BEYOND THE NUMBERS
Most emergency room (ER) physicians report seeing more patients since health reform’s major coverage expansions took effect in 2014, a recent survey found. Critics say this shows that health reform’s coverage expansions — particularly its Medicaid expansion — aren’t providing access to needed care or reducing ER use for care that people could receive in less costly settings. The reality, though, is more complex.
First, the survey results come with substantial caveats. Only 9 percent of surveyed physicians responded, and the questions — about events over a period of more than a year — would likely be better answered by a hospital administrator. Also, the survey didn’t distinguish between ER visits for non-urgent care that could be provided elsewhere and those for emergencies or at times when doctors’ offices weren’t open.
The best research available — on Oregon’s 2008 Medicaid expansion to low-income adults — suggests that when people get health coverage, they use more primary care, hospital care, and ER care. That makes sense. Coverage improves access to care, and people need care in each of these settings at different times. For emergency care, analysts found that Medicaid beneficiaries averaged 1.43 ER visits over 18 months, compared with 1.02 visits for otherwise similar low-income adults who were uninsured.
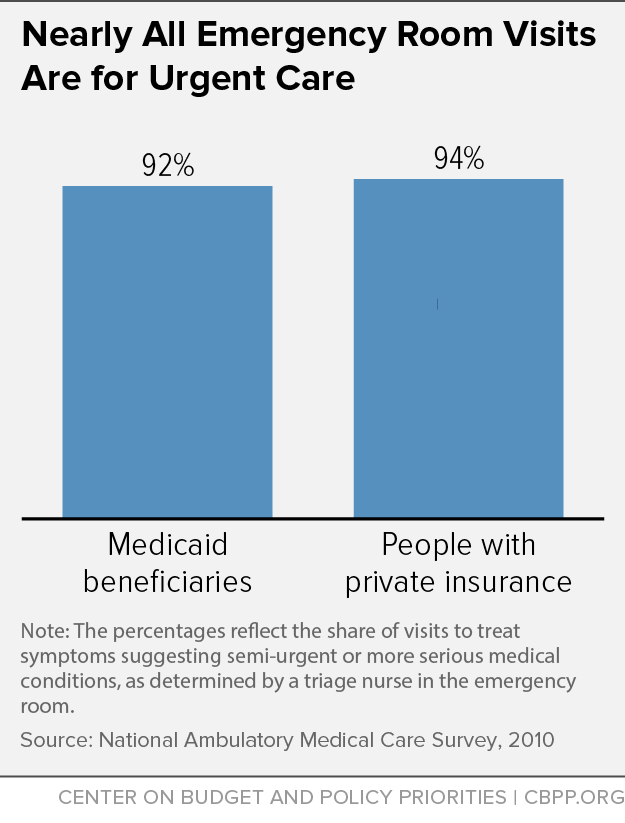
Only a small share of ER visits for people with insurance are for non-urgent conditions to begin with: 8 percent among Medicaid beneficiaries and 6 percent among those with private insurance, research shows (see graph). Most ER visits are at night or on the weekend, when doctors’ offices typically are closed: 75 percent for children with Medicaid and 71 percent for children with private coverage.
Although ERs treat relatively few non-urgent cases, state Medicaid programs are working to further reduce ER visits for non-urgent care. Washington, for example, developed seven best practices to reduce non-urgent ER care in Medicaid, including providing education materials to beneficiaries, re-directing care to the most appropriate setting, and identifying frequent ER users. In just one year the state cut non-urgent ER visits by 14 percent, saving more than $30 million.
This CBPP paper identifies several other initiatives in which states are using their flexibility in Medicaid to provide health care services more effectively and efficiently.