a serious mental illness, many of whom obtained coverage through the Affordable Care Act’s Medicaid expansion.
Now, however, the Trump Administration is allowing states to take away Medicaid coverage from people who don’t document that they work a specified number of hours each month. This will harm people with mental health conditions, threatening their coverage and access to treatments including medications, therapy, and case management services.
The Administration’s policy requires states to exempt people deemed “medically frail” and recommends exempting those with an acute medical condition that keeps them from working. But many people with mental health conditions likely won’t qualify for an exemption or won’t be able to prove they do. That’s what seems to have happened in Arkansas, the first state to implement such a policy, where the number of people who lost Medicaid coverage exceeded the work requirement’s presumed target population — people who are neither working nor qualify for an exemption. More than 18,000 people in the state lost coverage in 2018 due to the new requirements.
While a federal court has since halted Arkansas’ policy, the Administration is continuing to approve similar policies in other states. Most of these policies require enrollees, other than those who are 65 or older, pregnant, or qualify because they are receiving Supplemental Security Income (SSI), to document that they work or engage in other work activities (e.g., job training or volunteer work) for at least 80 hours per month.
Many People with Mental Health Conditions Won’t Qualify for an Exemption or Will Have Trouble Proving They Do
The definition of “medically frail” is strict and will leave many people with mental health conditions out of the exemption. The definition only explicitly includes individuals with “disabling mental disorders.”
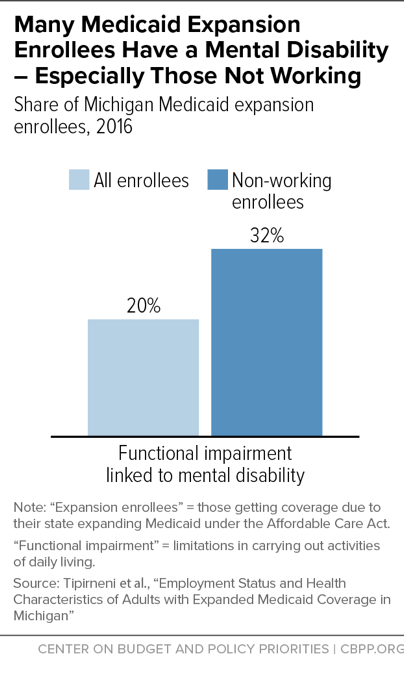
About 14 percent of Arkansas Medicaid beneficiaries who were subject to the work requirement at the end of 2018 qualified as medically frail. But it is likely that many more people have mental health conditions that may affect their ability to work on a consistent basis. For example, nearly 18 percent of Ohio expansion enrollees and 20 percent of Michigan expansion enrollees reported that they had a mental health condition that impaired their ability to function. (See chart.)
Many who qualify for an exemption may have trouble proving it. To prove they are exempt, people with a mental health condition will need to obtain letters from their health care providers, medical records, or whatever documentation a state deems necessary. Red tape and paperwork requirements have been shown to reduce enrollment in Medicaid across the board. Mental illness can interfere with clear thinking and executive function, skills needed to meet documentation and reporting requirements. Some enrollees may be reluctant to disclose their condition and forgo applying for an exemption. Moreover, people with mental health conditions who don’t have coverage will face challenges getting the documentation they need to prove they are exempt if they can’t pay for a doctor’s visit.
People with Mental Health Conditions Face Barriers to Work and Need Additional Supports
While most people with a mental health condition can and want to work, many people face significant barriers to work. Only 17.8 percent of adults with a serious mental illness worked in 2012. The impact of a mental illness on the ability to function often fluctuates, which can lead to inconsistent attendance at work or sudden job loss. People with mental illness disproportionately face other barriers to work such as past involvement with the criminal justice system. And for some, the possibility of losing their health coverage may create additional stress that can exacerbate their condition and makes it more difficult to meet the work requirement. These obstacles can be minimized if people have access to services designed to overcome barriers to employment such as individualized job search assistance, job coaching, and counseling. But the Administration’s guidance on work requirements explicitly states that federal Medicaid funding cannot help pay for these additional supports. Without additional funding, budget-strapped states likely won’t fund necessary supports, making it more likely that people with mental health conditions will be unable to comply.
Medicaid can support work for people with mental health conditions. Instead of implementing punitive policies requiring work, states can use Medicaid to support work through voluntary supported employment services programs. Several states, including Iowa, Mississippi, Wisconsin, and Washington, have implemented supported employment programs for people with mental illness. While each state’s approach differs, all use evidence-based approaches that have helped participants find and maintain employment. They provide an array of services, such as skills assessment, assistance with job search and applications, job development and placement, job training, and negotiation with prospective employers.
Losing Coverage Will Cause Harm to Mental and Physical Health
Medicaid expansion has enabled significant gains in access to treatment for people with mental health conditions. Ten expansion states saw a 44 percent average decline in uninsured mental health stays as of 2014. And in Ohio, 44 percent of Medicaid expansion enrollees who screened positive for depression or anxiety disorders that limited activities like work reported that access to mental health treatment had become easier after enrolling in Medicaid. Work requirements would roll back gains made in access to mental health care. This is why groups like the National Alliance on Mental Illness, the National Council for Behavioral Health, and the Consortium for Citizens with Disabilities oppose Medicaid work requirements.
The Administration largely tries to justify Medicaid work requirements by citing research showing that people with jobs have better health and higher incomes than people without jobs. But that research doesn’t show whether employment causes improved health or rather, as is likely for many people, the causal relationship is in the other direction — namely, that healthy people are likelier to have jobs than those in poor health.
Taking coverage away from people with mental health conditions will threaten not just their mental health. People with mental illness often need health care for physical health conditions in conjunction with treatment for mental illness. People with a serious mental illness have an average life expectancy 25 years shorter than the general population, according to estimates. Taking away their health coverage will delay treatment for both their mental and chronic physical health conditions, such as hypertension, diabetes, and asthma.