A temporary Arkansas policy that took Medicaid enrollees’ coverage away for not meeting onerous work-reporting requirements has, despite its many failures, continued to surface as a model for policymakers seeking to cut or limit access to Medicaid. House Republicans recently tried, unsuccessfully, to add a work-reporting requirement to Medicaid at the federal level. And after a federal judge vacated the Biden Administration’s decision to revoke Georgia’s Medicaid work-reporting requirement waiver, the state began implementing its policy in July, requiring a group of adults with low incomes to report 80 hours of work each month to keep Medicaid coverage.[1]
The Arkansas policy was a failure in many respects:
- The work-reporting requirement harmed thousands of people by taking away their health coverage, leaving many uninsured. It harmed thousands of others by requiring them to live under the ongoing stress of potential coverage loss.
- People who were supposed to be exempted from submitting monthly proof of their work hours were not always shielded from losing coverage.
- The requirement imposed extreme levels of red tape on targeted Medicaid enrollees, resulting in coverage losses and no increases in employment.
The experience in Arkansas shows why similar policies should not be implemented at the federal or state level. Work-reporting requirements do not increase employment but are very effective at kicking people off coverage due to excessive red tape and paperwork. Justifications for work requirements rest on the false assumptions that people who receive benefits do not work and must be compelled to do so. These assumptions are rooted in stereotypes based on race, gender, disability status, and class. They ignore the realities of the low-paid labor market, the lack of child care and paid sick and family leave, how health and disability issues and the need to care for family members affect people’s lives, and ongoing labor market discrimination.[2] They also ignore the research that shows that most people on Medicaid are already working or would meet an exemption.
In the first seven months of the Arkansas Medicaid work-reporting requirement, 18,000 people — or 1 in 4 of those subject to the requirement — lost coverage. Only a very small share regained coverage the next year.
But it is not just the data that demonstrate the policy’s failures. Testimonials from people subject to the reporting requirement reveal a confusing, onerous system that also fails in its supposed purpose of encouraging work; focus groups found that most were already working or looking for work and were highly motivated to work as much as they could. And even if that weren’t the case, taking people’s health coverage is not the solution to labor market realities beyond their control. Everyone needs enough resources to afford basics like health care, and Medicaid provides valuable assistance that helps people stay covered and healthy as they position themselves to thrive.
Medicaid does not include any requirements to report work as a condition of gaining or retaining coverage. During the Trump Administration, however, 13 states received approval to implement section 1115 demonstrations, or waivers, to require some Medicaid enrollees to report a certain number of hours of “community engagement” activities every month, or else lose their coverage.[3] Most of these waivers were not implemented due to courts striking them down as contrary to Medicaid’s central objective, or to the state deciding to postpone or suspend them. Arkansas was the only state to take Medicaid coverage away from people under a work-reporting requirement before a court invalidated the waiver.
At the time Arkansas requested federal permission to add a Medicaid work-reporting requirement, the state had an existing Medicaid waiver that allowed the state to use Medicaid funds to pay for private marketplace plans for adults eligible under the Affordable Care Act Medicaid expansion (people aged 19-64 who had incomes below 138 percent of poverty, or about $28,000 for a family of three based on 2018 poverty guidelines). The state amended that waiver — known as ArkansasWorks, or ARWorks — to add a “community engagement” reporting requirement beginning on June 1, 2018 for ARWorks enrollees aged 19-49.[4] Because the Arkansas requirement only applied to the Medicaid expansion population, some enrollees (such as people enrolled through a disability pathway or parents with very low incomes) didn’t have to report work or seek an exemption.
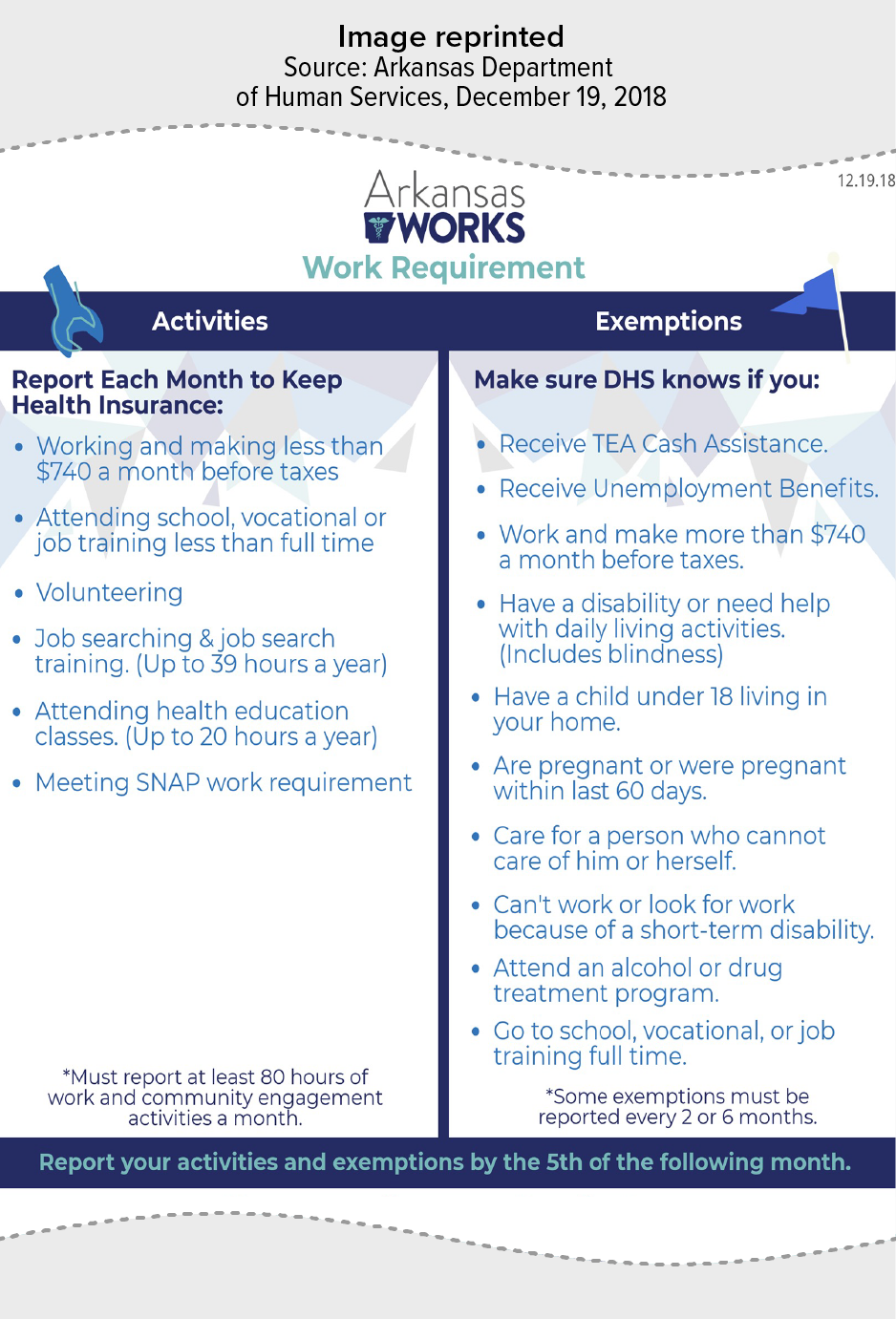
Below is an overview of how the requirement was structured in Arkansas:[5]
- ARWorks enrollees under age 50 had to report that they completed at least 80 hours of qualifying activities each month or had an exemption in any given month. (See Figure 1 for a list of qualifying activities and exemptions.)
- Reporting a month’s hours had to be completed through an online portal or phone (the phone option was not added until December 2018) by the 5th of the following month. Exemptions could be reported by phone or online at any time.
- If someone went three months in a calendar year (consecutive or non-consecutive) without a completed report showing at least 80 hours of qualifying activities, the state could disenroll them for the remainder of the calendar year. The date of disenrollment was the first day of the month after a notice was sent, unless the enrollee filed an appeal or reported a “good cause exemption.”[6]
- People who were disenrolled had to wait until the following plan year to apply to reenroll in Medicaid, unless they qualified through another pathway, meaning that people could be locked out of coverage for up to nine months.
- The state used data from the ARWorks application process or other system data to identify people who qualified for an exemption, though some people receiving exemptions had to actively renew them often.[7] Some examples of data used include exemptions from work requirements under the Supplemental Nutrition Assistance Program, receipt of unemployment benefits, prior determination of medical frailty, or the use of workforce services agency data to identify people already working 80 hours or more a month.[8] There were 171,449 ARWorks enrollees aged 19-49 as of March 2, 2018. About 69,000 of them did not have an exemption identified through the data, meaning they would have to report work or request an exemption on their own to avoid losing coverage. For example, people with certain medical conditions had to pursue an exemption as “medically frail” if they had not already been determined as such.
In the first seven months of the Arkansas Medicaid work reporting requirement, 18,000 people — or 1 in 4 of those subject to the requirement — lost coverage.[9] Arkansas enrollees who lost Medicaid coverage in 2018 were unlikely to get Medicaid coverage the following year. Only 11 percent of the people who lost Medicaid coverage in 2018 regained it in 2019.[10] Some may have enrolled in other coverage, but a portion likely became uninsured. A survey of Arkansas residents aged 30-49 who reported disenrolling from Medicaid or the marketplace in 2018 found that 26 percent were uninsured in late 2019.[11]
Losing health coverage keeps people from getting the care they need when they need it and also can contribute to greater financial instability. Half of Arkansas residents aged 30-49 who lost Medicaid or marketplace coverage in 2018 reported having serious problems paying off medical debt. Most of the people in that group also reported delaying necessary care or not taking their medications because of cost.[12]
In focus groups with people who lost coverage in Arkansas,[13] most participants said they did not know their Medicaid coverage was terminated until they were seeking care or picking up a prescription. This caused a lot of mental and financial stress for people:
I woke up from seizures in the hospital and one day my Medicaid was active and the next day it wasn’t. When you wake up from a seizure you are already disoriented and then you are telling me I have to pay out of pocket before being seen? — Urban Institute focus group participant, May 2019
Focus group participants cited worsening of their health conditions, higher stress, and hindrances to work:
I have to have my medication because I am epileptic, and I take three different seizure medicines. If I don’t take it, I can’t work…. I had to be stable and if I was not stable I was going to lose my job. — Urban Institute focus group participant, May 2019
Other people who did not lose their coverage (including younger adults who would have been subject to the work-reporting requirement later, had it not been struck down) were worried about keeping up with ongoing monthly reporting given other demands in their lives. They were also afraid that unexpected events could cause themselves or others to lose coverage and face harsh consequences:
My mom said I need to go online and do this and do that…. I was on the phone with a lady trying to, she said I needed to do something with my hours…. Well I was on the phone with the lady for like an hour, then she sent me to someone else, then she sent me to someone else. So it just…I just gave up from trying to report my hours worked. — KFF and PerryUndem focus group participant, November 2018
Some people who should have been exempted based on the program rules in Arkansas were not given initial exemptions based on the state’s data matching process, putting them at high risk of losing coverage. And those who did receive initial automatic exemptions had to actively renew them as often as every two months or they would lose that exemption.
Enrollees, health care providers, and other stakeholders raised concerns about people falling through the cracks, or witnessed people who did. That was especially the case for people with medical conditions that prevented them from working.[14] In the 2019 Urban Institute focus groups, two providers said they had patients with disabilities who should have been exempted but were not and lost coverage.
Exemptions were supposed to be available to, for example: parents and others living with a dependent child under the age of 18, full-time students, people participating in a treatment program for a substance use disorder, and people medically certified as “unfit for employment.” (See Figure 1 for exemption list.) Enrollees were who not automatically exempted by the state’s data matching could apply for an exemption at any time using the online portal (a phone option was not added until later).
In addition to the list of specified exemptions, people could request good cause exemptions if they had a temporary circumstance preventing them from reporting or completing 80 hours a month. However, very few people made these good cause requests, suggesting a lack of understanding of the process. And a third of the requests were related to a disability or serious health issue, showing that people who should have been shielded were still at risk.[15]
People were confused because of the different types of exemptions that were available and varying timelines for re-verifying different exemptions. Some exemptions lasted until the situation changed, but several were as short as two months (for example, participating in treatment for alcohol or drug addiction or having a short-term disability that keeps you from working) or six months (for example, attending school full time or receiving unemployment benefits).
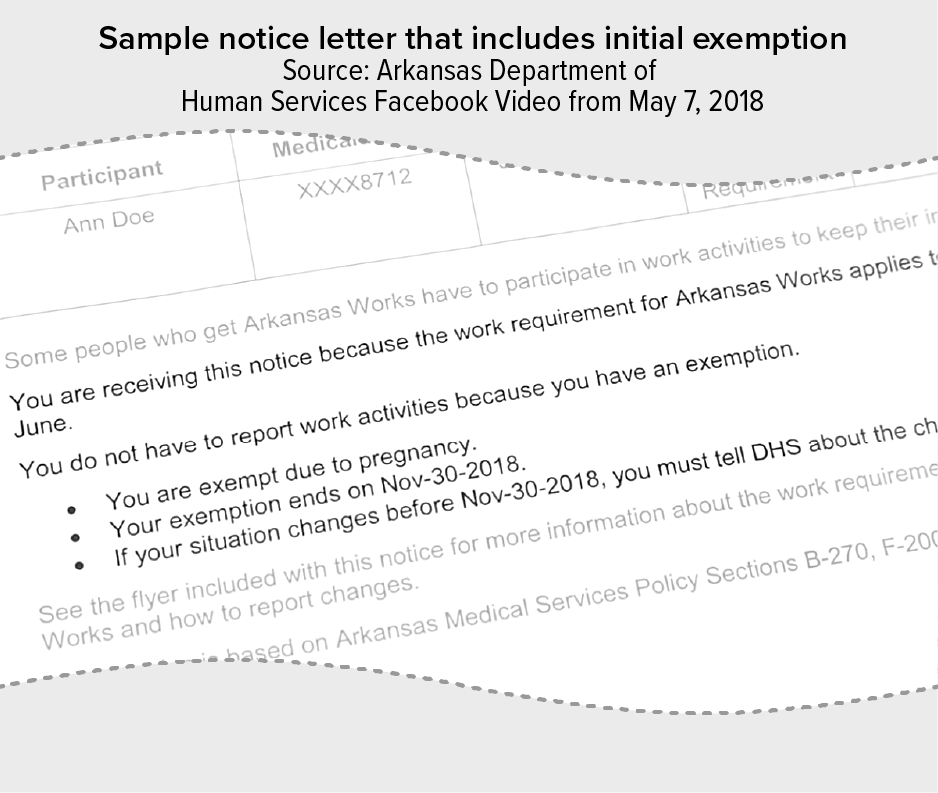
In a sample notice letter (see Figure 2), the “action” box says the person is subject to the work requirement, but the letter also says they have an exemption due to pregnancy (but only until the end of the official 60-day postpartum coverage period in November 2018). One participant in a focus group convened by KFF said she was confused by seeing the letter’s two conflicting statements on the same page.[16] In the Urban Institute focus groups, a participant commented on the confusing exemption timeliness:
One problem is you go [online] to put things in, and it might need you to do it the next month, and then sometimes I wouldn’t have to do it for two or three months…. They [should] send you an email or text to tell you how long the exemption lasts.
The requirement was complex and many people were unsure if the requirement applied to them. Among people who were not exempt from the requirement and did not report 80 hours in a given month, almost 99 percent reported zero activities.[17] That is a strong indicator that many people did not understand they were subject to the work-reporting requirement or were deterred by the difficulties of reporting.
Large numbers of people lost Medicaid for administrative reasons (a term called “administrative denials”) — not because they were not working. This is consistent with national estimates showing that in 2021, 9 in 10 Medicaid adults who could be subject to a work-reporting requirement were already working or would meet an exemption.[18] This finding also supports research showing that many people had not heard about the requirement, were unsure if they received a letter in the mail notifying them about whether they were subject to the requirement or exempt, were already overwhelmed with stressful life events, or were concerned about their or others’ online access and skills.[19]
“Half my family probably doesn’t have a smart phone…. A lot of people here don’t have internet still,” a 19-year-old woman explained in an interview. Her 47-year-old mother-in-law struggled using the portal: “She had to do it online or something, and she didn’t like it at all.”[20]
Before the phone option was made available in December 2018, enrollees had to create an online account to report their hours or an exemption. The online reporting system was a major barrier for people who did not have consistent internet access. Arkansas ranked near the bottom for broadband access at the time of the waiver implementation.[21]
People who did have internet access also faced challenges with navigating the website, with setting up an account, and with the limited hours the site operated (the state’s web portal was unavailable for part of the day). One focus group participant said it took more than ten-and-a-half hours to set up an account, even with the help of a friend who shared their computer.[22] And even when the phone option was added, there were long wait times and people commented on the staff being condescending or not helpful in getting the report done.
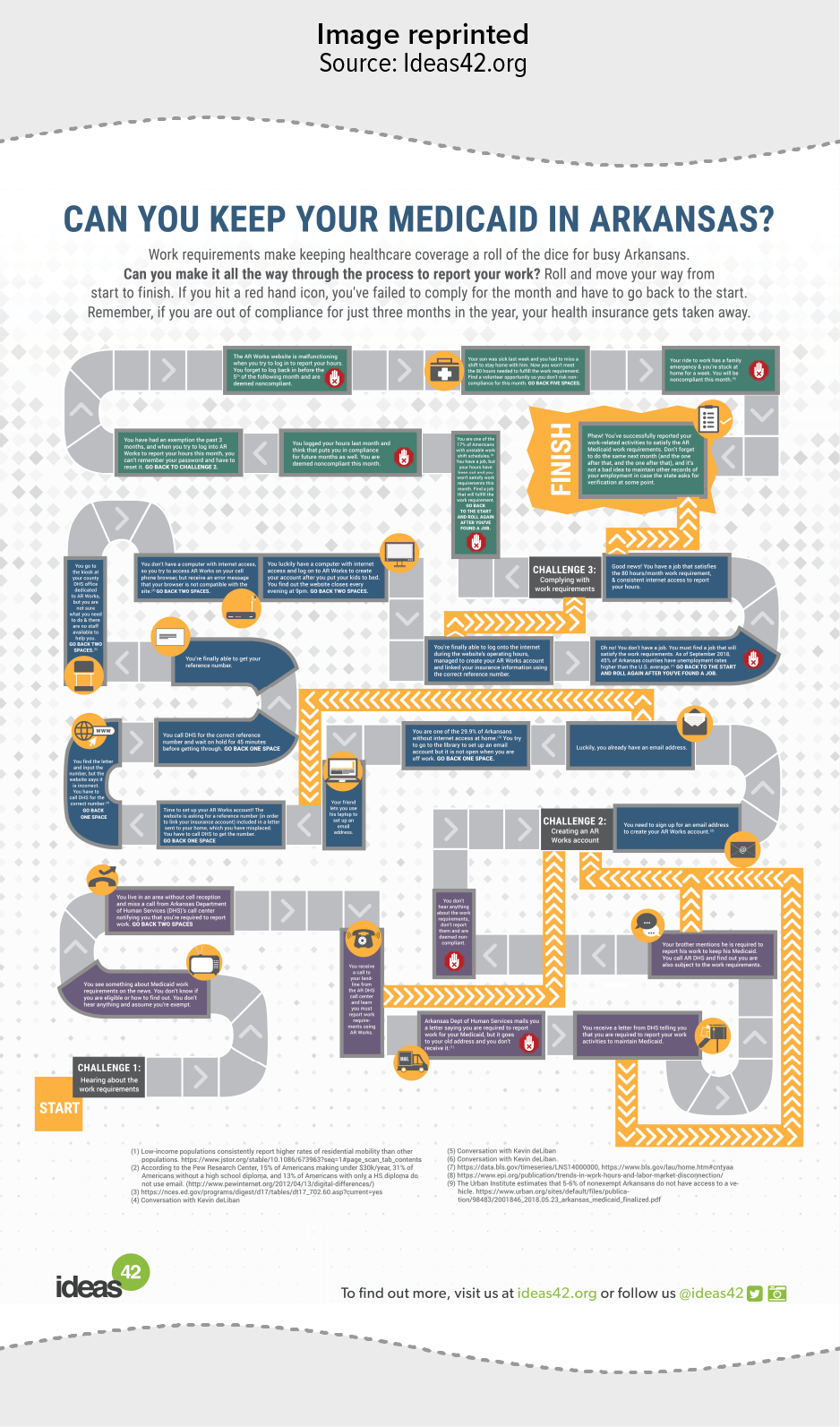
The scenario outlined in an elaborate board game created by ideas42 shows some of the difficulties that people faced — finding out about the requirement, setting up an online account, and linking the account with their insurance information — just to get to the point where they could report work hours.[23] (See Appendix.)
The state relied largely on mailed notices and phone calls to inform people whether they were subject to the requirement or exempt. Some key informants interviewed noted the lack of diversity of outreach methods, such as not using trusted partners in the community to share information. The higher reliance on more traditional methods meant that some people, especially college students and people with unstable housing, who were more likely to have frequent changes in their address, were also less likely to receive notices.[24] State agency officials reported that the agency received a high volume of returned and undelivered mail.[25]
Many enrollees who were successfully reached agreed that information was not communicated clearly. The state made an effort to improve the readability of their materials while the waiver was in place, but enrollees and other stakeholders like health care providers and case managers agreed that the materials were confusing.[26] Some confusion also arose from the letters being long and confusing — with some key information not appearing until the second page or being spread across multiple notices.
Trying to comprehend these notices, and the requirements generally, while dealing with pressing needs led many to feel overwhelmed or defeated:
I only skimmed through [the notice] and picked up [that] I had to do the 80 hours a month or something and then I set it down…. It didn’t say nothing about opening an account.” — KFF and PerryUndem focus group participant, November 2018
I don’t know about it…I guess it goes over my head. I am oblivious to it. — Urban Institute focus group participant, May 2019
It is hard enough for me to get a job.… I have a part-time job but when they added on all this…. It is a big hassle.” — Urban Institute focus group participant, May 2019
The Arkansas requirement did not result in any significant changes to employment or number of hours worked between 2018 and late 2019 (after which the work requirement was put on hold).[27] Focus groups with participants found that most were already working or looking for work and were highly motivated to work as much as they could because of financial pressures they were already experiencing.[28]
The state worked to connect people with job search and training programs by referring ARWorks enrollees to the state’s workforce services agency. But the programs were not accessible, and the broader outreach issues led to relatively low usage of the services among enrollees. At the time, there were just 37 workforce centers for the state’s 75 counties.[29] One enrollee who was looking for work said they could not get to the state’s workforce services office because it was 30 miles away and there was no public transportation.[30]
And for people who lost coverage for not reporting hours, they ended up in a vicious cycle where they may end up too unwell to find or keep a job. An enrollee in Arkansas shared his story about finding out his coverage was terminated while trying to pick up a prescription for his chronic illness. He couldn’t afford the medication and ended up missing a lot of work due to complications of his illness, so he lost his job.[31] Adding more red tape to the process of getting health care is the last thing people need when seeking employment or training opportunities.
Everyone needs enough resources to afford the basics including food, housing, and health care. Making people go through the extra steps involved in monthly reporting to keep their Medicaid coverage is just an attempt to trip people up with more paperwork and, ultimately, to cut Medicaid — the country’s single largest source of health coverage.[32]
As we saw in Arkansas, work-reporting requirements would leave more people without the health care they need, without increasing employment and instead making it harder for people to meet their basic needs and to find and keep work. Arkansans who were subject to Medicaid work-reporting requirements shared that they had more stress and anxiety in their lives as they worried about being able to keep their coverage. And those who lost coverage had to delay care due to cost or got sicker and had a hard time continuing to work. These real-life experiences show why this policy is misguided and should not be a model at the state or national level.