BEYOND THE NUMBERS
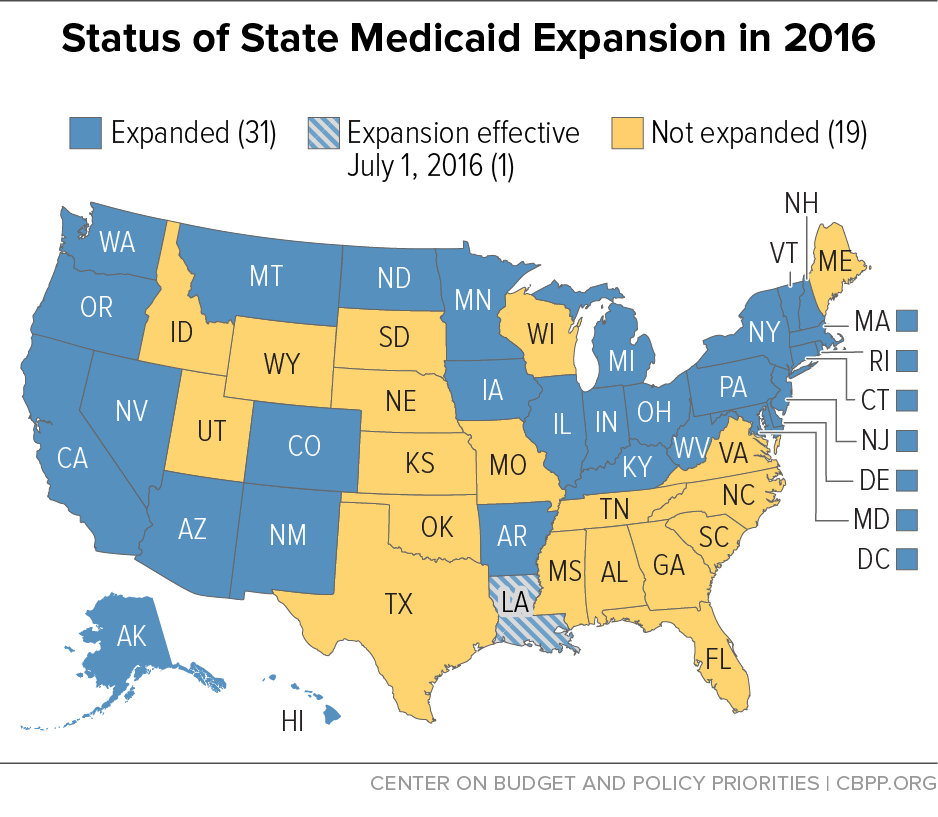
Louisiana’s new governor, John Bel Edwards, signed an executive order today to expand Medicaid as part of health reform, effective July 1. That will make 292,000 uninsured, low-income Louisianans eligible for Medicaid coverage, according to estimates from the Kaiser Family Foundation.
Louisiana has long had some of the nation’s lowest Medicaid eligibility levels for adults: currently, a parent of a dependent child is eligible for Medicaid only if he or she earns less than 24 percent of the federal poverty line, or $4,800 a year for a family of three. And non-elderly non-disabled adults without dependent children aren’t eligible at all. That has created a “coverage gap” in Louisiana and other non-expansion states in which poor individuals with income too high for Medicaid but too low for federal subsidies to purchase coverage in health reform’s marketplaces remain without health insurance.
By adopting the expansion, which raises Medicaid eligibility for non-elderly non-disabled adults to 138 percent of the poverty line, Louisiana will provide for the first time a pathway to affordable health coverage for many of its low-income residents.
For a preview of how expansion will likely benefit Louisiana, one can look to the recent experiences of the three Southern states that have already expanded: Arkansas, Kentucky, and West Virginia. Like Louisiana, these states had high rates of uninsurance and low Medicaid eligibility levels for adults before health reform. But after taking up the expansion, Arkansas’ uninsurance rate among adults fell from 22.5 percent to 9.1 percent between 2013 and the first half of 2015, the largest percentage-point drop in the country. Over the same time period, Kentucky’s uninsured rate fell from 20.4 percent to 9 percent and West Virginia’s fell from 17.6 percent to 8.3 percent (the second- and seventh-largest drops nationwide, respectively).
Medicaid expansion has also produced net savings for many state budgets, with Arkansas, Kentucky, and West Virginia garnering some of the largest savings. Expansion can save states money because it allows them to move people who previously received health services through targeted Medicaid programs — such as family planning services and care for certain women with breast and cervical cancers — which are financed at the state’s regular Medicaid matching rate, into the new expansion group for which the federal government is now paying the entire cost (and no less than 90 percent on a permanent basis). Moreover, as more people gain coverage, demand for health services for uninsured low-income people that states fund entirely, such as funding for hospitals to help with uncompensated care costs, declines.
Three million uninsured adults are caught in the coverage gap in the states that haven’t yet expanded; 90 percent of them live in the South. Louisiana’s decision to expand will lower this number. Other states — particularly those in the South — should follow suit.