Policymakers are paying long-overdue attention to reducing high and increasing rates of deaths and severe health complications among Black people who give birth. Comprehensively addressing this challenge and the broader maternal health crisis requires making a continuum of high-quality health coverage, health care, and other services accessible before, during, and after pregnancy. But the Medicaid “coverage gap” — in which adults with low incomes have no pathway to affordable coverage because their state is one of 12 that has refused to expand Medicaid — puts continuous health coverage out of reach for over 800,000 women of reproductive age. Federal policymakers should close the coverage gap in forthcoming recovery legislation so all women of reproductive age with incomes below the poverty line can get affordable coverage whether they are pregnant or not.
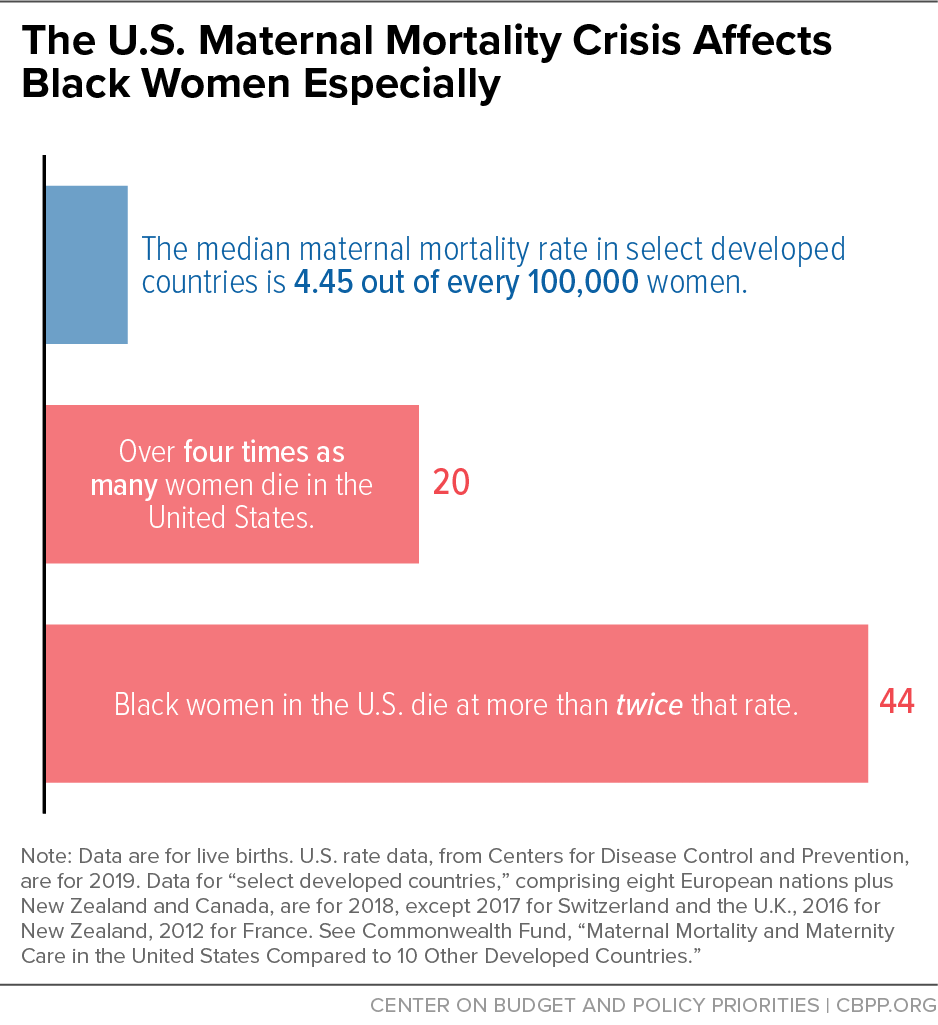
Among developed countries, the United States has the highest rate of people dying of pregnancy-related complications during or within 12 months of the end of pregnancy. And it is getting worse; that rate is higher than it was 25 years ago. Black women are dying at significantly higher rates than other groups, which is linked to factors including structural racism in health care delivery and toxic stress from people’s lived experiences of racism. Black women are also twice as likely to experience severe maternal morbidity: unexpected outcomes of labor and delivery resulting in significant health consequences.
Medicaid pays for more than 40 percent of U.S. births and 65 percent of births to Black mothers, so expanding and enhancing Medicaid coverage must be part of a comprehensive strategy to address the Black maternal health crisis. States that expanded Medicaid under the Affordable Care Act have seen a significant rise in health coverage among women of reproductive age. This has improved their access to preconception and prenatal services that make pregnancy and birth safer for parent and baby. Research also shows Medicaid expansion is associated with reduced rates of maternal death, particularly for Black women.
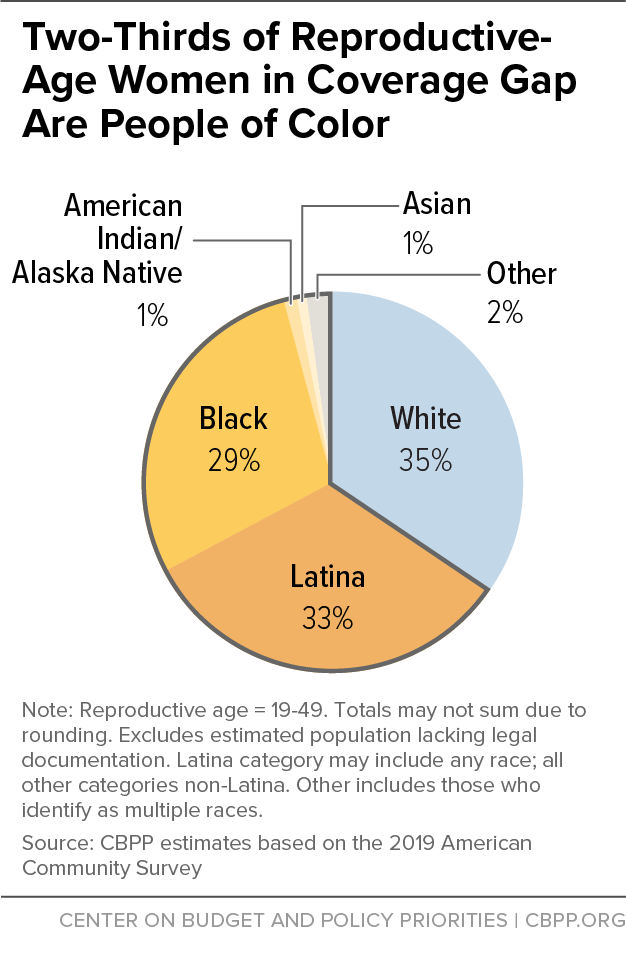
The picture is starkly different in the 12 states that have not expanded Medicaid to cover adults with incomes below 138 percent of the poverty line, or about $17,800 yearly for a single adult. These states have significantly higher uninsured rates for women of reproductive age than do expansion states. In 2019, 810,000 women of reproductive age with incomes below the poverty line — 29 percent are Black and 33 percent Latina — were uninsured without any pathway to affordable health coverage. (See Figure 1.) Almost all lived in the South, where states generally have not expanded Medicaid. (See Appendix Table 1.)
If people in the coverage gap become pregnant, they become eligible for Medicaid. But necessary preconception care is likely unavailable and being uninsured before pregnancy is associated with a higher prevalence of risk factors that contribute to poor pregnancy outcomes, especially for Black women. Moreover, uninsured people may delay prenatal care until they apply for and enroll in Medicaid.
Closing the Medicaid coverage gap is by no means sufficient to address the maternal health crisis. All states should take up the American Rescue Plan’s option to extend Medicaid pregnancy coverage for 12 months after the end of pregnancy instead of the 60 days required under current law. And states should enhance the benefits they provide, including coverage for doulas, who provide support during and after pregnancy. Moreover, numerous bills in the current Congress would invest in health care, nutrition, housing, and transportation and expand the workforce assisting pregnant people, including doulas. The Biden Administration’s budget for the Department of Health and Human Services includes $116 million for its “Improving Maternal Health in America” initiative. Investments like these are necessary to address the many factors behind high rates of maternal mortality and morbidity, especially among Black women.
A history of structural racism, defined as a “system in which public policies, institutional practices, and cultural representations work to perpetuate racial inequity,”a has created greater barriers to health for people of color than for white people. Structural racism is a major factor contributing to people of color’s higher rates of maternal mortality and morbidity, low birthweight and infant mortality, and lower life expectancy. The Medicaid coverage gap, which most heavily affects people of color, is itself evidence of structural racism.
Lasting exposure to adverse experiences, including structural racism, can create toxic stress that increases the likelihood of developing conditions linked to higher rates of maternal and infant death, like hypertension. Moreover, discrimination and implicit bias in the health care delivery system are often expressed in the dismissal of Black women’s concerns and symptoms, which helps explain poor outcomes even for black women with higher income and education.b Black women were ten times more likely to say they were treated unfairly than white women, a survey of women in California showed.c
Structural racism also contributes to income and wealth inequality, which manifests in unequal access to food, transportation, clean air and water, and high-quality education. Public investments and policies play a significant role in shaping the distribution of resources and opportunities to be healthy, so reducing disparities in health outcomes requires directing more resources to the communities that have faced the greatest barriers to health, training providers to address racism, and increasing the diversity of the health care workforce. Policies shape where people can afford to live and whether those places are served by grocery stores with fresh foods, public transit that reduces car dependence, and public parks and recreation spaces that provide safe places to be active.d All these policies, in addition to closing the Medicaid coverage gap, must be addressed to advance health equity.
a Jamila Taylor et al., “Eliminating Racial Disparities in Maternal and Infant Mortality: A Comprehensive Policy Blueprint,” Center for American Progress, May 2019, https://cdn.americanprogress.org/content/uploads/2019/04/30133000/Maternal-Infant-Mortality-report.pdf?_ga=2.58426478.534167243.1625237322-612833220.1620046882.
b Linda Villarosa, “Why America’s Black Mothers and Babies Are in a Life-or-Death Crisis,” New York Times Magazine, April 11, 2018, https://www.nytimes.com/2018/04/11/magazine/black-mothers-babies-death-maternal-mortality.html.
c National Partnership for Women & Families, “Listening to Black Mothers in California,” September 2018, https://www.nationalpartnership.org/our-work/resources/health-care/maternity/listening-to-black-mothers-in-california.pdf.
d Jennifer Sullivan, “Better State Budget, Policy Decisions Can Improve Health,” Center on Budget and Policy Priorities, February 21, 2019, https://www.cbpp.org/research/state-budget-and-tax/better-state-budget-policy-decisions-can-improve-health.
Maternal Mortality and Morbidity: High and Rising
An estimated 700 to 900 women in the United States die each year from pregnancy-related complications. Black women are about three times more likely to die than white women, and American Indian/Alaska Native women are twice as likely.[1] Most of these deaths are preventable.[2]
For every 100,000 live births in 2018, 17 mothers died — more than twice the maternal mortality rate of most other high-income countries.[3] The rate rose to 20 out of every 100,000 live births in 2019, and 44 maternal deaths for Black women. (See Figure 2.) At least 50,000 people a year experience serious complications of pregnancy, and these complications also disproportionately affect Black women.[4] Latina women do not experience deaths at a higher rate, but are at higher risk for severe maternal morbidity.[5] Notably, a college-educated Black mother is at 60 percent greater risk for maternal death than a white or Latina woman with less than a high school education.[6]
There is now consensus among researchers and health care providers that disproportionately high maternal mortality and morbidity among Black women, regardless of income and education, are due to structural racism in the delivery of health care services along with their lived experiences of racism, which leads to toxic stress and elevated risk of conditions such as hypertension.[7]
Cardiovascular conditions including high blood pressure, heart muscle disease, and blood clots are the leading cause of pregnancy-related deaths. Due in significant part to lasting exposure to adverse experiences including structural racism, Black women are at higher risk for these treatable and preventable conditions.[8] (See box, “People of Color’s Higher Maternal Mortality, Morbidity Rates Rooted in Structural Racism.”) Chronic hypertension is associated not only with pregnancy-related deaths and maternal morbidity but also with significant fetal and neonatal morbidity and mortality.[9] (See box, “Mortality Also Higher for Infants of Black Women.”)
While infant mortality rates in the United States have fallen over the past decade, they have fallen at a slower rate among infants of Black women than infants of women of other races.a The infant mortality rate among infants of Black women was 10.75 per 1,000 live births, the highest of any racial/ethnic group and nearly twice the national average of 5.67. Maternal complications, preterm birth and low birthweight are among the key causes of infant mortality. Infants born to Black mothers also have higher rates of low birthweight than any other racial/ethnic group for which data are available.b Low-birthweight babies are more likely to experience serious health complications as infants and are at higher risk for harmful health conditions like heart disease and high blood pressure later in life.
In addition to addressing maternal morbidity and mortality, closing the Medicaid coverage gap would be a down payment on better health outcomes for Black infants and children. More than 70 percent of children in low-income families are enrolled in Medicaid.c Improving access to prenatal and postpartum health care will contribute to better health outcomes for children, especially children enrolled in Medicaid.
a U.S. Department of Health and Human Services, “Health, United States: 2019,” https://www.cdc.gov/nchs/data/hus/hus19-508.pdf.
b National Vital Statistics Reports, “Births: Final Data for 2019,” Centers for Disease Control and Prevention, March 23, 2021, https://www.cdc.gov/nchs/data/nvsr/nvsr70/nvsr70-02-508.pdf.
c State Health Facts, “Health Insurance Coverage of Low Income Children 0-18 (under 200% FPL),” 2019, https://www.kff.org/other/state-indicator/health-insurance-coverage-of-low-income-children-0-18-under-200-fpl/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D.
Racial disparities are significant in the rate of severe maternal morbidity: it was 63 percent higher for women in majority Black and 32 percent higher in majority Latino communities in 2020 than in majority white communities, according to a study of claims for 2.2 million hospital deliveries with a major insurer. The same study found women in majority Black communities have up to twice the prevalence of risk factors such as hypertension or anemia than women in majority white communities. Women in majority Latino communities have prevalence rates up to a third higher for a prior cesarean birth and preexisting diabetes, which are also risk factors for severe maternal morbidity.[10] Having health coverage before and between pregnancies makes it far more likely that these risks get screened for and treated prior to pregnancy, thereby decreasing the risk of poor outcomes.
Medicaid and the Children’s Health Insurance Program (CHIP) pay for more than 40 percent of births in the United States, ranging from a high of 71 percent in New Mexico to a low of 20 percent in Vermont. Medicaid pays for at least 50 percent of births in all states that haven’t expanded Medicaid except for Wisconsin.[11] The share of births that Medicaid finances is higher for Black and Latina women, at 65 percent and 59 percent in 2019, respectively.[12]
Medicaid’s importance in covering pregnant people is especially apparent when looking at how Medicaid coverage of women of reproductive age increases after they become pregnant and decreases afterwards. In 2017, 13.2 percent of women of reproductive age reported being uninsured prior to pregnancy. But the share dropped sharply to 2.6 percent during pregnancy and returned to 10.8 percent after pregnancy. These fluctuations corresponded to increases in Medicaid coverage for this group, which went from 23 percent prior to pregnancy to 35.6 percent during pregnancy and 29.7 percent after.[13]
States must cover pregnant people with incomes up to 133 percent of the poverty line and all but four states cover people with higher incomes, with the 2021 median eligibility level among all states at 200 percent of the poverty line.[14] Pregnancy coverage continues through 60 days postpartum, and the American Rescue Plan Act gives states the option to make postpartum coverage available for 12 months, beginning April 1, 2022.[15] Three states are already providing extended postpartum coverage through demonstrations under Social Security Act section 1115, two states have proposals pending, and 17 have enacted legislation or taken other steps to extend postpartum coverage.[16]
All states should take up the option to extend postpartum coverage, but that doesn’t go far enough. In states that haven’t expanded Medicaid, many people have to wait until they become pregnant to get coverage. States that haven’t expanded generally only cover parents with very low incomes; adults without children generally don’t have any pathway to coverage regardless of their income. The median non-expansion state caps eligibility for parents at about 40 percent of the poverty line, or just $8,800 in annual income for a single parent with two children.[17]
There were just over 800,000 uninsured women of reproductive age in the Medicaid coverage gap in 2019. Most of these women lived in the South, with over 300,000 in Texas alone, and almost two-thirds were people of color (29 percent were Black and 33 percent were Latino).[18] These women could enroll in Medicaid if they become pregnant, but they have no pathway to coverage until they know they are pregnant and apply for and enroll in Medicaid. This leaves them without access to care that could identify and address their health risks before pregnancy and potentially delays the start of prenatal care.[19]
Extending postpartum coverage, as the American Rescue Plan allows states to do, is critically important to reducing maternal mortality and morbidity. That is because about a third of deaths, most of which are preventable, occur between seven and 365 days following delivery.[20] Other Medicaid proposals, such as covering doulas, expanding coverage for home visiting programs that support pregnant people and new parents, and providing evidence-informed services to pregnant people with behavioral health conditions also would contribute to better outcomes for both parents and babies, as would improvements in housing, transportation, nutrition, and environmental conditions.[21] Doulas in particular have been effective in supporting Black women through pregnancy, childbirth, and the postpartum period.[22]
But fully addressing maternal mortality and morbidity, especially for Black women, requires attention to people’s health before and between pregnancies. Having care in these periods allows for identification and treatment of risk factors such as hypertension and diabetes as well as for preconception health care services such as counseling and prescriptions for folic acid, which reduces birth defects. Women who are uninsured before pregnancy are more likely to have these risk factors that are associated with worse outcomes.[23] Moreover, having Medicaid before and between pregnancies ensures access to family planning services and supplies, which all states must cover. Contraceptive use reduces maternal mortality not just in the United States, but around the world, research shows.[24]
Having coverage before pregnancy also eliminates the gap in coverage that occurs between conception and being found eligible for Medicaid based on pregnancy. Nationwide, just 68 percent of people whose births were financed by Medicaid had prenatal care that began in the first trimester.[25]
Overall, Medicaid expansion decreased the uninsured rate for women of reproductive age by 13.2 percentage points, one study estimated.[26] The decrease was much greater, 27.4 percentage points, for women without dependent children who weren’t eligible for Medicaid prior to expansion than it was for parents, some of whom qualified before expansion.
Expansion states also had lower uninsurance rates among women both before and after pregnancy, according to a 43-state study of new mothers who had Medicaid-covered prenatal care between 2015 and 2018. In expansion states, 17.3 percent of new mothers were uninsured prior to conception, less than half the uninsured rate for mothers in non-expansion states (38.1 percent). Within two to six months postpartum, just 10 percent of mothers in expansion states became uninsured compared to 36.1 percent in non-expansion states.[27] Medicaid expansion resulted in a 10.1 percentage-point decrease in churn, defined as moving between different insurance plans or between insurance and uninsurance, according to another study of 19 states and New York City covering 2012 to 2017.[28]
Having coverage makes a difference in the care pregnant people receive. Medicaid expansion was associated with a 22 percent increase in preconception health counseling aimed at addressing risks such as smoking, depression, uncontrolled diabetes, and hypertension before conception. Expansion also led to a 10 percent increase in the proportion of women with low incomes who reported daily folic acid intake in the month before conception. While expansion did not lead to significant changes in indicators related to chronic disease or other health behaviors, researchers noted that the study period of five years after expansion took effect may have been too short to observe detectable changes.[29]
An Oregon study found that expansion, two years after its implementation, increased Medicaid enrollment prior to pregnancy and also increased timely and adequate prenatal care.[30] Medicaid expansion has also been shown to be associated with increased utilization of health care, better self-rated health, and decreased avoidance of health care due to costs among women of reproductive age.[31]
A recent study of maternal mortality from 2006 to 2017 found that while the overall maternal mortality ratio (deaths per 100,000 live births) rose over the period, it was lower in expansion versus non-expansion states. The difference was greatest among Black mothers and was also significant for Hispanic mothers.[32] And in New York, expansion was associated with a statistically significant reduction in severe maternal morbidity among women with low incomes.[33] An editorial accompanying the study notes the importance of preconception care in optimizing women’s health, managing chronic disease, and addressing risk factors for women and their babies.[34]
These studies confirm that coverage will be key to reducing maternal mortality and morbidity for women of color. That coverage must be comprehensive and offer evidence-informed services that are free of discrimination. And it must identify and reduce risks associated with poor pregnancy outcomes for women of color, including those due to toxic stress, poverty, and racism.
| APPENDIX TABLE 1 |
| Uninsured Women of Reproductive Age in the Coverage Gap, by Race/Ethnicity (Southern States) |
| State |
Total |
Black |
Latina |
White |
Other |
| Alabama |
51,000 |
22,000 |
* |
28,000 |
* |
| Florida |
130,000 |
40,000 |
40,000 |
44,000 |
7,000 |
| Georgia |
100,000 |
50,000 |
12,000 |
36,000 |
* |
| Mississippi |
43,000 |
25,000 |
* |
15,000 |
* |
| North Carolina |
73,000 |
24,000 |
8,000 |
36,000 |
* |
| South Carolina |
34,000 |
14,000 |
* |
16,000 |
* |
| Tennessee |
31,000 |
8,000 |
* |
20,000 |
* |
| Texas |
324,000 |
48,000 |
193,000 |
72,000 |
11,000 |