BEYOND THE NUMBERS
The Centers for Medicare & Medicaid Services (CMS) has approved New Hampshire’s waiver proposal to take away Medicaid from people not working or engaged in qualifying work activities for 100 hours per month. Under the Obama Administration, CMS rejected a similar proposal from the state in 2016 after concluding that it would “undermine access, efficiency, and quality of care provided to Medicaid beneficiaries.” That earlier assessment was correct: rather than advance Medicaid’s core objectives as waivers are supposed to do, New Hampshire’s will reduce coverage and jeopardize the gains that the state has made since expanding Medicaid coverage to low-income adults under the Affordable Care Act.
All New Hampshire residents aged 19-64 who receive coverage under the state’s Medicaid expansion will have to meet these strict work requirements beginning January 1, 2019 unless they can prove they qualify for exemptions. While New Hampshire did not provide estimates of the waiver’s impact on coverage, states that have done so forecast that Medicaid work requirements will result in large coverage losses.
And New Hampshire’s work requirement is in some ways harsher than those that CMS has approved in Kentucky, Indiana, and Arkansas. For example, its requirement of 100 hours per month of work or work activities exceeds that of other states, which require 80 hours at most. It also provides an exemption only for parents of children under age 6, versus children of all ages in Kentucky and Arkansas.
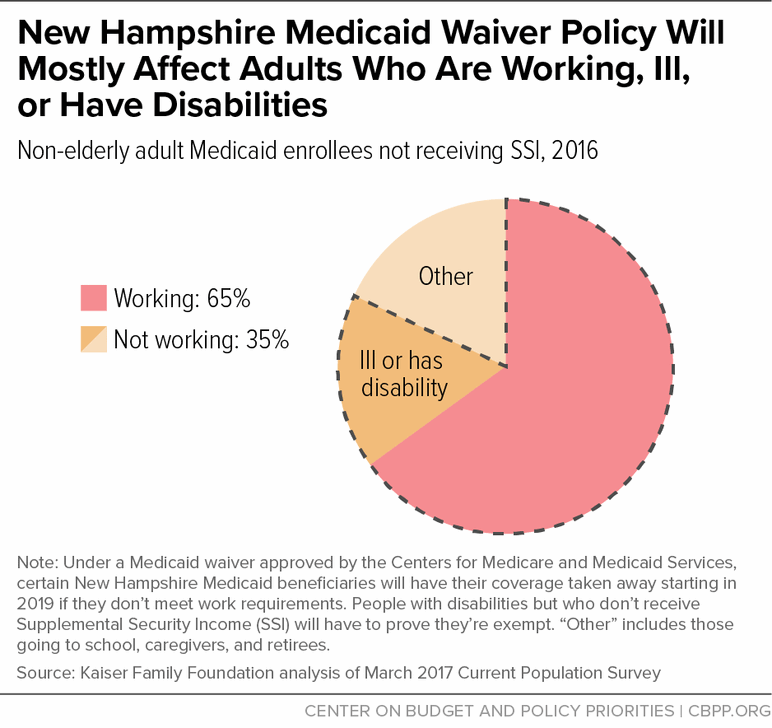
About 65 percent of New Hampshire Medicaid enrollees who could be subject to work requirements already work, and nearly half of those not working are ill or have a disability (see chart). These facts might seem to suggest that the new policy will affect relatively few people but, in reality, many workers and people with serious health needs will likely lose coverage.
While most New Hampshire Medicaid enrollees work, they work in industries like retail, home health, and construction — jobs where hours fluctuate from month to month and there is little flexibility, meaning any illness, family emergency, or disruption in child care or transportation can lead to job loss and a gap in employment. As a result, 46 percent of working low-income adults would be at risk of losing coverage under an 80-hour-per-month work requirement — a lower standard than New Hampshire’s.
Meanwhile, people with disabilities or serious illnesses may lose coverage because they don’t meet the standards to qualify for exemptions, don’t know they qualify, or have a hard time providing the necessary documentation. Red tape and paperwork requirements reduce enrollment in Medicaid, studies show, and people with mental illness or serious physical limitations may have particular difficulty overcoming these barriers.
Children will also likely suffer. New Hampshire provides an exemption from work requirements only for parents of children under age 6, and parents of older children are likely at particular risk of losing coverage if they can’t balance caregiving responsibilities with working 100 hours every month. When parents lose coverage, children get hurt because families lose financial security and parents are less able to take care of their own physical and mental health. Studies have also found that children are likelier to have health coverage when their parents do too, with children gaining both coverage and access to care as states expanded Medicaid coverage for parents.
Since New Hampshire expanded Medicaid, its uninsured rate has fallen by 45 percent, and the share of adults forgoing care due to cost fell by about a quarter. Medicaid is now an important source of coverage for over 52,000 low-income adults in New Hampshire, providing cervical, breast, and colorectal cancer screenings to over 20,000 adults — as well as ensuring access to substance use disorder services to 11,000 adults, which are critical in combatting the opioid epidemic that’s gripping the state. The state’s Medicaid expansion has also helped reduce uncompensated care costs, which have fallen by about half as a share of hospital budgets since the expansion took effect.
With yesterday’s announcement from CMS approving New Hampshire’s waiver proposal, these gains will be in jeopardy. New Hampshire’s harsh work requirement and coverage suspensions will inevitably lead to coverage gaps, reducing access to care and worsening health outcomes for many low-income adults. And, while the New Hampshire House of Representatives just approved an extension of its Medicaid expansion, with a vote pending in the Senate, the bill maintains harsh work requirements similar to those CMS just approved. Extending the state’s Medicaid expansion would help maintain coverage for low-income adults in New Hampshire, but the state’s waiver will mean thousands fewer people with coverage and access to care than if New Hampshire were to maintain its current Medicaid program.