Commentary: At Its 10th Anniversary, the ACA Is Helping to Address Our Public Health and Economic Crisis
End Notes
[1] Sam Stein, “Trump reaffirms that his administration will go forward with lawsuit to end the Affordable Care Act: ‘what we want to do is terminate it’ and replace it with something better,” March 22, 2020, https://twitter.com/samstein/status/1241869302560628738.
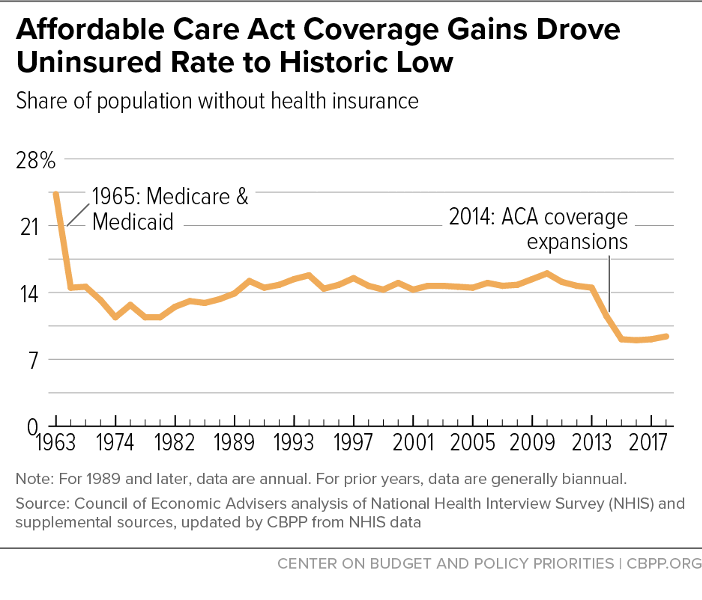
[2] “Chartbook: Accomplishments of Affordable Care Act,” CBPP, March 19, 2019, https://www.cbpp.org/research/health/chart-book-accomplishments-of-affordable-care-act.
[3] Ibid.
[4] Gary Claxton et al., “Pre-Existing Condition Prevalence for Individuals and Families,” Kaiser Family Foundation, October 4, 2019, https://www.kff.org/health-reform/issue-brief/pre-existing-condition-prevalence-for-individuals-and-families.
[5] Wyatt Koma et al., “How Many Adults Are at Risk of Serious Illness If Infected with Coronavirus?” Kaiser Family Foundation, March 17, 2020, https://www.kff.org/global-health-policy/issue-brief/how-many-adults-are-at-risk-of-serious-illness-if-infected-with-coronavirus/.
[6] Matt Broaddus, “ACA Medicaid Expansion Drove Large Drop in Uncompensated Care,” CBPP, November 6, 2019, https://www.cbpp.org/blog/aca-medicaid-expansion-drove-large-drop-in-uncompensated-care.
[7] Richard C. Lindrooth et al., “Understanding the Relationship Between Medicaid Expansions and Hospital Closures,” Health Affairs, January 2018, https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0976.
[8] 2017 Economic Report of the President, “Reforming the Health Care System,” January 2017, p. 283, https://obamawhitehouse.archives.gov/sites/default/files/docs/chapter_4-reforming_health_care_system_2017.pdf.
[9] Leana S. Wen, “The ACA Replacement Would Devastate America’s Health,” STAT, March 22, 2017, https://www.statnews.com/2017/03/22/aca-replacement-public-health/.
[10] Congressional Budget Office, “H.R. 1628, American Health Care Act of 2017,” May 24, 2017, https://www.cbo.gov/system/files/115th-congress-2017-2018/costestimate/hr1628aspassed.pdf.
[11] “Chartbook: Accomplishments of Affordable Care Act.”
[12] Jessica Schubel et al., “The Trump Administration’s Medicaid Block Grant Guidance: Frequently Asked Questions,” CBPP, February 6, 2020, https://www.cbpp.org/research/health/the-trump-administrations-medicaid-block-grant-guidance-frequently-asked-questions.
[13] Jennifer Wagner and Jessica Schubel, “States’ Experiences Confirming Harmful Effects of Medicaid Work Requirements,” CBPP, updated October 22, 2019, https://www.cbpp.org/health/states-experiences-confirming-harmful-effects-of-medicaid-work-requirements.
[14] Tara Straw et al., “Strong Demand Expected for Marketplace Open Enrollment, Despite Administration Actions,” CBPP, October 31, 2018, https://www.cbpp.org/research/health/strong-demand-expected-for-marketplace-open-enrollment-despite-administration; Karen Pollitz, Jennifer Tolbert, and Maria Diaz, “Data Note: Limited Navigator Funding for Federal Marketplace States,” Kaiser Family Foundation, November 13, 2019, https://www.kff.org/private-insurance/issue-brief/data-note-further-reductions-in-navigator-funding-for-federal-marketplace-states/.
[15] Matt Fiedler, “Coverage Gains Among Higher-Income People Suggest the ACA’s Individual Mandate Had Big Effects on Coverage,” Brookings Institution, May 31, 2018, https://www.brookings.edu/blog/usc-brookings-schaeffer-on-health-policy/2018/05/31/new-evidence-the-acas-individual-mandate-substantially-increased-insurance-coverage/.
[16] Sarah Lueck, “Key Flaws of Short-Term Health Plans Pose Risks to Consumers,” CBPP, September 20, 2018, https://www.cbpp.org/research/health/key-flaws-of-short-term-health-plans-pose-risks-to-consumers.
[17] Robert Greenstein, “Trump Administration Rule Will Harm Immigrant Families and Ill-Serve America,” CBPP, August 12, 2019, https://www.cbpp.org/press/statements/trump-administration-rule-will-harm-immigrant-families-and-ill-serve-america.
[18] Rachel Garfield, Kendal Orgera, and Anthony Damico, “The Coverage Gap: Uninsured Poor Adults in States that Do Not Expand Medicaid,” Kaiser Family Foundation, January 14, 2020, https://www.kff.org/medicaid/issue-brief/the-coverage-gap-uninsured-poor-adults-in-states-that-do-not-expand-medicaid/.
[19] Christen Linke Young, “The Trump DOJ has taken an unexpected and unworkable position on the ACA,” Brookings Institution, September 18, 2019, https://www.brookings.edu/blog/usc-brookings-schaeffer-on-health-policy/2019/09/18/the-trump-doj-has-taken-an-unexpected-and-unworkable-position-on-the-aca/.
[20] See, for example: Jonathan H. Adler and Abbe R. Gluck, “What the Lawless Obamacare Ruling Means,” New York Times, December 15, 2018, https://www.nytimes.com/2018/12/15/opinion/obamacare-ruling-unconstitutional-affordable-care-act.html; Dylan Scott, “The new anti-Obamacare lawsuit heads to court today. Scholars think it’s “absurd,” Vox, September 5, 2018, https://www.vox.com/policy-and-politics/2018/6/8/17441512/obamacare-lawsuit-texas-trump; Ilya Somin, “Thoughts on the Trump Administration's Decision Not to Defend Obamacare,” Reason, June 9, 2018, https://reason.com/2018/06/09/thoughts-on-the-trump-administrations-de/.
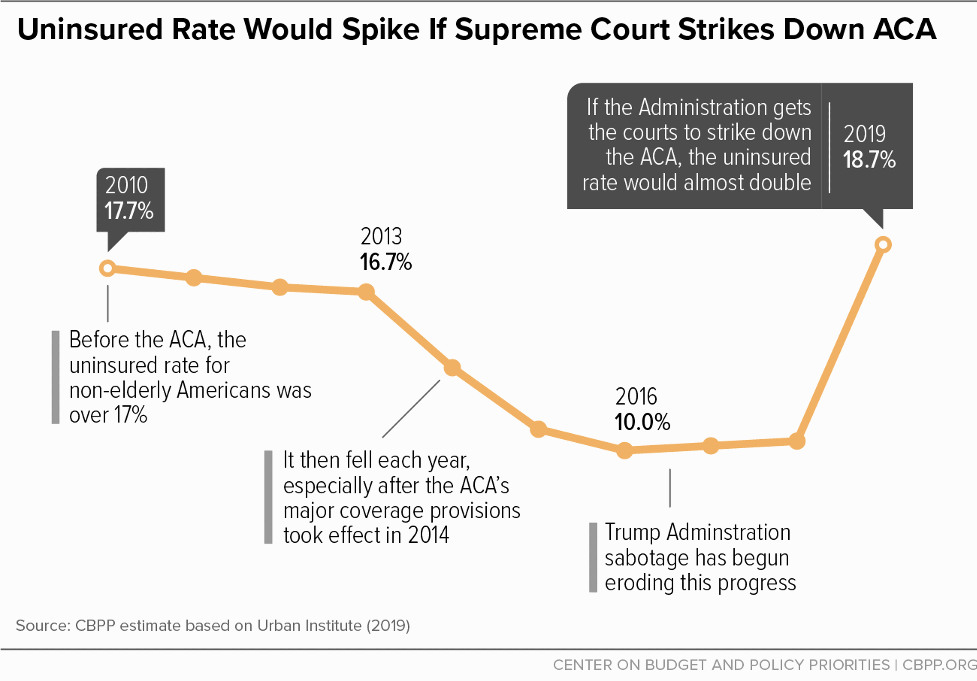
[21] Jessica Banthin et al., “Implications of the Fifth Circuit Court Decision in Texas v. United States,” Urban Institute, December 19, 2019, https://www.urban.org/research/publication/implications-fifth-circuit-court-decision-texas-v-united-states.