BEYOND THE NUMBERS
Republican Bill Vetoed in January Would Have Reversed Almost All of Health Reform’s Coverage Gains
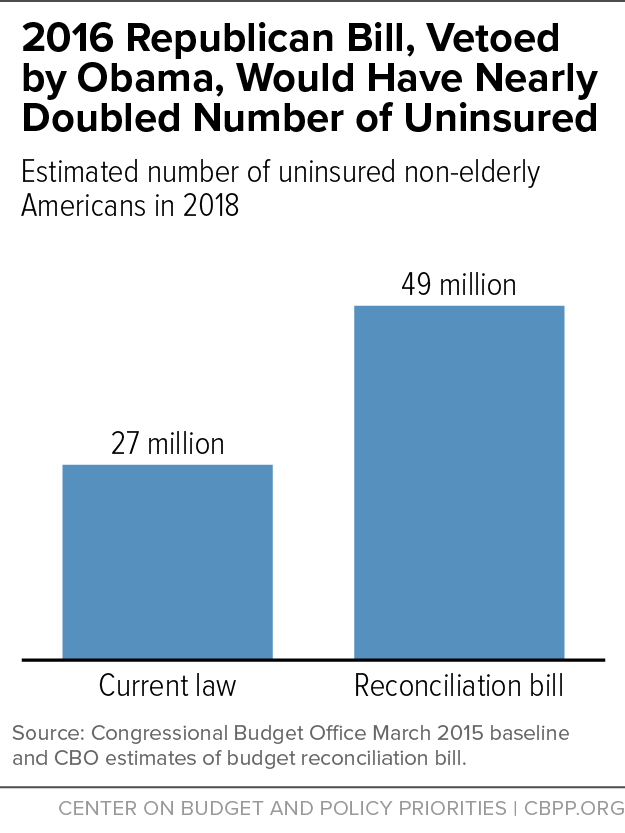
With congressional Republicans reportedly considering using budget reconciliation to repeal the Affordable Care Act early next year, it’s worth taking another look at the reconciliation bill they passed — but President Obama vetoed — last January to undo much of the health reform law. As the Congressional Budget Office (CBO) found at the time, that bill would have raised the number of uninsured Americans by at least 22 million starting in 2018, relative to current law (see chart). Thus, the bill would have reversed at least 92 percent of the historic health coverage gains that CBO expected health reform to achieve by 2018.
Among other things, the bill would have:
- Eliminated health reform’s Medicaid expansion by 2018. That would end health coverage for the millions of low-income individuals who have gained it in the states that have expanded Medicaid and prevent the remaining states from expanding it in the future.
- Eliminated the premium and cost-sharing subsidies that help low- and moderate-income people buy coverage through the health insurance marketplaces, starting in 2018. About 83 percent of the 12.7 million individuals who enrolled in marketplace coverage during the open enrollment period for 2016 qualified for financial assistance.
- Effectively — and immediately —repealed health reform’s requirement, known as the individual mandate, that most individuals must have insurance or pay a penalty, by “zeroing out” the penalty amount. Without the mandate, many fewer people would enroll in job-based coverage, individual market coverage, Medicaid, the Children’s Health Insurance Program, or other sources of coverage.
- Effectively — and immediately — repealed the requirement that employers with more than 50 full-time employees provide affordable, comprehensive coverage to their workers or pay a penalty. As with the individual mandate, the bill would have zeroed out the penalty. Fewer employers would newly offer coverage to their workers and some employers that now provide it would drop it or scale it back so that it’s no longer affordable.
The bill left in place health reform’s market reforms, including those that bar insurers from denying coverage to people with pre-existing health conditions or charging them higher premiums in the individual market. But without the individual mandate and the subsidies to make coverage more affordable, healthier people would likely drop or otherwise go without coverage. Losing most of the healthy people from the risk pool would substantially push up individual market premiums for everyone else, by making those still enrolled sicker and costlier to cover, on average. Higher premiums, in turn, would push even more healthy people out of the pool over time, driving up premiums still further.
As a result, CBO warned that the overall individual insurance market, particularly in smaller states, could entirely destabilize, “leading to very low to no participation by insurers and consumers.” That would lead to even more uninsured people, on top of the 22 million increase that CBO already projected, relative to current law.