BEYOND THE NUMBERS
An expert panel recommends sensible steps to strengthen program integrity in Social Security’s Disability Insurance (DI) and Supplemental Security Income (SSI) programs so that disability benefits go only to eligible people and in the correct amounts. The panel, appointed by the Social Security Advisory Board, has outlined improvements in continuing disability reviews (CDRs) as well as other program-integrity tools in the Social Security Administration’s (SSA’s) kit.
Lawmakers should support SSA’s ability to deploy these proven tools instead of making erroneous charges that disability benefits are easy to get or rife with fraud.
CDRs — regular follow-ups of DI and SSI beneficiaries to weed out those who’ve recovered enough to work — lead to termination of benefits in a minority of cases. About 6 percent of CDRs conducted in 2012 led the agency to stop benefits, though the rate was much lower for adults and higher for children (whose medical conditions tend to be more changeable).
Even with those low termination rates, CDRs more than pay for themselves over time, saving about $10 in benefits for each $1 they cost to conduct, SSA estimates.
The panel suggests boosting CDRs and related efforts by:
- Providing CDR funding that’s adequate, predictable, and sustained. Congress should provide dedicated funding that the agency can count on, so that SSA can train and keep the specialized staff that CDRs require.
- Strengthening other program-integrity tools. Congress also should support the best practices for avoiding erroneous benefit awards in the first place. Such practices include pre-effectuation reviews to ensure that people approved for benefits are still eligible before receiving any payments and expanding Cooperative Disability Investigation units to investigate suspicious claims. SSA needs full and predictable funding for program integrity as a whole, not just for CDRs.
- Strengthening implementation of the medical improvement review standard (MIRS). This standard, which Congress enacted unanimously in 1984 in response to the Reagan Administration’s abuse of CDRs to terminate large numbers of DI and SSI beneficiaries, requires SSA to find that a beneficiary’s condition has actually improved before stopping benefits. The panel regards the standard as an essential safeguard but urges SSA to better train staff on how to evaluate the narrow circumstances in which it doesn’t apply, such as when a beneficiary refuses to cooperate with the CDR or has been helped dramatically by rehabilitation or technological advance.
- Doing more to help beneficiaries prepare for, and adjust to, the loss of benefits once they are no longer eligible. The panel suggests that Congress extend beneficiaries’ eligibility for rehabilitation and employment support services for a year after their benefits end. It also urges SSA to communicate work expectations clearly for beneficiaries most likely to recover so they’re not caught off-guard by their CDR. That’s especially important for youths turning 18, many of whom lose SSI benefits only to struggle in adulthood.
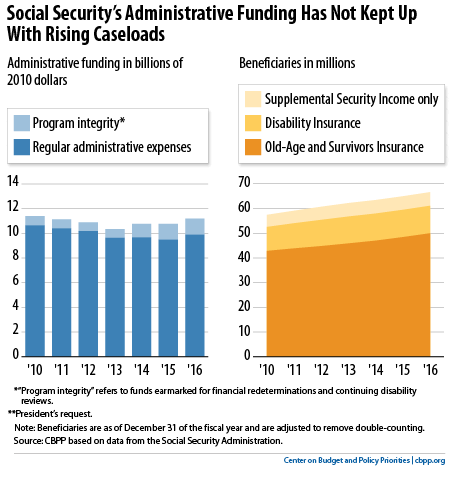
Funding is key, as the panel’s report makes clear. SSA’s administrative budget hasn’t kept up with its workload (see graph), and until recently Congress failed even to provide all of the money for CDRs that the 2011 Budget Control Act explicitly permitted.
President Obama’s 2016 budget proposes to address that by providing a reliable stream of money (not subject to annual appropriation) for doing CDRs as well as financial redeterminations in SSI. Even closer to the panel’s recommendations, Representative Xavier Becerra (D-CA) has introduced a bill to not only guarantee funding for CDRs and redeterminations but also enable SSA to beef up quality reviews before award, detect and prosecute fraud, and recover overpayments. Such reforms could be included in needed legislation to replenish the DI trust fund.
