Unwinding Watch: Tracking Medicaid Coverage as Pandemic Protections End
Our “Unwinding Watch” highlights key developments as states resume determinations on people’s Medicaid eligibility. Previously, the pandemic-related “continuous coverage” requirement safeguarded this coverage for millions of people.
As of April 1, 2023, states may begin ending coverage for people found ineligible or whose redetermination can’t be completed for procedural reasons. Start dates for this so-called “unwinding” process vary by state and states will take different amounts of time to redetermine their full caseloads.
States and consumer advocates prepared for unwinding , but coverage losses are growing, even among people still eligible. Unwinding Watch highlights key data and policy developments across the country.
For more information, see our “End of the Pandemic-Era Medicaid Continuous Coverage Requirement” resource page.
March 28 The Centers for Medicare & Medicaid Services (CMS) released monthly unwinding data, including December unwinding renewal outcomes and operations data as well as preliminary January unwinding outcomes data.
Once again, the good news relates to the rate of ex parte renewals (using data sources to confirm ongoing eligibility without requiring action from the enrollee). The preliminary January data show an ex parte rate of nearly 46 percent, similar to December’s rate. The rate is about double what it was at the beginning of the unwinding, and two consecutive months at similarly high rates indicate the progress is sustainable. Nineteen states reported an ex parte rate of greater than 50 percent. Much of this improvement is attributed to work the U.S. Digital Services (USDS) did in partnership with CMS to provide direct support to states to improve their ex parte processes, which was also highlighted in a press release and case study released by CMS.
The bad news, unfortunately, continues to be that states are still greatly struggling to handle the volume of work from renewals and applications (many of which are re-applications from people procedurally denied at their renewal). In December, seven states took more than the federally mandated deadline of 45 days to process 30 percent or more of their MAGI applications. Many states have declining timeliness numbers, including the two states with the highest rates of untimely applications: Missouri (57 percent untimely) and New Mexico (61 percent untimely).
Delays in processing applications — especially the extreme and worsening delays we are seeing in many states — cause hardship both to people newly seeking coverage as well as those who lost coverage during their renewal despite remaining eligible and now must reapply and wait for their application to be approved. They also indicate states are having difficulty with customer service overall and are often associated with long call center wait times, lost documents, and inaccurate determinations.
March 28 The Centers for Medicare & Medicaid Services (CMS) announced plans to extend the end date of the “unwinding Special Enrollment Period” (SEP) from July 31 to November 30, 2024 in states that use HealthCare.gov. In January 2023, CMS created that SEP for anyone losing Medicaid or Children’s Health Insurance Program (CHIP) coverage between March 31, 2023 and July 31, 2024 to help them avoid gaps in health coverage during unwinding. The extension will allow people losing Medicaid/CHIP, especially people in states that are taking longer than expected to complete the unwinding process, to make a smoother transition to marketplace coverage. The new November 30 deadline overlaps with the November 1 start of marketplace open enrollment, which could help eliminate a gap in coverage for people who have lost their Medicaid coverage and are seeking marketplace coverage to start before January 1, 2025.
The unwinding SEP is now available to anyone who lost or will lose Medicaid or CHIP coverage at any time between March 31, 2023 and November 30, 2024. People can access the SEP by submitting (or updating) an application on HealthCare.gov and answering "yes" to the question whether their Medicaid/CHIP recently ended or will soon end and attesting that their coverage ended/will end between March 31, 2023 and November 30, 2024. People then have 60 days after being determined eligible for the marketplace to select a plan and pay their first month’s premium. States that operate their own marketplaces control their own SEP policies and can adopt similar extensions.
The extended SEP was announced alongside other actions that CMS has recently taken to help people stay covered during Medicaid and CHIP renewals, including guidance on prohibited practices during renewals; updated guidance to Medicaid managed care plans on completing signatures for enrollees; and guidance to help stakeholders navigate Medicaid fair hearings. CMS also released updated unwinding data, which we will cover in an upcoming Unwinding Watch entry.
March 27 The Centers for Medicare & Medicaid Services (CMS) released its long-anticipated Medicaid eligibility and enrollment final rule. First proposed in September 2022, and building on regulations that were issued after the passage of the Affordable Care Act to streamline access to coverage, the rule codifies many important policies that will simplify the process for eligible people, including older adults and people with disabilities (non-MAGI enrollees), children, and pregnant people to get and stay enrolled in Medicaid and the Children’s Health Insurance Program (CHIP).
The final rule comes as unwinding has generated an increased awareness that eligibility and enrollment policies can prevent people who meet Medicaid and CHIP eligibility criteria from enrolling or keeping their coverage. Once fully implemented, the changes the rule makes to increase reliance on electronic data sources (including to verify financial resources for non-MAGI groups as well as both citizenship and identity) and to minimize burdensome and time-consuming documentation processes will help streamline the eligibility process, keep eligible people enrolled, and reduce administrative burdens for states and enrollees.
Key changes in the rule include:
- Streamlined non-MAGI enrollment and renewal policies. Older adults and people with disabilities are known as non-MAGI enrollees because their eligibility is not determined based on the “modified adjusted gross income,” or MAGI, standard used for other enrollees. The final rule aligns non-MAGI policies with MAGI requirements, including prohibiting interview requirements, limiting renewals to once a year, requiring use of pre-populated renewal forms, and requiring a 90-day reconsideration period to re-enroll without a full application if an individual’s coverage has been terminated for procedural reasons.
- Improvements to CHIP enrollment processes. The final rule prohibits lock-out periods after failure to pay CHIP premiums, eliminates waiting periods to enroll in CHIP after becoming uninsured, and prohibits lifetime or annual limits to receiving CHIP coverage. It also requires all states to establish processes to improve transitions between Medicaid and CHIP to reduce the risk of coverage losses when enrollees appear to be eligible for the other program.
- Policies that promote coverage and retention for all Medicaid enrollees. The final rule requires states to implement a multi-step process to reach all individuals whose mail comes back as returned, including a check of reliable data sources for updated contact information, and conducting outreach through multiple modalities such as text and email. To help ensure that people have adequate time to respond to agency requests for additional information, the rule also sets minimum timeframes of at least 15 days for individuals to provide additional information requested by the agency at initial application, and 30 days when renewing coverage. It also eliminates the requirement to apply for other benefits as a condition of Medicaid eligibility, a burdensome policy that can delay Medicaid enrollment for eligible people.
- Improved program integrity measures. In addition to advancing state reliance on data sources in making eligibility determinations, the rule updates outdated recordkeeping rules to define the types of eligibility determination documentation states must retain and requires states to retain records for three years. The rule also requires that states make such records available to federal and state auditors within 30 days of a request. Finally, the rule will advance program integrity by promoting proper and efficient administration of Medicaid and CHIP. As the rule recognizes, program integrity goes beyond ensuring that Medicaid is not covering ineligible people to properly encompass whether individuals who are eligible for coverage receive it.
The rule will be published in the Federal Register on Tuesday, April 2 and will be effective 60 days after publication, or June 3, 2024. States must come into compliance with some provisions by that date, but many provisions have compliance dates ranging from 12 to 36 months after the effective date. These later compliance dates give states time to “phase into” compliance, particularly for changes that require more extensive operational or systems changes.
CMS anticipates that the rule will reduce administrative burdens for states and enrollees, but the delayed compliance dates give states valuable time to make these changes while they continue both unwinding and addressing gaps in compliance with existing policies that have come to light during unwinding.
March 15 The Centers for Medicare & Medicaid Services (CMS) released a set of resources aimed at clarifying and reminding states of federal Medicaid and Children’s Health Insurance Program (CHIP) renewal requirements based on questions they have received from state Medicaid agencies and other stakeholders throughout the unwinding process. Resources CMS shared include:
- A Center for Medicaid and CHIP Services Informational Bulletin (CIB) detailing ten important Medicaid and CHIP renewal requirements and state renewal actions that are not permitted under federal regulations, such as not determining eligibility on all bases before terminating someone’s coverage or giving enrollees less than 30 days to respond to a renewal form before terminating their coverage. The CIB “strongly encourages” states to review their current renewal processes to ensure they are in full compliance with federal requirements, and to reach out to CMS if they identify any areas of potential non-compliance.
- A slide deck with ten example scenarios based on the renewal requirements highlighted in the CIB that state agencies may encounter related to Medicaid and CHIP renewals and how states should approach them. The examples include state actions not permitted by federal regulations, actions that states must do in response to the scenarios, and strategies for state agencies to consider.
March 12 The National Health Law Program (NHeLP) filed complaints in Washington, D.C. and Texas alleging that state Medicaid redetermination processes violate the Americans with Disabilities Act (ADA); NHeLP filed the complaints along with Disability Rights DC at University Legal Services (DRDC) and Disability Rights Texas (DRTx), respectively.
The complaints, filed with the Department of Justice and the Health and Human Services Office for Civil Rights, state that unwinding processes in D.C. and Texas fail to provide equal coverage access, do not meet inclusivity obligations, and have resulted in unnecessary barriers and improper procedural terminations for people with disabilities.
For example, NHeLP and DRDC explain that D.C. creates additional burdens by requiring long-term care enrollees to be assisted by “unreliable” case managers, rather than allowing enrollees to renew their coverage independently or with the assistance of their choosing. In Texas, NHeLP and DRTx allege that the state’s call center regularly provides incorrect information to home- and community-based service enrollees with disabilities. The complaints also point out that both states have failed to use existing information to process renewals.
Advocates request various forms of relief, including that the federal government order D.C. and Texas to stop their redetermination processes and reevaluate members of affected populations whose coverage was terminated after April 2023.
These complaints follow similar allegations filed by NHeLP and the Colorado Center on Law and Policy in February 2024, which alleged that changes to Colorado’s long-term services and supports case management procedures and software violated the ADA by contributing to improper coverage terminations and other access issues for enrollees with disabilities.
March 5 In a letter to Centers for Medicare & Medicaid Services (CMS) Administrator Chiquita Brooks-LaSure, Senate Finance Committee Chair Ron Wyden and House Energy and Commerce Committee Ranking Member Frank Pallone requested information on how the agency is helping states correct the unwinding-related eligibility and enrollment issues in Medicaid and the Children’s Health Insurance Program (CHIP) that are leaving millions without coverage.
The letter noted that unwinding has revealed states’ various shortcomings in implementing and complying with eligibility, enrollment, and renewal requirements that are designed to create a seamless system of coverage. The letter identifies areas of noncompliance, including failures to process applications in a timely manner and to automatically renew eligibility even when a state has the data needed to do so.
Wyden and Pallone express their support for CMS’s efforts to address these “significant deficiencies,” which have included requiring state agencies to utilize temporary mitigation plans and encouraging the uptake of several additional strategies to promote coverage. But they also voice concerns that state Medicaid programs’ shortcomings will continue without further action.
Therefore, they urge CMS to require that all states “commit to a specific and detailed plan to adopt sustainable, long-term systems fixes,” and they request that CMS make these plans public. They also request that CMS continue to require and publish states’ monthly submissions of eligibility and enrollment operations data, which is currently required under the Consolidated Appropriations Act, 2023, but ends after this year’s June renewals.
The letter concludes with a request that CMS provide more detail on:
- the agency’s plans and timeline to ensure that all states come into compliance with federal eligibility and enrollment requirements;
- whether it is prioritizing particular areas of noncompliance;
- how it will monitor compliance and what remedies it will pursue if a state does not come into compliance in a timely manner; and
- whether CMS needs particular tools or resources to effectively oversee and monitor compliance.
Wyden and Pallone requested a response to these questions by March 29, 2024.
February 29 The Centers for Medicare & Medicaid Services (CMS) released monthly unwinding data, including November unwinding renewal outcomes and operations data as well as preliminary December unwinding outcomes data.
As in previous months, the data include a combination of good news and bad news.
Once again, rising ex parte rates are a bright spot in the data. The percentage of renewals completed ex parte (using data sources to confirm ongoing eligibility without requiring action from the enrollee) is beginning to increase more rapidly as states implement unwinding waivers and prioritize addressing deficiencies in their ex parte systems in response to CMS guidance. Final November data shows that 36 percent of all renewals due were renewed ex parte, which is consistent with numbers throughout the fall. The preliminary December data show a big jump — to 47 percent nationwide (CBPP calculation based on preliminary state-by-state data released by CMS). Eighteen states reported an ex parte rate of greater than 50 percent, while only four states reported a rate of 10 percent or less.
The continuing bad news, though, is that many states are continuing to struggle with processing applications in a timely way, as federal regulations require. Federal law sets a 45-day deadline for processing applications for parents, caretakers, children, and expansion adults. (These groups are often referred to as the “MAGI” population because their eligibility is based on a technical income standard called “modified adjusted gross income.”)
According to the final November operational data, 14 states are processing more than 10 percent of their MAGI applications beyond the deadline. Some states missed the mark on 40 percent or more of their applications: the District of Columbia (42 percent); Georgia (40 percent), Missouri (42 percent), and New Mexico (59 percent) are particular outliers. These application processing delays cause hardship both to people newly seeking coverage as well as those who lost coverage during their renewal despite remaining eligible and now must reapply and wait for their application to be approved.
CMS’s marketplace Medicaid unwinding report shows that some people losing Medicaid are finding their way to marketplace coverage; others who lost coverage for purely procedural reasons are likely reapplying for Medicaid or may remain uninsured.
January 31 The Centers for Medicare & Medicaid Services (CMS) released monthly unwinding data, including October unwinding renewal outcomes and operations data as well as preliminary November unwinding outcomes data.
First, the good news. The percentage of renewals completed ex parte (using data sources to confirm ongoing eligibility without requiring action from the enrollee) has continued to increase. In October, 38 percent of all renewals due were renewed ex parte, a substantial increase over the June rate of 29 percent. Fourteen states reported an ex parte rate of greater than 50 percent, while only three states reported a rate of 10 percent or less.
The bad news, though, is that some states continue to struggle to keep up with the volume of work they are facing. Call center wait times remain high in a number of states, with nine states reporting an average wait time over 20 minutes. And most states have seen a substantial increase in application volume during unwinding, with many states reporting more than twice the application volume from before unwinding began. This suggests that many of the people losing coverage at renewal for procedural reasons are in fact still eligible and reapply, causing hardship for the enrollee as well as additional work for overwhelmed agencies.
Most significantly, though, many states are struggling to process applications in a timely way, as federal regulations require. Federal law sets a 45-day deadline for processing applications for parents, caretakers, children, and expansion adults. (These groups are often referred to as the “MAGI” population because their eligibility is based on a technical income standard called “modified adjusted gross income.”)
Fifteen states are processing more than 10 percent of their MAGI applications beyond the deadline, with some states missing the mark on 40 percent more of their applications (see table below). These delays cause hardship both to people newly seeking coverage as well as those who lost coverage during their renewal despite remaining eligible and now must reapply and wait for their application to be approved.
| Many States Struggling to Meet Deadlines for Processing Applications | |
|---|---|
| State | Share of MAGI Applications Not Processed Within 45 Days |
| Alabama | 1% |
| Alaska | 37% |
| Arizona | 2% |
| Arkansas | 8% |
| California | 13% |
| Colorado | 3% |
| Connecticut | 0% |
| Delaware | 0% |
| District of Columbia | 38% |
| Florida | 7% |
| Georgia | 40% |
| Hawai’i | 5% |
| Idaho | 2% |
| Illinois | 11% |
| Indiana | 3% |
| Iowa | 6% |
| Kansas | 22% |
| Kentucky | 0% |
| Louisiana | 7% |
| Maine | 7% |
| Maryland | 0% |
| Massachusetts | 0% |
| Michigan | 3% |
| Minnesota | 0% |
| Mississippi | 18% |
| Missouri | 34% |
| Montana | 31% |
| Nebraska | 9% |
| Nevada | 1% |
| New Hampshire | 6% |
| New Jersey | 27% |
| New Mexico | 45% |
| New York | 0% |
| North Carolina | 5% |
| North Dakota | 9% |
| Ohio | 14% |
| Oklahoma | 0% |
| Oregon | 0% |
| Pennsylvania | 1% |
| Rhode Island | 6% |
| South Carolina | 8% |
| South Dakota | 2% |
| Tennessee | 4% |
| Texas | 32% |
| Utah | 3% |
| Vermont | 9% |
| Virginia | 19% |
| Washington | 4% |
| West Virginia | 15% |
| Wisconsin | 1% |
| Wyoming | 8% |
December 28 The Centers for Medicare & Medicaid Services (CMS) released monthly unwinding data, including September unwinding renewal outcomes and operations data as well as preliminary October unwinding outcomes data. The preliminary October outcomes data continue to reflect the initial impact of CMS’ direction to states to pause procedural terminations if they were conducting ex parte terminations on a household, rather than individual, basis.
The CMS-posted data continue to lag real-time state reporting, which is captured by KFF and the Georgetown Center for Children and Families (CCF) trackers.
Among the key takeaways from the data:
- 22.9 percent of all enrollees due for renewal in September had their Medicaid eligibility terminated, and procedural terminations accounted for 64.8 percent of total terminations, down slightly from August. Twenty-two states and the District of Columbia paused some or all procedural terminations in September due to issues identified in previous months. This number is nearly double the number of states that paused procedural terminations in August and at least partly explains the reduction in procedural terminations nationwide.
- 23.3 percent of cases due for renewal were still pending at the end of September, slightly up from 22.2 percent in August. As we’ve noted before, backlogs in some states could reflect operational capacity challenges, while others could indicate that states have paused procedural terminations to address identified issues and to avoid improperly terminating eligibility for more people.
- The average ex parte renewal rate in September was 33.7 percent, which is again slightly higher than the previous month. Overall, while the nationwide ex parte renewal rate is still low, it continues to slowly tick up.
- The release also includes information about people with previous Medicaid or Children’s Health Insurance Program enrollment who applied for coverage through the Affordable Care Act marketplaces or had their information transferred from Medicaid to the marketplace. As in prior months, the December-released Medicaid-to-marketplace transition data suggest that many people who have lost Medicaid face barriers to enrolling in marketplace coverage.
Coupled with large renewal backlogs, the September operations data include concerning metrics on application processing times with many states routinely exceeding the 45-day maximum allowable timeframe. The September operations data also indicate major challenges for people seeking assistance applying for or renewing coverage over the phone. Call center average wait times were 20 minutes or higher in 15 states, which is a larger share of states than last month and suggests that as backlogs grow and more people need assistance connecting to coverage, state call centers are having difficulty keeping up with demand.
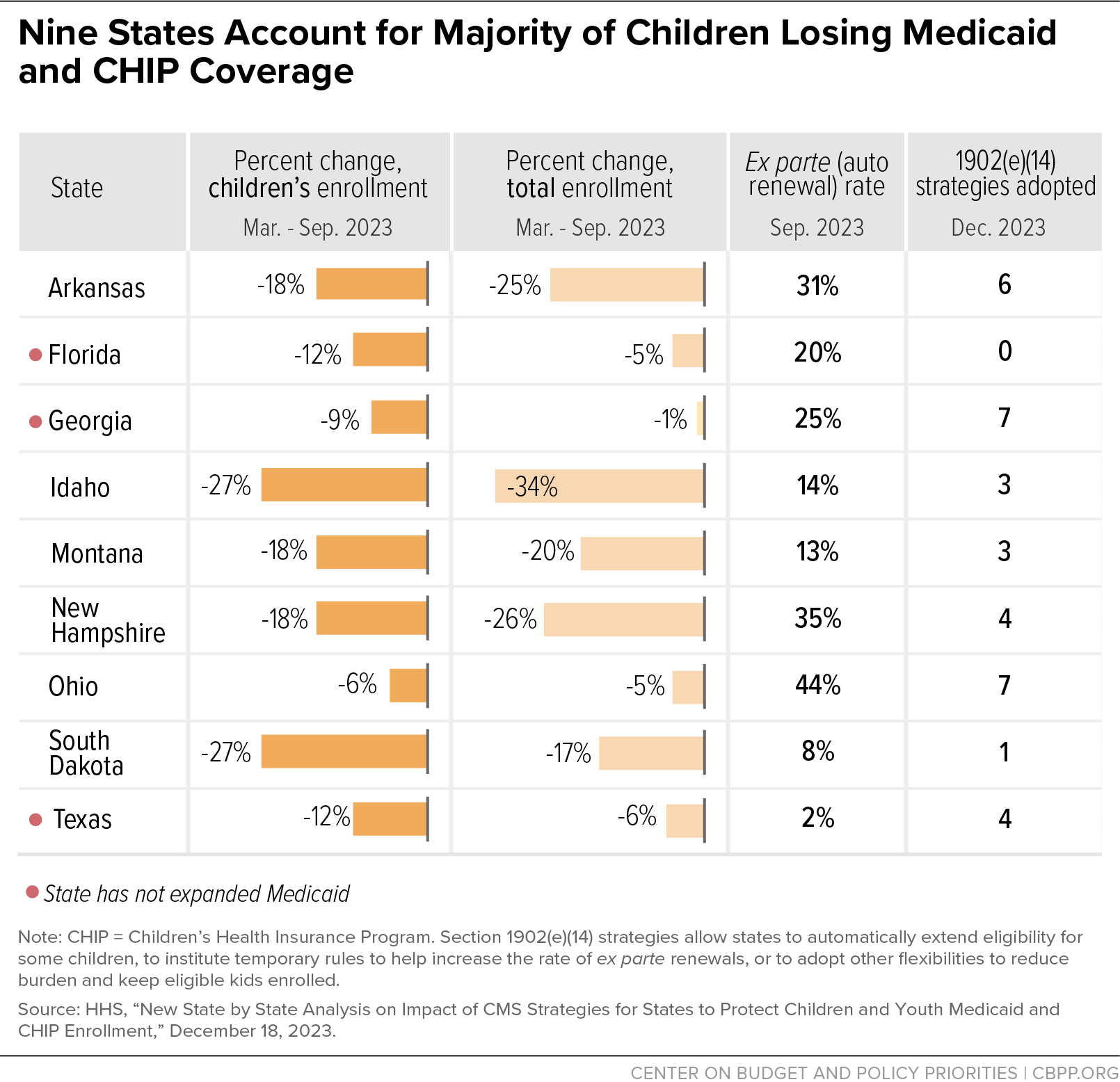
December 18 The Department of Health and Human Services (HHS) and Centers for Medicare & Medicaid Services (CMS) released a variety of materials to draw attention to children's coverage losses during unwinding and called on states to adopt strategies to stem coverage losses among children who continue to meet Medicaid and Children’s Health Insurance Program (CHIP) eligibility standards. The announcement comes in response to ongoing concern that Medicaid and CHIP enrollment among children dropped by more than 2.2 million between March 2023 and September 2023; the totals are even higher now.
Relying on newly released data about children’s coverage losses, the HHS Secretary sent letters to governors in the nine states with the highest child disenrollment rates by number and percentage, which account for about 60 percent of such coverage losses (see graphic). The letters urge these states — Arkansas, Florida, Georgia, Idaho, Montana, New Hampshire, Ohio, South Dakota, and Texas — to adopt additional strategies to help prevent eligible children from losing coverage, including by adopting additional section 1902(e)(14) waivers, which allow states to automatically extend eligibility for some children or to institute temporary rules to help increase the rate of ex parte renewals to reduce burden and keep eligible kids enrolled.
Higher ex parte rates and higher take up of renewal flexibilities are correlated with a smaller decrease in enrollment for children under age 19, CMS’s data show. The data also show that youth aged 19-23 make up a greater share of disenrollments in non-expansion states compared to expansion states (27.6 percent vs. 12.1 percent), underscoring that states’ choices not to expand Medicaid to adults leave many people in a coverage gap.
CMS also announced that section 1902(e)(14) flexibilities will remain in place at least through 2024. This extended timeline is intended to give states more certainty about adopting additional strategies now, knowing that they will not be required to phase them out this spring, when the unwinding period was originally projected to be complete.
To aid states, CMS posted several new tools:
- an informational bulletin highlighting a broad range of strategies states can use to help protect coverage for children;
- guidance with operational considerations for strategies (including section 1902(e)(14) waivers) to minimize procedural terminations; and
- slides with new guidance to support seamless transitions between Medicaid and CHIP.
Finally, CMS also posted a summary of unwinding data trends, reflecting data from March to September 2023.
December 12 CBPP published a piece in Health Affairs highlighting the ways in which unwinding is shining a light on our fragmented health coverage system and detailing opportunities for federal and state policymakers to fix long-standing challenges that make it hard for people to enroll in and retain Medicaid, Children’s Health Insurance Program (CHIP), and marketplace coverage.
Federal policy sets up a streamlined Medicaid eligibility and enrollment system for eligible people to enroll and stay enrolled. But many states have not fully implemented all of these requirements, and coverage losses during unwinding — especially among people who continue to meet Medicaid eligibility requirements — are magnifying the impact of these failures.
As we write in Health Affairs:
States should continue the work they started during the pandemic to create more user-friendly eligibility processes, including by developing clearer notices, ensuring that websites and call centers effectively facilitate online and telephonic applications and renewals, and establishing call centers that can provide effective help within reasonable wait times for all people, including for people with limited English proficiency.
Even with these improvements underway, it is clear that not all gaps in the eligibility and enrollment experience will be fixed during the unwinding period. Therefore, we write that federal and state policymakers have an obligation to continue to expand innovative changes, remedy failures, and improve transparency and accountability in the future.
Key opportunities that our piece highlights include:
- Increasing ex parte Medicaid renewals;
- Adopting continuous eligibility for adults and longer eligibility periods for children;
- Ensuring seamless coverage transitions between Medicaid, CHIP, and/or the marketplace; and
- Closing the Medicaid coverage gap.
December 6 An interim final rule (IFR) spelling out the Centers for Medicare & Medicaid Services’ (CMS’) enforcement authority during the unwinding period was released and went into effect on December 6. The rule — summarized in new CMS slides — implements unwinding standards enacted last year as part of the Consolidated Appropriations Act, 2023 (CAA) and codifies authorities CMS can use in its oversight of state unwinding activities during the statutorily defined unwinding period, April 1, 2023-June 30, 2024. (Some states may continue their unwinding activities longer, but the CAA authorities reflected in the IFR do not continue past June 30.)
For example, building on FAQs released earlier this year, the IFR codifies the unwinding data that states are required to report during the unwinding period, defines “timely” data submission, and sets out a process by which CMS can gradually reduce the Medicaid matching rate for states that fail to report required unwinding data. For states that do not meet federal renewal requirements, the IFR also sets out details about the process CMS can use to put states on corrective action plans (CAPs) and, thereafter, impose civil monetary penalties if a state fails to implement a CAP and/or require states to pause procedural terminations during the unwinding period.
The preamble to the IFR reiterates CMS’ ongoing interest in working collaboratively with states to bring them into compliance with regulations but sets out mitigating circumstances that could justify CMS applying enforcement discretion. Still, given the operational challenges that states across the country continue to have in timely and accurately renewing coverage, and the harm this has caused to people who remain eligible for Medicaid but may not be successfully renewed, the clarity now codified in regulations should encourage CMS to take enforcement action where needed during the remainder of the unwinding period.
The rule went into effect immediately, but CMS will take comments on the rule through February 2, 2024 and could consider changes in the future.
November 30 The Centers for Medicare & Medicaid Services (CMS) released monthly unwinding data, including August unwinding renewal outcomes and operations data as well as preliminary September unwinding outcomes data. The preliminary September outcomes data begin to reflect the initial impact of CMS’ direction to states to pause procedural terminations if they were conducting ex parte terminations on a household, rather than individual, basis.
The CMS-posted data continue to lag real-time state reporting, which is captured by KFF and the Georgetown Center for Children and Families (CCF) trackers.
Among the key takeaways from the data:
- 26.6 percent of all enrollees due for renewal in August had their Medicaid eligibility terminated, and procedural terminations again accounted for 70.9 percent of total terminations. Eleven states and the District of Columbia paused some or all procedural terminations in August due to issues identified in previous months.
- 22.2 percent of cases due for renewal were still pending at the end of August, slightly down from 25.1 percent in July. As we’ve noted before, backlogs in some states could reflect operational capacity challenges, while others could indicate that states have paused procedural terminations to address identified issues and to avoid improperly terminating eligibility for more people.
- The average ex parte renewal rate in August was 31.5 percent, which is again slightly higher than the previous month. Overall, while the nationwide ex parte renewal rate is still low, it has been slowly ticking up and, according to the preliminary September data, some states (including New Hampshire, New Mexico, and South Carolina) have raised their rates significantly.
- The release also includes information about people with previous Medicaid or Children’s Health Insurance Program enrollment who applied for coverage through the Affordable Care Act marketplaces or had their information transferred from Medicaid to the marketplace. The trends in the November-released Medicaid-to-marketplace transition data are consistent with the trends we observed in September’s release.
Coupled with large renewal backlogs, the August operations data include concerning metrics on application processing times with many states routinely exceeding the 45-day maximum allowable timeframe. The August operations data also indicate major challenges for people seeking assistance applying for or renewing coverage over the phone. Call center average wait times were 20 minutes or higher in 11 states.
November 22 The Centers for Medicare & Medicaid Services (CMS) released frequently asked questions (FAQs) about Transitional Medical Assistance (TMA) and cooperation with medical support requirements.
Parents and other caretaker relatives (P/CR) are entitled to 12 months of additional Medicaid coverage, known as TMA, when increases in their income disqualify them from Medicaid eligibility in the P/CR category. The FAQs provide an overview of TMA and answer a number of related questions, including how states should approach renewals during the unwinding process for individuals who were enrolled in or eligible for TMA during the continuous coverage period. Key unwinding-related takeaways include:
- In states that conducted renewals during the continuous coverage period and placed people into TMA for 12 months (or longer), these individuals may not receive an additional 12 months of TMA coverage when their case is up for renewal, unless they reenrolled in the P/CR group since then and subsequently experienced another TMA-qualifying event.
- In states that did not conduct renewals and did not place eligible people into TMA during the continuous coverage period, people who experienced a TMA-qualifying event must be given a new, prospective 12-month TMA coverage period even if more than 12 months have passed since the qualifying event.
- State agencies must conduct full renewals for people enrolled in TMA when their coverage is renewed during the unwinding process by first attempting to renew their coverage ex parte and, if that fails, by sending them a pre-populated renewal form to determine their eligibility for Medicaid on all possible bases.
The FAQs also touch on how state agencies should handle redeterminations for people who did not cooperate with medical support requirements while the continuous coverage requirement was in effect. Typically, Medicaid applicants who have a child with a parent living outside of the home must establish the identity of that parent and cooperate with the state in obtaining medical support from them as a form of child support (or provide good cause for not doing so); during the continuous coverage period, states did not disenroll people for failing to cooperate with these requirements. During unwinding, however, state agencies:
- Must conduct a full renewal for these individuals, providing them with the opportunity to either meet the cooperation requirements or provide a legitimate reason for not doing so.
- May disenroll people subject to medical support requirements without conducting a full renewal if their most recent eligibility determination took place within the last 12 months and they were given the opportunity to meet the requirements or provide good cause for not doing so.
November 17 The Centers for Medicare & Medicaid Services (CMS) recently made several updates to its unwinding website, adding useful resources and relevant information for state Medicaid agencies and advocates. Those include:
- An updated summary list of approved section 1902(e)(14)(A) waivers, designed to facilitate renewals and ensure due process during unwinding. An interactive map displays the number and type of waivers by state, and a more comprehensive dataset outlines all approved waivers by state.
- Information about states that have opted to delay procedural disenrollments. In a new table, which CMS expects to update monthly, CMS shows which states have delayed procedural disenrollments to reach more enrollees through targeted renewal outreach and to give enrollees more time to renew. The page reflects only voluntary pauses, not CMS-mandated delays in procedural terminations or ones that states implemented as they remedy their ex parte processes to properly determine eligibility on an individual (not household) basis.
- A presentation outlining federal requirements, key considerations, and best practices for state Medicaid agency eligibility determination and adverse action notices, along with sample notice language.
- An update to the CMS unwinding data reporting specifications that reflects various updates and clarifications. One notable new section details how CMS now requests that states report the outcomes of pending renewals once they go through the eligibility determination process — and not just continue reporting the number of those pending cases, which advocates were concerned painted an incomplete picture. CMS requests that states report these outcomes within three months after the reporting period. Data on cases that were pending in states’ April – August monthly reports are due by December 29, 2023.
October 31 The Centers for Medicare & Medicaid Services (CMS) released monthly unwinding data, including July unwinding outcomes and operations data as well as preliminary August unwinding data.
The CMS-posted data continue to lag real-time state reporting, which is captured by KFF and the Georgetown Center for Children and Families (CCF) trackers.
The final July data appear largely unchanged from the preliminary data that CMS issued in September. Given the overall consistency between the preliminary and final July data, below we highlight some preliminary August data that were released this month as a closer-in-time snapshot of redetermination outcomes. (CMS is only posting preliminary outcomes data on a state-by-state basis, without national totals, and is not yet posting preliminary operations data.)
Among the key takeaways from the new Medicaid unwinding and operations data:
- 23.3 percent of all enrollees due for renewal in July had their Medicaid eligibility terminated, and procedural terminations accounted for 70.9 percent of total terminations (down from 73.7 percent in June). Fourteen states paused some or all procedural terminations in July due to issues identified in previous months. (The July data do not yet reflect more recent pauses in procedural terminations in response to CMS oversight related to state ex parte processes, for example.)
- 25.1 percent of cases due for renewal were still pending at the end of July, slightly up from 24 percent in June. As we’ve noted before, backlogs in some states could reflect operational capacity challenges, while others could indicate that states have paused procedural terminations to address identified issues and to avoid improperly terminating eligibility for more people.
- The average ex parte renewal rate in July was 30.7 percent, which is slightly higher than June. Overall, while the nationwide ex parte renewal rate is still low, it has been slowly ticking up and, according to the preliminary August data, some states (including California, Hawai’i, and Arizona) have raised their rates significantly.
- The release also includes information about people with previous Medicaid or Children’s Health Insurance Program enrollment who applied for coverage through the Affordable Care Act marketplaces or had their information transferred from Medicaid to the marketplace. The trends in the October-released Medicaid-to-marketplace transition data are consistent with the trends we observed in September’s release.
October 27 The Centers for Medicare & Medicaid Services (CMS) approved a waiver Kentucky requested to delay for 12 months renewals for children under age 19. Kentucky requested this waiver to catch up on its high volume of renewals during the unwinding process and to improve operational and system issues that would otherwise contribute to process delays. Other states are reportedly considering similar requests to help protect coverage for children.
September 29 The Centers for Medicare & Medicaid Services (CMS) released monthly unwinding data, including June unwinding outcomes and operations data as well as preliminary July unwinding data, significantly reducing the delay between when states submit data to CMS and when CMS releases the data publicly.
Among the key takeaways from the new Medicaid unwinding and operations data:
- 25 percent of all enrollees due for renewal in June had their Medicaid eligibility terminated, and procedural terminations accounted for 73.7 percent of total terminations (down from 77 percent in May). Seventeen states paused some or all procedural terminations in June due to issues identified in previous months. Some states that reported high procedural terminations in May saw significant increases in application volume in June, suggesting many of those who lost coverage may still have been eligible.
- 24 percent of cases due for renewal were still pending at the end of June, up from 20 percent in May. Backlogs in some states could reflect operational capacity challenges that states are experiencing, while others could indicate that states have paused procedural terminations to address identified issues and to avoid improperly terminating eligibility for more people.
- The average ex parte renewal rate was only 29.4 percent (up slightly from 24.7 percent in May), highlighting that this is an ongoing challenge for states. The ex parte rate varied significantly across states, with six states reporting no or less than 10 percent ex parte and seven states reporting rates of 50 percent or greater. (In September, 30 states self-identified as improperly conducting ex parte renewals on a household, rather than an individual, basis; they are working to update their systems now.)
For the first time, the release also includes new data about enrollment in the Children’s Health Insurance Program (CHIP) and information about individuals who lost Medicaid or CHIP in April 2023 and transitioned to HealthCare.gov. In the 33 states that use HealthCare.gov (the health insurance marketplace operated by the federal government), 267,000 people who applied for marketplace coverage or had their information transferred by a state Medicaid agency had their Medicaid or CHIP coverage terminated in April 2023. Of this group, nearly 46,000 people (or 17 percent) selected a marketplace plan via HealthCare.gov.
Data on account transfers from Medicaid or CHIP to HealthCare.gov is available later than data on renewals and data on marketplace applications through HealthCare.gov, which is why CMS only now reported the April 2023 cohort transition data. (Previous months have included data about plan selection from HealthCare.gov and state-based marketplaces, but without the type of cohort analysis now available).
September 29 As part of its most recent monthly unwinding data report, the Centers for Medicare & Medicaid Services (CMS) included new data on transitions from Medicaid and the Children’s Health Insurance Program (CHIP) to the Affordable Care Act (ACA) marketplace in the 33 states that use HealthCare.gov. Many people moving from Medicaid or CHIP to the marketplace face barriers to enrolling in coverage, the data suggest.
Many people who lose Medicaid during the unwinding period will still be eligible for Medicaid. However, one-third of those who lose Medicaid during unwinding are projected to be eligible for ACA marketplace coverage with premium tax credits. While a system is in place to transfer people from Medicaid to the marketplace if they are likely to be eligible for a marketplace plan, relatively few people are completing enrollment this way.
Previously, CMS reported information on people who applied for coverage on HealthCare.gov and were previously enrolled in Medicaid. But this statistic only includes people who applied for coverage, not those who were eligible for marketplace coverage but did not apply. For the first time, the September data release included people whose information was transferred to HealthCare.gov from state Medicaid agencies, regardless of whether they applied for coverage.
Medicaid agencies are not supposed to send these account transfers if a person loses Medicaid or CHIP for procedural reasons (disenrollments due to paperwork, rather than being determined ineligible for Medicaid). This is because many people who lose Medicaid and CHIP for procedural reasons are likely still eligible for those programs rather than for financial help through the marketplace.
The new data show that so far, only a small percentage of applications HealthCare.gov received via account transfer resulted in a household applying for coverage and selecting a health plan, suggesting flaws in a system that has the potential to link hundreds of thousands of people losing Medicaid to coverage. Most people (85 percent) who lost Medicaid or CHIP coverage in April 2023 and later interacted with HealthCare.gov had their information transferred by the state Medicaid agency. But just 11 percent of people in this group applied for marketplace coverage, and only 7 percent selected a plan.
That’s likely because the contact information on account transfers is often incomplete, inaccurate, or missing, hindering outreach efforts. But even people who receive a notice that their information has been transferred to the marketplace may not understand the notice or know that they need to take action to enroll. Those who make it to HealthCare.gov must complete multiple steps to gain coverage, including completing a lengthy application, selecting a plan, and paying the first month’s premium.
Encouragingly, it seems that when people who lost Medicaid or CHIP coverage submitted a HealthCare.gov application, they were highly likely to gain marketplace coverage and be eligible for financial help. Between April and June 2023, approximately 440,000 people who previously had Medicaid or CHIP applied for coverage through HealthCare.gov. Eighty-eight percent were determined eligible for marketplace coverage, 77 percent were eligible for premium tax credits, and 67 percent ultimately selected a health plan.
The 18 states that operate their own health insurance marketplace cannot be directly compared to those that use HealthCare.gov, as they report slightly different metrics. But the data here also suggest challenges in completing enrollment. Between April and June 2023, 69 percent of the almost 600,000 state-based marketplace applicants who lost Medicaid at renewal were determined to be eligible for marketplace coverage. Forty-one percent were eligible for financial assistance, but only 11 percent selected a plan.
Additional research and analysis are needed to fully understand variations across states, how many people are enrolling in coverage from other sources (including employers), and what improvements can be made to reduce barriers to coverage transitions.
September 29 The Centers for Medicare & Medicaid Services (CMS) issued guidance to states regarding 12-month continuous eligibility (CE) for children enrolled in Medicaid and the Children’s Health Insurance Program (CHIP), which all states must adopt by January 2024.
Twelve-month CE — in which most children retain eligibility even if they experience midyear changes in income that would otherwise trigger at least reexamination of their eligibility and potentially termination of coverage — has long been a state option. According to CMS, 21 states have CE for children in both Medicaid and CHIP, and 11 more states have CE in at least one program.
Congress made CE a requirement for children as part of the same legislation that set an end date for the pandemic continuous coverage protection. The pandemic-era continuous coverage provision protected coverage for people of all ages over multiple years, providing important lessons about the value of minimizing administrative barriers that can lead to disruptions in coverage, even for people who continue to meet eligibility requirements. Studies of CE also show reduced rates of churn (the percentage of children who disenroll and reenroll within a year).
The new CE requirement does not eliminate the need for states to redetermine eligibility for children as part of unwinding, but the guidance explains that states must begin a new 12-month CE period for children whose eligibility is renewed during unwinding. Providing 12-month eligibility periods will help protect coverage for children going forward and will reduce administrative burdens on agencies as they work through their unwinding caseload because states will not have to process changes in circumstances for children during their 12-month eligibility period.
The new CMS guidance explains differences between current CE requirements and those that will take effect in January. It also makes clear that mandatory CE is not required for children enrolled through medically needy Medicaid coverage, which allows people with high medical expenses to qualify for Medicaid in certain circumstances, or children eligible only based on Transitional Medical Assistance, which provides time-limited coverage to enrollees who experience an income increase, for instance because a parent gets a higher-paying job.
Notably, the guidance explains CE considerations related to special populations, including youth determined eligible for Medicaid or CHIP who are later incarcerated (for whom states often pause Medicaid benefits because of limits on federal financial support) as well as pregnant people receiving prenatal care and other pregnancy-related benefits under the “from conception to end of pregnancy” option (a CHIP option that many states adopt to address the health care needs of pregnant people who are immigrants and who do not otherwise qualify for Medicaid or CHIP).
To comply with the new requirements, states that do not have CE, that apply CE to a subset of their under 19 population, or that have CE but for less than 12 months will have to submit a state plan amendment (SPA) to comply with the new requirement. Medicaid SPAs must be submitted by March 31, 2024 to meet the new requirements; CHIP SPAs must be submitted no later than the end of state fiscal year 2024. Finally, CMS reiterates that states interested in providing CE for children for longer than 12-months, or for adults, may apply for a Section 1115 waiver.
September 21 The Centers for Medicare & Medicaid Services (CMS) released a list of 29 states plus the District of Columbia that to date have self-identified as erroneously making ex parte renewal decisions on a household level, rather than an individual level as federal regulations require. Ex parte renewals use already available data, reducing burdens on enrollees; in its materials CMS characterizes ex parte renewals as “one of the strongest tools that states have to keep eligible people enrolled in Medicaid or CHIP [Children’s Health Insurance Program] coverage during the renewals process.”
CMS identified this issue in late August, which we now know led to nearly half a million children and other individuals losing coverage. CMS directed states to report by September 13 on whether they had this issue and, if so, the steps the state would take to address it. CMS set out steps that impacted states must take to pause procedural terminations, reinstate coverage, implement mitigation strategies, and fix their systems and processes.
Key takeaways from the information posted by CMS include:
- To date, 29 states and D.C. self-identified as having the issue; others are continuing to assess their systems and whether people erroneously lost coverage.
- States will reinstate coverage for nearly 500,000 children and other individuals who were improperly disenrolled from Medicaid or CHIP.
- CMS is requiring these states to pause procedural disenrollments for impacted people, unless the state can ensure all eligible people are not being improperly disenrolled due to this issue.
- CMS will offer direct assistance as states work to complete their assessments and achieve compliance.
CMS’ decision to post this information shortly after it received it from states is a key step to holding states accountable for addressing the issue, which they are starting to do by reinstating coverage for impacted people. For example, last week Nevada announced that it had reinstated eligibility for 130,000 people.
Transparency will also help stakeholders across the country raise awareness among people who erroneously lost coverage and help make sure they know their coverage was reinstated.
September 15 States across the country continue to take different approaches to unwinding, with varied impacts on Medicaid enrollees in their states as a result. At least 6.4 million people nationwide have lost coverage as of September 13, KFF’s unwinding tracker reports.
This week, two states were in the news for very different reasons: Idaho completed its renewal process for cases kept open during the pandemic, while Hawai’i announced it was pausing terminations until January 2024.
- Idaho completed its six-month long unwinding process. Idaho announced on September 8 that the state completed its unwinding process after only six months, processing 153,196 renewals for individuals who were kept enrolled due to the continuous coverage provision. The state prioritized moving quickly, starting with sending notices in February and initiating the first terminations in April. Overall, the state determined that 31,900 of cases held open during the pandemic were eligible to remain enrolled, while 121,296 were ineligible. Over half of all renewals conducted during the state’s unwinding process resulted in procedural terminations (as opposed to someone being determined to no longer qualify for Medicaid).
- Hawai’i is pausing Medicaid terminations until January 2024. According to the state’s Medicaid agency, this means coverage for current enrollees will continue through at least the end of the year, except for people who request to end their coverage or who move out of state. Hawai’i will continue processing ex parte renewals (i.e., renewals using available data, which reduces burdens on enrollees) and will let people know if their coverage was renewed; for people who cannot be renewed at this time, the Medicaid agency will notify enrollees about their new renewal month.
Hawai’i did not explain why it is pausing terminations, nor did it explain whether it was pausing voluntarily or because the Centers for Medicare & Medicaid Services (CMS) directed the state to do so. It is possible that Hawai’i is one of more than a half dozen states that are improperly conducting ex parte renewals by requiring the entire household to be eligible for renewal in order to complete an ex parte, rather than completing an ex parte renewal for each person for whom it has data indicating continued eligibility. CMS required states to report back by September 13 if they have this issue and, if so, their plans to address it, which could include pausing renewals until the issue is fixed.
August 31 The Centers for Medicare & Medicaid Services (CMS) posted state unwinding data for May 2023, its second unwinding data release (see below for more on the initial data release last month). CMS is posting the data as required by the Consolidated Appropriations Act of 2023, but many states have already released more recent data. The KFF Medicaid Enrollment and Unwinding Tracker shows that at least 5.5 million Medicaid enrollees have lost coverage as of August 29.
All states reported operations data for May, again showing a wide range of application processing timelines, call center wait times, and call center abandonment rates. These May data formed the basis of the precompliance letters that CMS sent to all states on August 9. The full data released for May show an increase in application volume, which likely reflects people who lost coverage in previous months reapplying.
The newly released renewal outcomes data include some troubling trends from the 36 states that had begun unwinding-related terminations as of May 2023:
- 29 percent of all enrollees due for renewal had their eligibility terminated for a procedural reason, and procedural terminations accounted for 77 percent of all terminations;
- 20 percent of cases due for renewal were still pending at the end of May, suggesting ongoing processing backlogs; and
- The average ex parte renewal rate was only 24.7 percent, highlighting that states can do much more to ease the administrative burden on people seeking to renew coverage.
System and policy errors that CMS publicized and directed states to fix on August 30 likely contributed to the low rates of ex parte renewals and high rates of procedural terminations; more than a dozen states will have to pause procedural terminations and reinstate coverage as they fix their systems. It will be several months before the CMS-posted data reflect these changes.
The May data also include metrics showing enrollment in Healthcare.gov and state-based marketplace states; in September CMS will post data that provide more information about transitions from Medicaid to the Marketplace.
Finally, CMS updated its overview of Data Sources and Metrics with this month’s release.
August 30 The Centers for Medicare & Medicaid Services (CMS) reminded state Medicaid directors of their obligation to follow all federal Medicaid renewal requirements, specifically the requirement to conduct ex parte renewals at the individual rather than household level. (Ex parte renewals use data already available, reducing burdens on enrollees.) Some family members, including many children, were being incorrectly disenrolled from coverage in over a dozen states because other members of their household couldn’t be renewed ex parte.
CMS’s letter specifies steps states must take to end family-based ex parte renewals, including reinstating people who have already lost coverage. If they don’t take these steps, states risk losing this year’s enhanced federal Medicaid matching rate, or could face other corrective actions.
Individual determinations aren’t just required by federal regulations; they’re also particularly important to ensure eligible children remain enrolled in Medicaid. Since Medicaid income eligibility levels for kids are higher than for adults, children are often eligible for coverage even if their parents aren’t. The high numbers of kids losing coverage during unwinding is likely in part a result of state systems that assess eligibility at the household level.
Household-level ex parte determinations also put some adults at risk of improperly losing coverage, such as people whose household includes someone with a disability. People whose coverage should have been renewed ex parte are being asked to submit information to maintain their Medicaid eligibility, creating an extra step that raises the risk of procedural terminations (disenrollments due to paperwork, which can affect people actually eligible for benefits). This also imposes burdens on strapped state systems.
CMS is now requiring all states to review their systems to ensure that ex parte renewals are happening at the individual level. States must respond no later than September 13 to either certify compliance with federal requirements or to share information about how the state will come into compliance; CMS provided a template that states can use. The State Health and Values Strategies Project also posted a toolkit to help states review their systems and assess whether they are properly conducting ex parte renewals at the individual level.
These are the steps states must take if they’re conducting household-level ex parte reviews:
- Pause procedural terminations for people whose coverage may be terminated under this error;
- Reinstate coverage for people procedurally disenrolled due to improper ex parte systems — retroactive to the date of disenrollment — and notify people that they have been reinstated;
- Implement mitigation strategies to prevent additional improper enrollments (e.g., manually renew coverage pending a systemic fix; suspend renewals while fixes are being made; extend eligiblity for 12 months from the scheduled renewal date); and
- Fix systems and processes to make sure renewals are conducted in accordance with Medicaid requirements.
States have significant work ahead to remedy the problems with ex parte renewals, and the National Association of Medicaid Directors indicates that some have already started doing it. CMS’s letter is an important step to protect coverage for people who meet Medicaid eligibility criteria. Monitoring how the states in question make the required changes will be crucial to ensuring eligible people stay covered.
August 22 Three Florida residents filed a lawsuit against the Florida Agency for Health Care Administration (AHCA) and the Department of Children and Families (DCF) for terminating their Medicaid coverage without providing adequate written notice and explanation. The plaintiffs allege that such inadequate notices violate the Due Process Clause of the Fourteenth Amendment and the Medicaid Act. Chianne D. et al. v. Jason Weida is the first lawsuit challenging the unwinding process. The plaintiffs are represented by the Florida Health Justice Project and the National Health Law Program.
The plaintiffs allege that the termination notices sent by DCF are confusing, do not clearly explain why people are losing their Medicaid coverage, and make it difficult to decipher which family members within a household are losing or maintaining their coverage. In response to the litigation, DCF claims that its notices do not violate federal regulations, noting that the Centers for Medicare & Medicaid Services approved the agency’s plan for redetermining enrollees’ Medicaid eligibility and that these notices are one of multiple methods the agency uses to communicate with enrollees during the eligibility determination process.
The complaint asks the U.S. District Court to intervene in Florida by instructing AHCA and DCF to reinstate all Medicaid enrollees whose coverage was terminated after receiving similar notices, and to pause Medicaid terminations until the state fixes this issue by improving the language and information provided in its termination notices.
August 9 The Centers for Medicare & Medicaid Services (CMS) sent letters to all states reviewing their respective data (from May 2023) on three sets of metrics for Medicaid and the Children’s Health Insurance Program (CHIP) and reminding them of their legal obligations and of policies affecting each of these areas. For some states CMS highlighted concerns, including long call center wait times, a high share of disenrollments for procedural (vs. eligibility-related) reasons, and application processing times above the 45-day standard applicable to most enrollees.
All of these areas can contribute to the documented difficulties that eligible enrollees are having renewing their Medicaid coverage during unwinding. Notably, the CMS letters connect each of these three areas with federal rules that govern state eligibility and enrollment operations. For example, CMS notes that excessive call center wait times and call abandonment rates “may indicate potential non-compliance with” the federal requirement that people be able to apply for or renew Medicaid and CHIP by telephone. And the letters reference particular access concerns and states’ responsibilities (previously detailed in a letter from the Department of Health and Human Services Office for Civil Rights ) to ensure access for people of color, people with limited English proficiency, and people with disabilities.
The letters, and the data they include, vary greatly across states. Some of that can be explained by states being at different stages of the unwinding process, which can last through next spring, and which some states are taking more time to complete than others. It is also important to evaluate call center data carefully because metrics may reflect the features and setup of call centers in each state.
States received different versions of the letter based on their individual data (see table below), but all of the letters identify strategies by which states could improve functionalities and, where applicable, address deficiencies. CMS identified concerns across all three metrics in five states (Alaska, Florida, Montana, New Mexico, and Rhode Island); across two metrics in 13 states; and across one metric in 18 states and the District of Columbia. Only 14 states have satisfactory data across all three metrics, although CMS recommends that all states review their data and consider adopting strategies to improve call center wait times, reduce terminations for procedural reasons, and implement strategies to ensure timely and accurate application processing.
CMS further indicates it could take compliance actions with states that don’t quickly address concerns.
The Consolidated Appropriations Act (CAA) of 2023 provides an increased Medicaid matching rate through the end of this year to support states in their unwinding efforts, so long as they adhere to federal redetermination requirements. Over the last few months, CMS has threatened to withhold this match from states unless they remedy gaps in their eligibility processes that violate federal requirements.
CMS can also impose corrective action plans on states that do not comply with standards set out in the CAA or in other federal requirements; if a state fails to implement a corrective action plan under the CAA, CMS can require it to pause procedural terminations, and impose financial penalties.
These letters are an important step to document areas of concern so that states can address them. CMS has many tools to help protect coverage for eligible enrollees; the letters underscore that CMS is prepared to take more forceful action if states do not voluntarily improve deficiencies.
May 2023 Eligibility and Enrollment Performance Indicator and Unwinding Data
| (data as of July 31, 2023) Metrics where CMS notes concern are highlighted. | ||||
|---|---|---|---|---|
| Call Center Operations | Procedural Terminations | Application Determination Processing Time | ||
| State | Average call center wait time | Average call abandonment rate | % of beneficiaries terminated for procedural reasons as a share of total beneficiaries due for renewal in May | % of application determinations processed in more than 45 days (for people eligible based on Modified Adjusted Gross Income or MAGI*) |
| Alabama | 1 minute | 4% | N/A** | 1% |
| Alaska | 16 minutes | 24% | 28% | 40% |
| Arizona | 21 minutes | 18% | 27% | 3% |
| Arkansas | 10 minutes | 16% | 35% | 5% |
| California | 2 minutes | 4% | N/A** | 18% |
| Colorado | 4 minutes | 8% | 26% | 3% |
| Connecticut | 1 minute | 3% | 19% | 0% |
| Delaware | 1 minute | 10% | 4% | 0% |
| District of Columbia | 1 minute | 5% | 23% | 26% |
| Florida | 32 minutes | 38% | 14% | 10% |
| Georgia | 1 minute | 0% | 13% | 12% |
| Hawaiʻi | 7 minutes | 30% | 27% | 1% |
| Idaho | 34 minutes | 7% | 51% | 1% |
| Illinois | 12 minutes | 34% | N/A** | 3% |
| Indiana | 5 minutes | 8% | 27% | 1% |
| Iowa | 0 minutes | 1% | 2% | 2% |
| Kansas | 23 minutes | 32% | 0% | 11% |
| Kentucky | 1 minute | 1% | 31% | 0% |
| Louisiana | 1 minute | 2% | N/A** | 4% |
| Maine | 35 minutes | 27% | 1% | 10% |
| Maryland | 1 minute | 7% | 21% | 0% |
| Massachusetts | 2 minutes | 3% | N/A** | 0% |
| Michigan | 1 minute | 1% | N/A** | 1% |
| Minnesota | 3 minutes | 12% | N/A** | 0% |
| Mississippi | 1 minute | 5% | N/A** | 4% |
| Missouri | 48 minutes | 44% | N/A** | 1% |
| Montana | 42 minutes | 40% | 36% | 15% |
| Nebraska | 5 minutes | 12% | 9% | 11% |
| Nevada | 13 minutes | 56% | 45% | 1% |
| New Hampshire | 11 minutes | 12% | 45% | 3% |
| New Jersey | 1 minute | 3% | N/A** | 10% |
| New Mexico | 20 minutes | 19% | 28% | 44% |
| New York | 0 minutes | 1% | N/A** | 0% |
| North Carolina | 0 minutes | 1% | N/A** | 5% |
| North Dakota | 2 minutes | 13% | 35% | 15% |
| Ohio | 4 minutes | 3% | 16% | 11% |
| Oklahoma | 0 minutes | 1% | 35% | 0% |
| Oregon | 15 minutes | 24% | N/A** | 0% |
| Pennsylvania | 6 minutes | 12% | 9% | 1% |
| Rhode Island | 39 minutes | 21% | 11% | 12% |
| South Carolina | 14 minutes | 31% | 49% | 4% |
| South Dakota | N/A*** | N/A*** | 32% | 0% |
| Tennessee | 0 minutes | 1% | N/A** | 1% |
| Texas | 8 minutes | 16% | 52% | 16% |
| Utah | 35 minutes | 26% | 48% | 3% |
| Vermont | 1 minute | 1% | 30% | 2% |
| Virginia | 1 minute | 1% | 6% | 17% |
| Washington | 0 minutes | 4% | 43% | 2% |
| West Virginia | 9 minutes | 19% | 24% | 4% |
| Wisconsin | 6 minutes | 8% | N/A** | 1% |
| Wyoming | 0 minutes | 0% | 0% | 3% |
July 28 In the first of what will be monthly releases over the next year, the Centers for Medicare & Medicaid Services (CMS) released unwinding data from the first two months of Medicaid terminations, including data from the 18 states that had completed at least one cohort of renewals by April 30. While states have already made some of these data public, the CMS-posted data provide a snapshot across all states. Among the 18 states that had completed at least one full cohort of unwinding-related renewals, 2.2 million people were due for renewal, just over 1 million were renewed, nearly 715,000 people were disenrolled from Medicaid/Children’s Health Insurance Program (CHIP), and about 492,000 renewals are still pending. More recent KFF data shows at least 3.8 million Medicaid enrollees have been disenrolled as of July 28.
This month’s CMS release includes:
- March and April redetermination summary data from the states that began terminating eligibility, along with more detailed data files;
- operational data from all states, including enrollment numbers and enrollment changes between March and April; applications received; application processing timeliness; and call center statistics, including wait times and abandonment rates;
- historic trend data from 2018 showing that 22 percent of Medicaid enrollees lost coverage sometime during that year. By comparison, coverage terminations nationwide during the first months of unwinding are around 30 percent;
- an infographic highlighting historical trends in Medicaid and CHIP enrollment and recapping April 2023 data; and
- data showing marketplace applications in states using HealthCare.gov and in states with state-based marketplaces. In September, CMS plans to release additional data about coverage transitions for people who left Medicaid/CHIP in HealthCare.gov states.
The operational data show wide ranges in call center wait times. As we previously explained, people’s ability to get help from a state’s Medicaid call center, with minimal wait times, is an important sign of how well an agency is serving Medicaid enrollees and applicants during unwinding. The data also show wide variety in application processing times and rates of ex parte renewal (renewals using available data without requiring enrollees to return forms).
All of these factors can impact the ease with which individuals can enroll and reenroll in coverage. Department of Health and Human Services (HHS) Secretary Xavier Becerra noted this in a letter to governors, reiterating that it is states’ responsibility to administer their programs consistent with federal requirements, encouraging states to adopt strategies to improve required ex parte renewals, and underscoring HHS’s oversight responsibility and intent to take action when states are not in compliance with federal requirements.
Overall, there are many caveats and nuances to consider when interpreting the data. Some states held procedural terminations at the beginning of unwinding or had significant backlogs at the end of each month, factors that greatly affect the reported data. Some states prioritized those they thought were ineligible, which led to higher rates of terminations in the early months of unwinding. And some states attempted manual ex parte renewals when forms weren’t returned, which doesn’t show up in the reported ex parte rates.
As CMS continues to release data each month, we will likely see how different policy choices and operational capacity across states affect retention rates. With many months of unwinding ahead, and opportunities for states to make mid-course corrections to their policies and operations, it is essential to get these data timely. That is why 35 leading patient groups called for more timely release of the data going forward.
July 21 As states continue to report Medicaid unwinding data, many states have very high numbers of pending renewals – renewals that were initiated but not processed by the scheduled end of an enrollee’s eligibility period. In some states, this number includes renewal forms that were submitted before the enrollee’s eligibility period ended, but the state or county has not yet processed.
Enrollees’ Medicaid coverage should continue until the agency completes the renewal form. But they may not realize that they’re still covered – if they haven’t gotten a notice confirming their eligibility – and may forgo care or have to make multiple phone calls to determine their status. If a state or county is unable to process a large portion of the renewals they receive in a month, this indicates major operational issues that will likely increase as the state sends out more renewals, handles reapplications from people who lost coverage, and fields phone calls from a growing number of residents who don’t know if they have coverage or not.
In other states, a large volume of pending renewals may be the result of the state delaying procedural terminations, either due to system or policy issues it needs to correct or because it has adopted the Center for Medicaid & Medicaid (CMS) strategy to delay procedural terminations by 30 days to give more time to do outreach to individuals who haven’t returned their forms. (Procedural denials occur when a person loses their coverage for a reason other than a confirmation that they are no longer eligible. For example, they can happen when a Medicaid enrollee does not receive their paperwork in time, if they do not return requested documents in time, or because the state lost track of paperwork someone sent in.)
Whether pending renewals are caused by a concerning reason (processing backlog) or client-friendly reason (delaying procedural terminations), they have a huge impact on unwinding data that states are reporting. If the pending renewals are mostly people who have returned their forms, this population is disproportionately likely to be determined eligible when those forms are processed, which will affect the percentage of cases renewed vs. terminated. And for those who are found ineligible based on their renewal form, that finding of ineligibility will lower the percentage of denials due to procedural reasons. Conversely, a state that delayed procedural terminations may have a low procedural denial rate in their reported data before the pending renewals are processed. But it will deny a large number of cases for procedural reasons the next month if the forms are not returned.
However, due to how CMS data reporting is currently structured, these pending renewals will never be reported. They won’t show up in the next month’s report, and the original report won’t be revised when these pending cases are processed. While CMS is working on a plan to better capture the outcomes of these cases, it’s important to consider the impact of these pending renewals while analyzing procedural denial rates and comparing outcomes across states. States can also report on these outcomes through state reports and dashboards.
July 20 The Centers for Medicaid & Medicaid Services, the Department of Treasury, and the Department of Labor sent a letter urging employers and health plan issuers to grant people losing Medicaid and transitioning to employer-sponsored insurance (ESI) the same special enrollment period (SEP) that will be used on HealthCare.gov for people transitioning to marketplace coverage. The temporary marketplace unwinding SEP is available until July 31, 2024, for anyone who loses Medicaid/CHIP between March 31, 2023, and July 31, 2024.
Currently, federal law requires that people who lose Medicaid/CHIP be given an SEP of at least 60 days to enroll in an employer-based plan. Employers and plans can offer a longer period, but that is not required. Given the complexity of the unwinding process, 60 days may not be enough time for many people. They may not receive notices that they are losing coverage on time or at all, or they may be confused about whether they can enroll in subsidized marketplace coverage instead of ESI. People with an offer of ESI that is considered affordable (does not exceed 9.12 percent in 2023) are not eligible to receive financial help with marketplace coverage.
An estimated 3.8 million people losing Medicaid/CHIP due to unwinding have an affordable offer of ESI. Some of these people are in mixed coverage status households, where some members are eligible for Medicaid/CHIP or marketplace coverage with financial assistance, and others are eligible for ESI. Aligning the SEPs would make it easier for more people to make a successful transition to another form of affordable coverage, prevent coverage gaps, and ensure people have ongoing access to needed care.
July 18 The Centers for Medicare & Medicaid Services (CMS) released two documents that provide insights into how the agency is working with states to address their failures in following federal rules in eligibility redetermination processes, which can contribute to coverage losses. CMS’s July 18 release shows that the majority of states are out of compliance with basic renewal functionalities like conducing ex parte renewals for all enrollees (26 states), allowing renewal through all required modalities, including online and by phone (19), and supporting transitions to marketplace coverage (6). CMS describes both actions states have taken voluntarily to address these failures and steps the agency can take where state actions are not sufficient.
-
Summary of State Mitigation Strategies for Complying with Medicaid Renewal Requirements Described in the Consolidated Appropriations Act, 2023. This document describes CMS-approved mitigation strategies that specific states adopted to address areas of non-compliance with Medicaid renewal requirements, as of March 31, 2023. Since before unwinding began, CMS has worked with states to identify gaps in compliance with Medicaid renewal requirements and to identify alternative strategies states can use to address these shortcomings while working to fully meet the requirements. These strategies are designed to help protect coverage for people who are eligible. States that aren’t in compliance must adopt mitigation strategies as a precondition for receiving the increased Medicaid matching rate that is in effect during the unwinding period.
The summary list posted by CMS includes ten mitigation strategies that various states have adopted, including pausing procedural terminations until approved mitigations are implemented, conducting manual data checks as an alternative to conducting fully automatic (or ex parte) renewals, and adopting approaches to facilitate renewals when required online or telephonic functionality is not in place.
CMS had not previously shared these mitigations or the extent to which states have adopted them. The list indicates that only 16 states had not adopted any mitigations as of March 31, although some of those states have experienced rapid coverage losses since unwinding started, which in some cases could be the basis for future CMS oversight activity, as described below.
-
Fact Sheet: Returning to Regular Medicaid Renewals: Monitoring, Oversight, and Requiring States to Meet Federal Requirements. This fact sheet reiterates CMS’s commitment to keeping eligible enrollees covered during unwinding and describes the levers that CMS has to ensure states’ compliance with federal requirements that are designed to protect enrollees during the renewal process.
During the unwinding period, CMS can withhold the enhanced Medicaid matching funds from states that do not remedy gaps in their eligiblity processes that violate federal requirements. If needed, CMS can put states on corrective action plans to align eligiblity renewals with federal requirements. If a state fails to implement a corrective action plan, CMS can require them to pause procedural terminations and impose financial penalties.
CMS has not yet put any states on a corrective action plan, but the fact sheet provides several examples of states that have taken steps to avoid losing the increased Medicaid matching rate. For example, one state paused procedural terminations, reinstated eligiblity, and conducted additional outreach in response to documented violations.
July 1 Beginning July 1, Congress authorized CMS to withhold federal Medicaid funding from states that do not report unwinding data that they are required to report to CMS under the Consolidated Appropriations Act, 2022. CMS released frequently asked questions (FAQs) about states’ data reporting obligations, and CMS’s compliance responsibilities, on June 30. The agency is also working on a new rule to provide further clarity about these new requirements (which are set forth in section 1902(tt) of the Social Security Act).
The CAA requires states to submit, and CMS to make public, monthly unwinding data from April 2023 through June 2024; the new FAQs include information on required reporting elements, acceptable data sources, and state reporting deadlines. Some of the information in the FAQs has been issued previously, and indeed states have already been reporting data to CMS. CMS has not yet posted data from the first months of unwinding but is expected to begin posting data — as also required by the CAA — later this summer.
The FAQs reiterate that if states do not provide the required data in a timely manner, the CAA requires CMS to reduce the federal medical assistance percentage (FMAP) determined for the state for that quarter by the number of percentage points (not to exceed 1 percentage point) equal to the product of 0.25 percentage points and the number of fiscal quarters during the period for which the state has failed to satisfy such requirements.
The FAQs also note that in states running state-based marketplaces (SBM), the penalty for late reporting would apply if an SBM fails to timely report required data. CMS notes that it will not levy this penalty on states making a good-faith effort to submit the required data in a timely manner. Finally, CMS explains that if it takes an FMAP reduction and the state later submits the data, CMS does not intend to restore the lost federal financial participation because CMS would not consider the delayed submission to be timely.
June 30 CMS released an updated chart showing state timelines for initiating unwinding-related renewals. The chart shows when states are initiating unwinding-related renewals; the effective date of the first anticipated eligibility termination date for the first cohort of unwinding renewals; how long states anticipate taking to renew their Medicaid population; and whether and how states are prioritizing individuals they identify as likely ineligible (the so-called “COVID-protected”) groups. The chart will help put unwinding data in context. For example, states prioritizing likely ineligible individuals in the early months of unwinding may have higher termination rates than states that do not.
June 12 In response to large coverage losses during the first two months of unwinding, the Secretary of the Department of Health and Human Services (HHS) on June 12 encouraged governors to step up their efforts to protect people from losing coverage, especially for procedural reasons such as not returning a renewal form. The Secretary’s letter encouraged states to continue partnering with stakeholders to get the word out about unwinding. The Centers for Medicare & Medicaid Services (CMS) launched new outreach and educational resources to support an “all hands on deck” strategy to reach enrollees.
Alongside the letter, CMS unveiled several new flexibilities for states to help minimize terminations for procedural reasons. Since the pandemic, states and CMS have agreed on waivers to make it easier for people to renew their coverage, including by streamlining workload for state agencies that are handling a record number of renewals. These waivers (called “e-14 waivers”) are granted under section 1902(e)(14) of the Social Security Act, which authorizes waivers needed to “ensure that states establish income and eligibility determination systems that protect beneficiaries.”
CMS is attempting to address problems that it and states have identified in the early months of unwinding, including making it easier for enrollees to complete redeterminations and for people whose eligibility was terminated for procedural reasons to reenroll. For example, under the new flexibilities:
- States can delay procedural terminations for one month while they conduct targeted outreach about renewals. Given findings about low awareness among enrollees about the need to complete renewal forms, this strategy could help boost targeted outreach and protect people from losing coverage when they are still eligible.
- States can designate pharmacies, community-based organizations, and/or health care providers to facilitate reinstatement of coverage for people who were recently disenrolled for procedural reasons. This would allow people to regain coverage at the point of service, pending a final eligiblity determination.
- States can reinstate eligibility effective on the individual’s prior termination date for those who were disenrolled based on a procedural reason and are subsequently redetermined eligible for Medicaid in the 90-days after they were disenrolled.
- Medicaid managed care plans can help enrollees complete their renewal forms (but not sign on their behalf).
Along with the new flexibilities, it is critical that CMS continue its monitoring and oversight efforts to ensure that states comply with federal rules regarding renewals and act quickly to address any violations. Not all coverage losses stem from violations, but for those that do, the Secretary’s letter notes that HHS “will not hesitate to use the compliance authority provided by Congress, including requesting that states pause procedural terminations under conditions outlined by the Consolidated Appropriations Act, 2023, should it be needed.”
June 5 As states unwind, they need to ensure their eligibility systems are reliable and well tested. The Centers for Medicare & Medicaid Services (CMS) has required states to submit multiple documents, called System Readiness artifacts, to demonstrate their readiness with technical system and process changes associated with unwinding. Some states have chosen to post their artifacts publicly. These artifacts are an opportunity for interested parties, particularly community advocates, to acquire insight into the technical issues and client scenarios that state agencies are prioritizing as they unwind.
Although the length of the System Readiness documents varies across states, some are detailed enough to illustrate the specific tests and scenarios that state IT workers are considering during this time. Louisiana and Kentucky are good examples of detailed System Readiness documents. Making documents publicly available is important, so advocates should consider reaching out to their state if these documents have not been published yet.
May 30 A survey of Medicaid enrollees, released by KFF last week, points to the need for enhanced outreach to help people either retain their coverage or to transition to other coverage that they might be eligible for.
Among KFF’s key findings:
- Most Medicaid enrollees were not aware that states are now permitted to resume disenrolling people from Medicaid. This could mean that people are not focused on renewal notices that states are starting to send out and may not realize that action is required.
- Nearly half of Medicaid enrollees say they have not previously been through the Medicaid renewal process, which was paused for three years. KFF points out that this group could be less likely to understand the importance of completing renewal forms to retain coverage.
These findings, coupled with early data revealing a high percentage of procedural terminations (which occur when someone doesn’t return renewal forms, for example; it does not mean they no longer meet eligibility criteria) underscore the need for the Centers on Medicare & Medicaid Services (CMS), states, and stakeholders to redouble efforts to communicate that current enrollees should watch their mail and take action, if needed, to renew their coverage.
CMS has posted various communication resources that states and stakeholders can use to communicate about eligibility determinations resuming. CBPP developed these community talking points. Other unwinding resources are also available from organizations such as Community Catalyst, Georgetown Center for Children and Families, and State Health and Values Strategies.
KFF also found that more than 4 in 10 people whose only coverage is Medicaid wouldn’t know where to look for other coverage if they lose Medicaid during unwinding or would end up uninsured. This also points to a need for increased education and outreach to help connect people to marketplace or employer sponsored coverage that could be available to them.
May 24 Data from early unwinding states give some reason for concern. Arkansas and Florida both terminated coverage for more than half of the enrollees for whom they completed renewals. The vast majority of those who lost coverage were terminated for procedural reasons ― meaning they didn’t submit the renewal form or other required documentation ― and not because they were determined to be no longer eligible for Medicaid. Both states said they prioritized initial redeterminations for enrollees they’ve identified as likely ineligible but had “protected” while the continuous coverage requirement was in effect. Indiana and Iowa similarly have very high rates of procedural terminations, while Arizona and Pennsylvania appear to be successfully renewing most of their enrollees.
More information is needed to fully understand these numbers. For example: will there be a spike in applications by eligible people who lost coverage and reapply? Are there stories of people not receiving notices or not being able to get through to call centers to complete their renewals? Such information would suggest that states need to increase their outreach efforts and scrutinize their operations to prevent high rates of procedural terminations. A high rate of procedural terminations might be less problematic in a state that also has a very high rate of ex parte (automated) renewals, because people who receive forms in the mail in those states are more likely to no longer be eligible and may choose to not return renewal forms.
Organizations such as Florida Health Justice Project are documenting compelling stories of situations where people are falling through the cracks, because Florida hasn’t expanded Medicaid or due to poor communication by the state. How Florida and other states respond to stories and other data in their own states will be telling as unwinding unfolds over the next year.
May 12 The Centers for Medicare & Medicaid Services (CMS) recently launched its Enrollment Assistance Personnel (EAP) program, which will provide outreach and assistance for people no longer eligible for Medicaid who need help transitioning to ACA marketplace coverage. The program will operate in 23 counties across 12 states (Ariz., Fla., Ill., La., Mich., Mont., N.C., Okla., S.D., Tenn., Texas, and Utah), and CMS anticipates the program will begin in earnest in June.
The EAP program, run by private contractor Cognosante, will supplement existing Navigators and enrollment assisters in these counties, conducting direct outreach, providing ACA marketplace application and enrollment assistance, and referring people to other organizations and resources when appropriate. In some states, Cognosante may also sub-contract with existing assister organizations.
CMS requires that EAP staff receive training at the same level as Navigators and observe the same consumer protections, including protection of personally identifiable information and a requirement to provide unbiased information about ACA marketplace plans. Like Navigators, EAP staff can’t recommend a specific marketplace plan and don’t receive commissions from health insurance companies.
May 1 A second group of 14 states have begun their first terminations of Medicaid coverage as part of unwinding the continuous coverage provision. Some enrollees in Connecticut, Florida, Indiana, Iowa, Kansas, Nebraska, New Mexico, Ohio, Oklahoma, Pennsylvania, Utah, Virginia, West Virginia, and Wyoming lost Medicaid coverage for the first time in over three years effective May 1. Arizona, Arkansas, Idaho, New Hampshire, and South Dakota terminated coverage for additional enrollees in May after beginning terminations in April.
We can expect to see data trickling in over the next couple of weeks that will begin to give an indication of outcomes in the first 19 states that started terminating coverage in April or May. States must submit reports to the Centers for Medicare & Medicaid Services (CMS) by May 8, and some of them will likely publicly post those reports after submitting them, as West Virginia has begun doing for prior months. Other states have dashboards with detailed unwinding data that may soon reflect April activity, including Iowa, Pennsylvania, Utah, and Virginia. And we expect CMS to begin releasing data on ex parte renewal rates and call center wait times across states sometime in June.
April 26 People who are no longer eligible for Medicaid following a redetermination may be eligible for Affordable Care Act (ACA) marketplace coverage with premium tax credits, but only if they do not currently have an offer of employer-sponsored insurance (ESI) that is considered affordable (employee share of premiums does not exceed 9.12 percent of income in 2023).
An estimated 3.8 million people losing Medicaid eligibility have ESI or an affordable offer of ESI, but they will need to act quickly to transition to ESI. Employers must provide people losing Medicaid or CHIP at least 60 days following loss of coverage to enroll in ESI (although they have the option to provide more time). If people miss this window, they qualify for the Unwinding Special Enrollment Period and can enroll in ACA marketplace coverage any time before July 31, 2024, but they do not qualify for premium tax credits or cost-sharing reductions to lower the cost of coverage and care.
For more information on helping people losing Medicaid/CHIP transition to ESI, see our FAQ: Transitioning from Medicaid to Employer-Sponsored Insurance.
April 5 A letter from the U.S. Department of Health and Human Services Office for Civil Rights (OCR) reminds state health officials of their obligations to provide people with limited English proficiency (LEP) and people with disabilities meaningful language access and effective communications to ensure those who remain eligible maintain access to coverage during unwinding.
Under long-standing anti-discrimination laws, all individuals must have an equal opportunity to participate in federally funded health programs, including Medicaid. This means states must provide communications to people with disabilities that are as effective as their communications with all other groups, and they must take reasonable steps to provide meaningful language access to people with LEP.
OCR’s letter provides examples of best practices and offers to provide technical assistance to states.
April 1 States can resume Medicaid coverage terminations as of April 1. Five states — Arizona, Arkansas, Idaho, New Hampshire, and South Dakota — have done so.
Unwinding enrollment data for these five states are pending. All states must submit reports with redetermination data each month to the U.S. Department of Health and Human Services.
The data will be made publicly available in the coming months and will include metrics such as the number of procedural terminations, rates of renewals conducted ex parte (that is, automatically), and state call center wait times. The reports will help stakeholders monitor states’ unwinding activities in this crucial period.
The month of a state’s first terminations depends on when they initiated the unwinding process. From here, we expect about 14 states to have their first set of terminations in May, 22 states in June, and nine states in July.