BEYOND THE NUMBERS
The Affordable Care Act’s (ACA) Medicaid expansion has extended health coverage to millions of women, and at least 2.2 million more uninsured women could gain coverage if the 14 states that haven’t yet implemented the expansion did so. That would improve coverage and access to care for people who have recently given birth, likely improving health outcomes, research shows.
Medicaid provides comprehensive health care services including preventive care, family planning, care between pregnancies, and care for chronic physical and behavioral health conditions. The expansion has provided a wide range of essential health care services for women. Before the ACA, many low-income women were ineligible for Medicaid if they weren’t pregnant or disabled or did not have young children, depending on their state’s eligibility criteria. In states that have expanded Medicaid, women with income up to 138 percent of the federal poverty level (about $30,000 for a family of three) can enroll in Medicaid for comprehensive physical and behavioral health services. Medicaid also provides essential pregnancy and postpartum care, family planning, and long-term care services.
Medicaid plays a particularly important role in pregnancy and postpartum health. Medicaid financed 43 percent of all births nationwide in 2018, but pregnancy-related Medicaid coverage ends 60 days after childbirth. Postpartum health coverage is particularly important because life-threatening conditions during and after pregnancy are distressingly common in the United States, and people with low incomes and people of color are disproportionately likely to face these conditions.
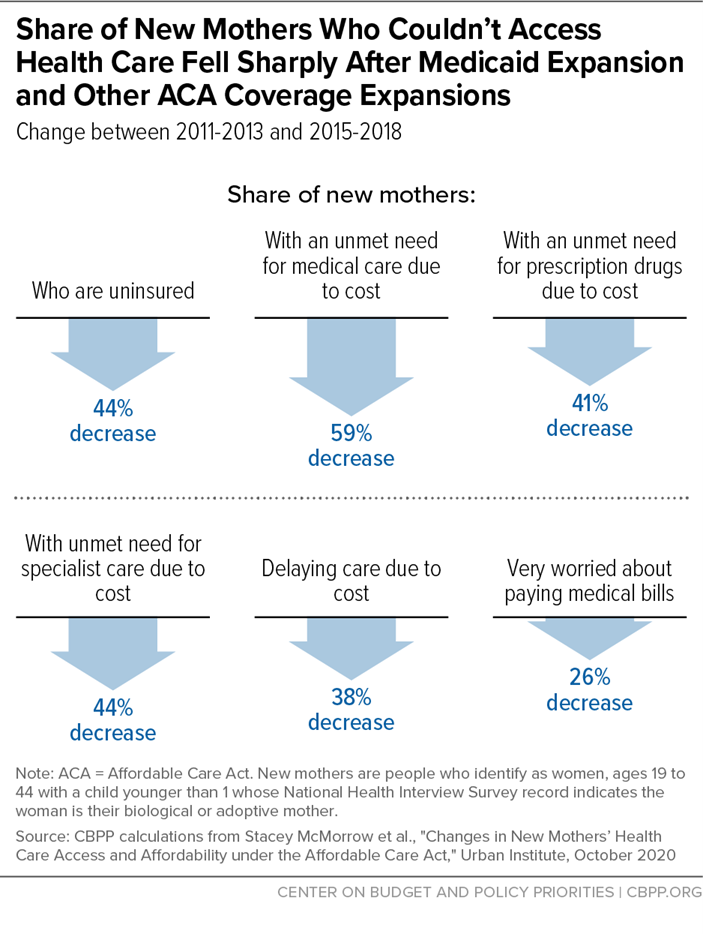
The ACA’s implementation, including the Medicaid expansion beginning in 2014, substantially improved new mothers’ access to care, data suggest. Nationally, the share of new mothers (women with infants under the age of 1) who reported that they have no insurance fell from 20 percent to 11 percent between 2011 and 2015. The share with an unmet medical need due to cost fell by nearly 60 percent (from 6.9 percent in 2011 to 2.8 percent in 2015), according to Urban Institute research. (See graphic.)
Studies focused specifically on postpartum coverage and care likewise find expansion states outperforming non-expansion states. A study comparing pregnancy-related outcomes in Colorado (which expanded Medicaid) versus Utah (which did not) found that among people with severe pregnancy-related health conditions, postpartum visits in Colorado were 50 percent higher than in Utah.
In states that did not expand Medicaid, postpartum people were three times likelier to be uninsured three to six months after childbirth than postpartum parents in states that expanded Medicaid, another study found. People who have recently given birth were also likelier to be continuously enrolled in coverage before, during, and after childbirth in expansion states than in non-expansion states (70 percent versus 56 percent, respectively), the study found. Overall, Medicaid expansion reduced “churn,” which occurs when people lose Medicaid and then re-enroll within a short period of time, among people who had recently given birth by 28 percent, another study found.
The evidence is clear: Medicaid expansion has increased coverage and improved access to care, including postpartum care, for millions of women. Expansion has also reduced individuals’ medical debt and providers’ uncompensated care costs while averting thousands of premature deaths. But 12 states still haven’t adopted the expansion while two others have yet to implement it, leaving millions of people uninsured, even during COVID-19.