SNAP Is Linked With Improved Health Outcomes and Lower Health Care Costs
End Notes
[1] Steven Carlson is a research analyst who previously directed the Office of Policy Support at the Agriculture Department’s Food and Nutrition Service. The opinions and conclusions expressed in this report are solely those of the authors and should not be construed as representing the views of the Agriculture Department.
[2] Estimated fiscal year 2023 benefits exclude temporary, pandemic-related increases and are based on a CBPP analysis of fiscal year 2019 SNAP household characteristics data. They reflect the U.S. Department of Agriculture’s (USDA) recent revision to the Thrifty Food Plan, which is used to set the amount of food assistance that households participating in SNAP receive. See Appendix I, Impact of Updated Thrifty Food Plan.
[3] Paula Braveman, Susan Egerter, and David R. Williams, “The Social Determinants of Health: Coming of Age,” Annual Review of Public Health, 32: 381-98, 2011, http://www.annualreviews.org/doi/pdf/10.1146/annurev-publhealth-031210-101218; Nancy E. Adler et al., “Addressing Social Determinants of Health and Health Disparities,” Vital Directions for Health and Health Care Series, National Academy of Medicine, September 19, 2016, https://nam.edu/wp-content/uploads/2016/09/Addressing-Social-Determinants-of-Health-and-Health-Disparities.pdf.
[4] Raj Chetty et al., “The Association Between Income and Life Expectancy in the United States, 2001-2014,” Journal of the American Medical Association, 315(16): 1750-1766, 2016.
[5] Dhruv Khullar and Dave A. Chokshi, “Health, Income, & Poverty: Where We Are & What Could Help,” Health Affairs Policy Brief, October 2018, https://www.healthaffairs.org/do/10.1377/hpb20180817.901935/full/HPB_2017_RWJF_05_W.pdf.
[6] Andrew Knighton, Brad Stephenson, and Lucy Savitz, “Measuring the Effect of Social Determinants on Patient Outcomes: A Systematic Literature Review,” Journal of Health Care for the Poor and Underserved, 29(1): 81-106, 2018 https://muse.jhu.edu/article/686956/summary.
[7] Brian Smedley, Adrienne Stith, and Alan Nelson, eds., Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care, National Academy Press, 2003, https://www.ncbi.nlm.nih.gov/books/NBK220358/.
[8] See, for example, William Mude et al., “Racial disparities in COVID-19 Pandemic Cases, Hospitalisations, and Deaths: A Systematic Review and Meta-analysis,” Journal of Global Health, 11: 05015, 2021, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8248751/.
[9] See, for example, Ozge Bahar et al., “‘Like, What Else Could Go Wrong?’ Multiple Contextual Stressors in Food Insecure Households,” Journal of Poverty, 25(4): 386-407, 2021, https://www.tandfonline.com/doi/abs/10.1080/10875549.2020.1840485; and Angela Odoms-Young, “Structural and Social Adversity and Food Insecurity in Families with Young Children: A Qualitative Metasynthesis,” in Families, Food, and Parenting, 2021, https://link.springer.com/chapter/10.1007/978-3-030-56458-2_1.
[10] Richard Wilkinson and Michael Marmot, “Social Determinants of Health: The Solid Facts,” World Health Organization, 2003 (2nd edition), http://www.euro.who.int/__data/assets/pdf_file/0005/98438/e81384.pdf. There is some suggestive, if not conclusive, evidence of the cumulative effect of multiple adverse experiences (such as loss of a parent through separation, divorce, or incarceration; witnessing neighborhood violence; or exposure to alcohol or drug abuse) in early childhood on food insecurity. While young children exposed to a single experience are about twice as likely to experience food insecurity, those exposed to more than one are about four times as likely. See Philip Baiden et al., “Adverse Childhood Experiences and Household Food Insecurity Among Children Aged 0–5 Years in the USA,” Public Health Nutrition, 24(8): 2123-2131, 2021, https://www.cambridge.org/core/journals/public-health-nutrition/article/adverse-childhood-experiences-and-household-food-insecurity-among-children-aged-05-years-in-the-usa/D7E980439685D1FB2ACA0D881FE1384E.
[11] For summaries of the extensive research on the health consequences of food insecurity, see Barbara A. Laraia, “Food Insecurity and Chronic Disease,” Advances in Nutrition: An International Review Journal, 4(2): 203-212, 2013, http://advances.nutrition.org/content/4/2/203.full; Craig Gundersen and James Ziliak, “Food Insecurity and Health Outcomes,” Health Affairs, 34(11): 1830-1839, 2015, http://gattonweb.uky.edu/Faculty/Ziliak/GZ_HealthAffairs_34(11)_2015.pdf; Daniel Arenas et al., “Negative Health Outcomes Associated with Food Insecurity Status in the United States of America: a Systematic Review of Peer-Reviewed Studies,” September 2018, https://osf.io/preprints/nutrixiv/uk9xw/; and Lesley Weaver and Connor Fasel, “A Systematic Review of the Literature on the Relationships Between Chronic Diseases and Food Insecurity,” Food and Nutrition Sciences, 9(5): 519-541, 2018, https://www.scirp.org/html/7-2702276_84666.htm?pagespeed=noscript.
[12] Alisha Coleman-Jensen, William McFall, and Mark Nord, “Food Insecurity in Households with Children,” Economic Research Service, USDA, May 2013, https://www.ers.usda.gov/webdocs/publications/43763/37672_eib-113.pdf?v=41424; Klébya de Oliveira et al., “Household Food Insecurity and Early Childhood Development: Systematic Review and Meta‐Analysis,” Maternal & Child Nutrition, 16(3): e12967, 2020, https://onlinelibrary.wiley.com/doi/full/10.1111/mcn.12967; and Shannon Simonovich et al., “A Systematic Review Examining the Relationship Between Food Insecurity and Early Childhood Physiological Health Outcomes,” Translational Behavioral Medicine, 10(5): 1086-1097, 2020, https://academic.oup.com/tbm/article-abstract/10/5/1086/5921050.
[13] Jason Nagata et al., “Food Insecurity and Chronic Disease in US Young Adults: Findings from the National Longitudinal Study of Adolescent to Adult Health,” Journal of General Internal Medicine, 34(12): 2756-2762, 2019, https://link.springer.com/article/10.1007/s11606-019-05317-8.
[14] Laraia, op. cit.; Gundersen and Ziliak, op. cit.; and Jennifer Te Vazquez et al., “Food Insecurity and Cardiometabolic Conditions: A Review of Recent Research,” Current Nutrition Reports, 10: 243-254, 2021, https://link.springer.com/article/10.1007/s13668-021-00364-2.
[15] Laraia, op. cit; Gundersen and Ziliak, op. cit.
[16] John T. Cook et al., “Are Food Insecurity’s Health Impacts Underestimated in the U.S. Population? Marginal Food Security Also Predicts Adverse Health Outcomes in Young U.S. Children and Mothers,” Advances in Nutrition: An International Review Journal, 4(1): 51-61, 2013, http://advances.nutrition.org/content/4/1/51.long; and Kayoung Lee, “Household Marginal Food Security Is Associated with Poorer Self-Rated Health in Korean Adults,” Nutrition Research, 10: 33-41, 2022, https://www.sciencedirect.com/science/article/abs/pii/S0271531722000021.
[17] Daphne Hernandez and Alison Jacknowitz, “Transient, but Not Persistent, Adult Food Insecurity Influences Toddler Development,” Journal of Nutrition, 139(8): 1517-1524, 2009, https://academic.oup.com/jn/article/139/8/1517/4670506?login=false; and Rachel Kimbro and Justin Denney, “Transitions Into Food Insecurity Associated with Behavioral Problems and Worse Overall Health Among Children,” Health Affairs, 34(11): 1949-1955, 2015, https://www.healthaffairs.org/action/showCitFormats?doi=10.1377%2Fhlthaff.2015.0626.
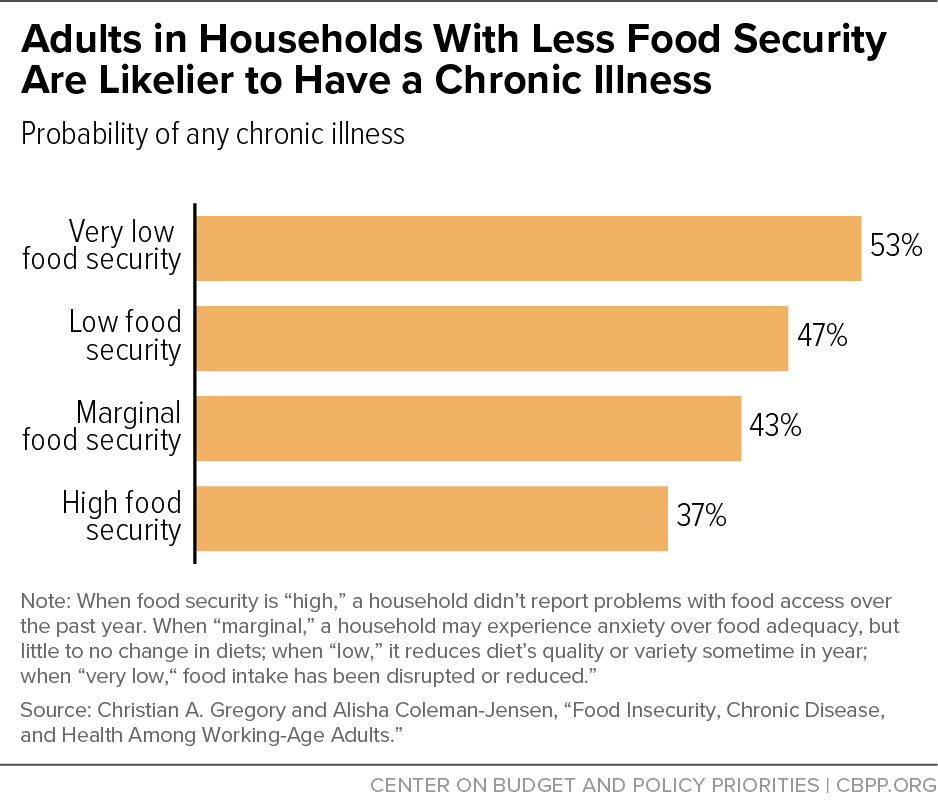
[18] Christian A. Gregory and Alisha Coleman-Jensen, “Food Insecurity, Chronic Disease, and Health Among Working-Age Adults,” Economic Research Service, USDA, July 2017, https://www.ers.usda.gov/webdocs/publications/84467/err-235.pdf?v=42942.
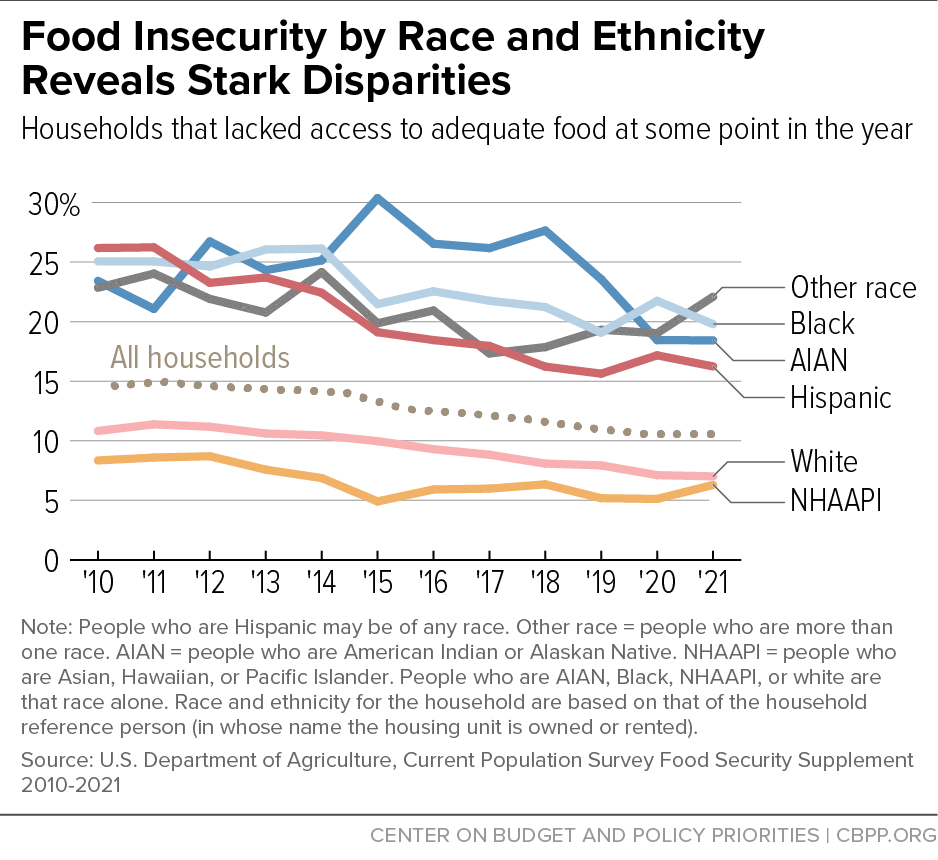
[19] Alisha Coleman-Jensen et al., “Household Food Security in the United States in 2021,” Economic Research Service, USDA, September 2022, https://www.ers.usda.gov/publications/pub-details/?pubid=104655. Note that household race and ethnicity is based on the race and ethnicity reported by the household reference person (in whose name the housing unit is owned or rented).
[20] Margaret Thomas, Daniel Miller, and Taryn Morrissey, “Food Insecurity and Child Health,” Pediatrics, 144(4): 2019, https://www.publications.aap.org/pediatrics/article-split/144/4/e20190397/38475/Food-Insecurity-and-Child-Health; and Craig Gundersen and Brent Kreider, “Bounding the Effects of Food Insecurity on Children’s Health Outcomes,” Journal of Health Economics, 28(5): 971-983, (2009), https://www.sciencedirect.com/science/article/abs/pii/S0167629609000708.
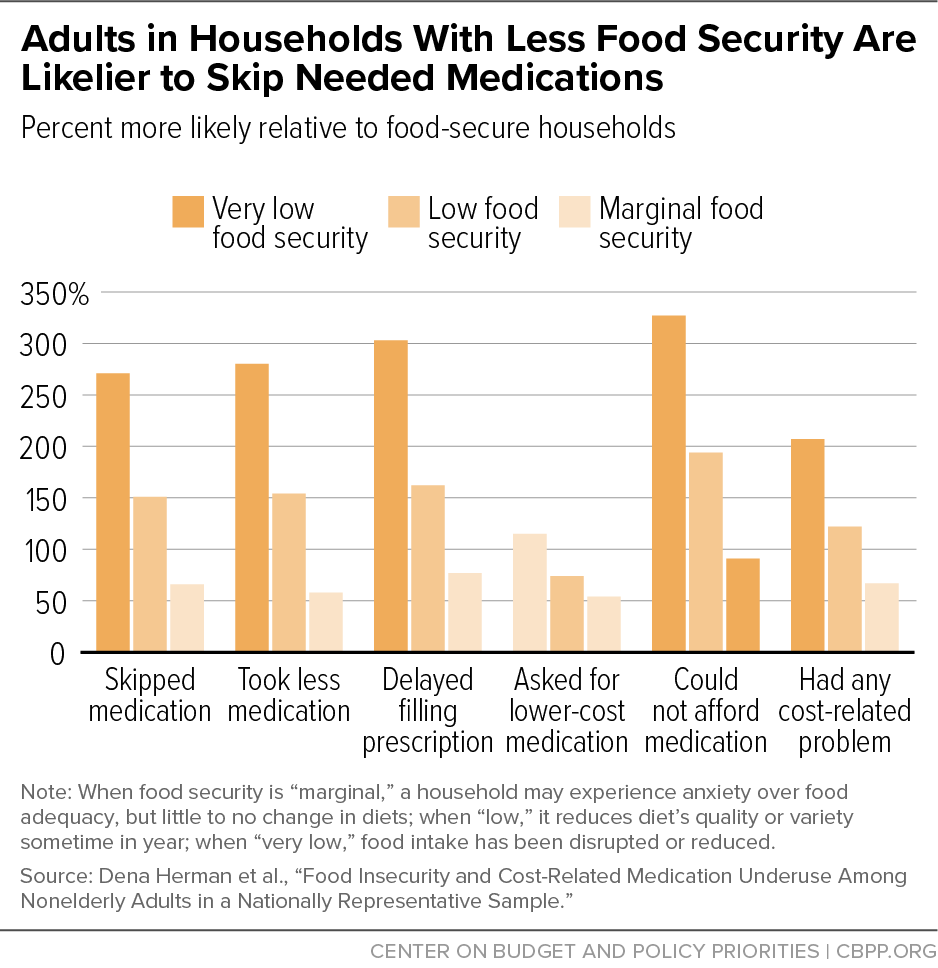
[21] Dena Herman et al., “Food Insecurity and Cost-Related Medication Underuse Among Nonelderly Adults in a Nationally Representative Sample,” American Journal of Public Health, 105(10): e48-e59, October 2015, http://ajph.aphapublications.org/doi/full/10.2105/AJPH.2015.302712.
[22] See, for example, Seth A. Berkowitz, Hilary K. Seligman, and Niteesh K. Choudhry, “Treat or Eat: Food Insecurity, Cost-Related Medication Underuse, and Unmet Needs,” American Journal of Medicine, 127(4): 303-310, 2014, http://www.amjmed.com/article/S0002-9343(14)00030-8/fulltext; Chadwick K. Knight et al., “Household food insecurity and medication ‘scrimping’ among US adults with diabetes,” Preventive Medicine, 83: 41-45, February 2016, http://www.sciencedirect.com/science/article/pii/S0091743515003679; Minal R. Patel et al., “Social determinants of health, cost-related nonadherence, and cost-reducing behaviors among adults with diabetes: findings from the National Health Interview Survey,” Medical Care, 54(8): 796-803, August 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4945373/; Patience Afulani et al., “Food Insecurity and Health Outcomes Among Older Adults: The Role of Cost-Related Medication Underuse,” Journal of Nutrition in Gerontology and Geriatrics, 34(3): 319-342, August 12, 2015, http://www.tandfonline.com/doi/abs/10.1080/21551197.2015.1054575; and Brittany Imel and Heather McClintock, "Food Security and Medication Adherence in Young and Middle-Aged Adults with Diabetes," Behavioral Medicine, published online October 25, 2021, https://www.tandfonline.com/doi/abs/10.1080/08964289.2021.1987855.
[23] Herman et al. Researchers found an even steeper gradient among Canadian adults under a different system of health care insurance and prescription drug coverage. After adjusting for differences in socio-demographic characteristics, adults from marginally, moderately, and severely food-insecure households were nearly twice, nearly four times, and about five times more likely, respectively, to delay or not fill prescriptions and skip or reduce doses relative to their food-secure counterparts. See Fei Men et al., “Prescription Medication Nonadherence Associated with Food Insecurity: A Population-Based Cross-Sectional Study,” Canadian Medical Association Open Access Journal, 7(3): E590-E597, 2019 https://www.cmajopen.ca/content/cmajo/7/3/E590.full.pdf.
[24] Zhiwen Xie et al., “Racial and Ethnic Disparities in Medication Adherence Among Privately Insured Patients in the United States,” PLoS One, 14(2): e0212117, 2019, https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0212117.
[25] Though fraught with uncertainty, estimates of the annual economic cost of poor health, illness, and health care associated with food insecurity in the United States range from over $40 billion to as much as $160 billion. See Donald S. Shepard, Elizabeth Setren, and Donna Cooper, “Hunger in America: Suffering We All Pay For,” Center for American Progress, October 2011, https://www.americanprogress.org/article/hunger-in-america/; John T. Cook and Ana Paula Poblacion, “Estimating the Health-Related Costs of Food Insecurity and Hunger,” in The Nourishing Effect: Ending Hunger, Improving Health, Reducing Inequality, Bread for the World, 2016, http://childrenshealthwatch.org/wp-content/uploads/JohnCook_cost_of_hunger_study.pdf, and Seth Berkowitz et al., “State-Level and County-Level Estimates of Health Care Costs Associated with Food Insecurity,” Preventing Chronic Disease, 16(E90), 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6741857/pdf/PCD-16-E90.pdf.
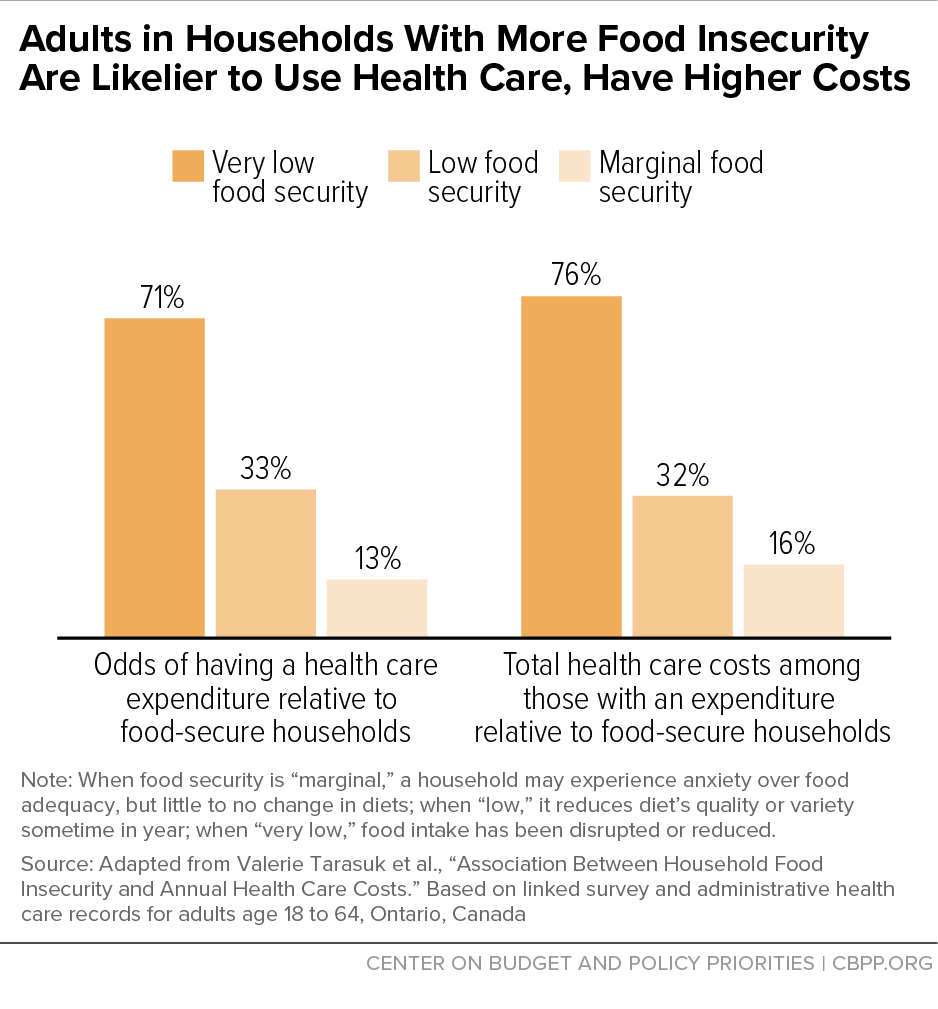
[26] Valerie Tarasuk et al., “Association Between Household Food Insecurity and Annual Health Care Costs,” Canadian Medical Association Journal, 187(14): E429-E436, October 6, 2015, http://www.cmaj.ca/content/187/14/E429. Note that the Canadian classifications (marginal, moderate, and severe) differ from those used to monitor food security in the United States (food insecure and very low food security), though both measures are based on the same set of questions. The authors also report results that include prescription drug benefits. Because these benefits are available only to low-income households in Ontario, and having low income is a strong predictor of food insecurity, their inclusion is likely to confound (and probably overstate) the association between food insecurity and health care costs. As expected, the inclusion of prescription drug costs results in even greater differences in total health care expenditures: 49 percent higher for households with moderate food insecurity and 121 percent higher for those with severe food insecurity.
[27] Fei Men et al., “Food Insecurity Is Associated with Higher Health Care Use and Costs Among Canadian Adults,” Health Affairs, 39(8): 1377-1385, 2020, https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2019.01637.
[28] Seth A. Berkowitz et al., “Food Insecurity and Health Care Expenditures in the United States, 2011-2013,” Health Services Research, 53(3): 1600-1620, 2018, http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12730/full. Subsequent research suggests that higher health care spending varies substantially across states and counties, primarily because of differences in the number of food-insecure adults. Per capita spending based on each state’s entire population, not just those who are food insecure, ranges from a high of $243 in Mississippi to a low of $78 in North Dakota. See Berkowitz et al., 2019, op. cit.
[29] Tiffany Fitzpatrick et al., “Looking Beyond Income and Education: Socioeconomic Status Gradients Among Future High-Cost Users of Health Care,” American Journal of Preventive Medicine, 49(2): 161-171, 2015, https://www.sciencedirect.com/science/article/pii/S0749379715000823.
[30] A study using a more nuanced categorization of food security and contemporaneous measures of food security and medical expenditures generally aligns with the conclusion that the use and cost of health care increase as household food insecurity increases. When controls for chronic health conditions are incorporated, however, the differences across food security groups largely dissipate, suggesting that underlying differences in health status may be an important factor in the relationship between food insecurity and health care costs. See Emma Boswell Dean, Michael French, and Karoline Mortensen, “Food Insecurity, Health Care Utilization, and Health Care Expenditures,” Health Services Research, 55(Suppl.2): 883-893, 2020, https://onlinelibrary.wiley.com/doi/pdfdirect/10.1111/1475-6773.13283.
[31] Karl Johnson et al., “Examining the Bidirectional Relationship Between Food Insecurity and Healthcare Spending,” Health Services Research, 56(5): 864-873, 2021, https://onlinelibrary.wiley.com/doi/full/10.1111/1475-6773.13641. It is worth noting that this study determined food security status only once based on a household’s food-related problems in the 30 days before the survey interview took place. Food security, however, can change from month to month as a family’s circumstances improve or worsen. As a result, the question of whether, and how much, the duration of exposure to food insecurity matters for subsequent health care expenditures remains unanswered.
[32] Christine Ma, Lauren Gee, and Margot Kushel, “Associations Between Housing Instability and Food Insecurity with Health Care Access in Low-Income Children,” Ambulatory Pediatrics, 8(1): 50-57, 2008, https://www.sciencedirect.com/science/article/abs/pii/S1530156707001554; and Alon Peltz and Arvin Garg, “Food Insecurity and Health Care Use,” Pediatrics, 144(4): e20190347, 2019, https://publications.aap.org/pediatrics/article/144/4/e20190347/76973/Food-Insecurity-and-Health-Care-Use.
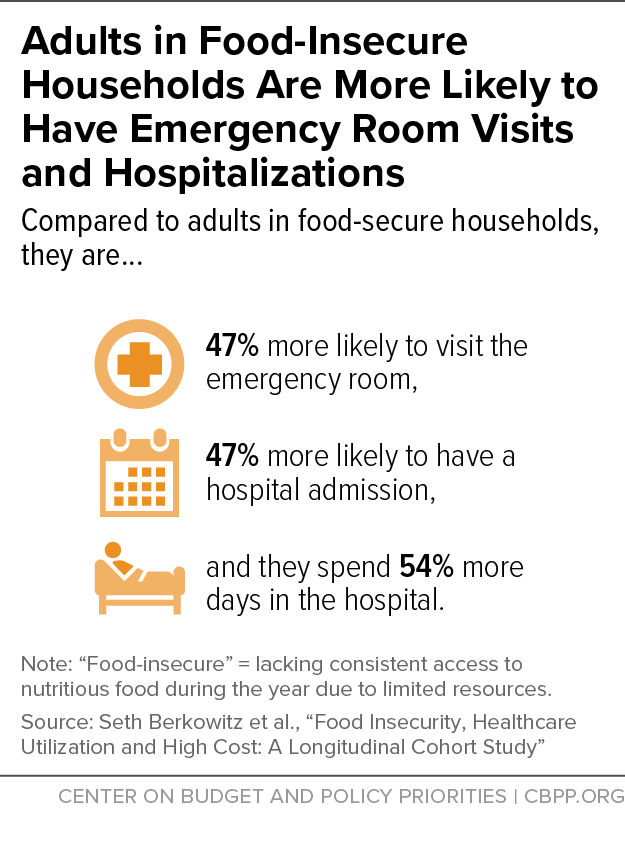
[33] Seth Berkowitz et al., “Food Insecurity, Healthcare Utilization and High Cost: A Longitudinal Cohort Study,” American Journal of Managed Care, 24(9): 399-404, 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6426124/pdf/nihms-1000556.pdf.
[34] Vibha Bhargava and Jung Sun Lee, “Food Insecurity and Health Care Utilization Among Older Adults in the United States,” Journal of Nutrition in Gerontology and Geriatrics, 35(3):177-192, 2016, http://www.tandfonline.com/doi/abs/10.1080/21551197.2016.1200334; Ariella Spitzer, Marisa Shenk, and James Mabli, “Food Insecurity is Directly Associated with the Use of Health Services for Adverse Health Events among Older Adults,” Journal of Nutrition, 150(12): 3152-3160, 2020, https://doi.org/10.1093/jn/nxaa286.
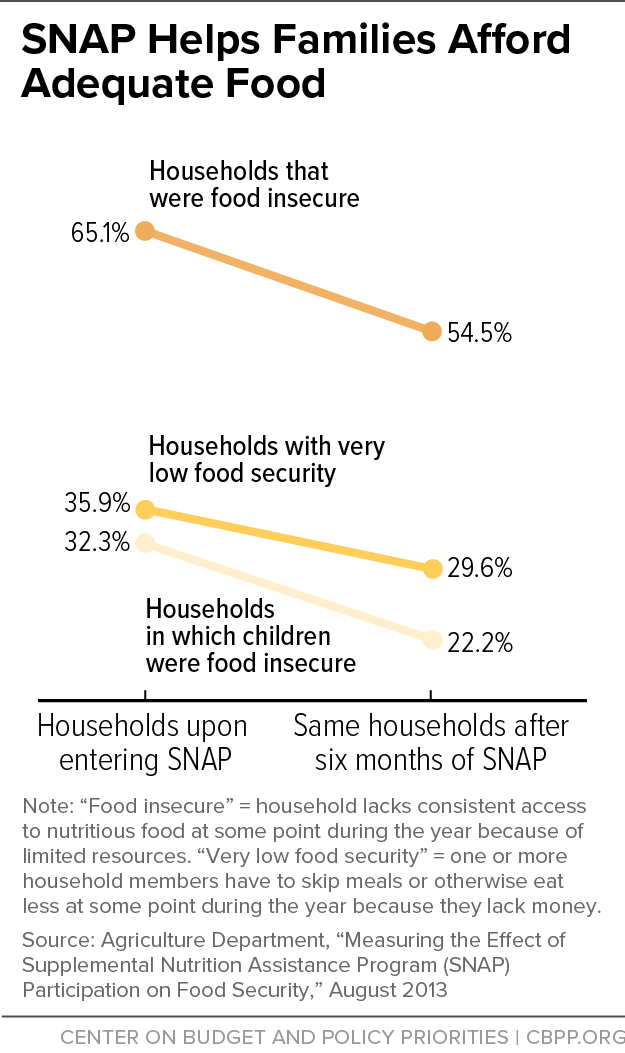
[35] James Mabli et al., “Measuring the Effect of Supplemental Nutrition Assistance Program (SNAP) Participation on Food Security,” Food and Nutrition Service, USDA, 2013, https://www.fns.usda.gov/measuring-effect-snap-participation-food-security-0. By following families as they enter SNAP, this study avoids two major pitfalls that would otherwise make it difficult to assert that participation is responsible for the improvements in food security. First, it avoids the problems associated with self-selection by using these families as their own controls, comparing their food security status just before entering SNAP to their status six months later (rather than to non-participants). Second, it avoids the problems associated with underreporting of SNAP participation in most surveys by drawing the sample of families directly from the records of local SNAP offices. A subsequent publication by the same research team offers slightly revised but substantively similar estimates of the overall impact of SNAP on food security and very low food insecurity. See James Mabli and Jim Ohls, “Supplemental Nutrition Assistance Program Participation Is Associated with an Increase in Household Food Security in a National Evaluation,” Journal of Nutrition, 145(2): 344-351, 2015, https://academic.oup.com/jn/article/145/2/344/4585732.
[36] Caroline Ratcliffe, Signe-Mary McKernan, and Sisi Zhang, “How Much Does the Supplemental Nutrition Assistance Program Reduce Food Insecurity?” American Journal of Agricultural Economics, 93(4): 1082-1098, July 12, 2011, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4154696/.
[37] Seungyeon Cho, “The Effect of Participation in the Supplemental Nutrition Assistance Program on Food Insecurity of Children in US Immigrant Households,” Journal of Family and Economic Issues, September 20, 2021, https://link.springer.com/article/10.1007/s10834-021-09799-9#citeas.
[38] Partha Deb and Christian Gregory, “Heterogeneous Impacts of the Supplemental Nutrition Assistance Program on Food Insecurity,” Economics Letters, 173: 55-60, 2018, https://www.sciencedirect.com/science/article/abs/pii/S0165176518303896.
[39] The demonstration initially provided a monthly benefit of $60 in the summer of 2012 and then compared the relative effectiveness of a smaller benefit ($30) in the summers of 2013 and 2014. The results suggested that both increases produced similar improvements in the most severe form of food insecurity among children. See Ann Collins et al., “Summer Electronic Benefits Transfer for Children (SEBTC) Demonstration: Summary Report,” prepared for the Food and Nutrition Service, USDA, May 2016, https://fns-prod.azureedge.net/sites/default/files/ops/sebtcfinalreport.pdf.
[40] Mark Nord and Mark Prell, “Food Security Improved Following the 2009 ARRA Increase in SNAP Benefits,” ERR-116, Economic Research Service, USDA, April 2011, https://www.ers.usda.gov/webdocs/publications/44837/7469_err116.pdf?v=41056.
[41] For example, see Andrew Bryant and Lendie Follett, “Hunger Relief: A Natural Experiment from Additional SNAP Benefits During the COVID-19 Pandemic,” The Lancet Regional Health - Americas, 10, June 2022, https://www.sciencedirect.com/science/article/pii/S2667193X22000412.
[42] Lauren Bauer et al., “An Update on the Effect of Pandemic EBT on Measures of Food Hardship,” Brookings Institution Hamilton Project, September 29, 2021, https://www.brookings.edu/research/an-update-on-the-effect-of-pandemic-ebt-on-measures-of-food-hardship/. Food insufficiency is a more severe condition than food insecurity and measures whether a household generally has enough to eat. In this way, food insufficiency is closer in severity to very low food security than to overall food insecurity.
[43] Bryant and Follett, op. cit.
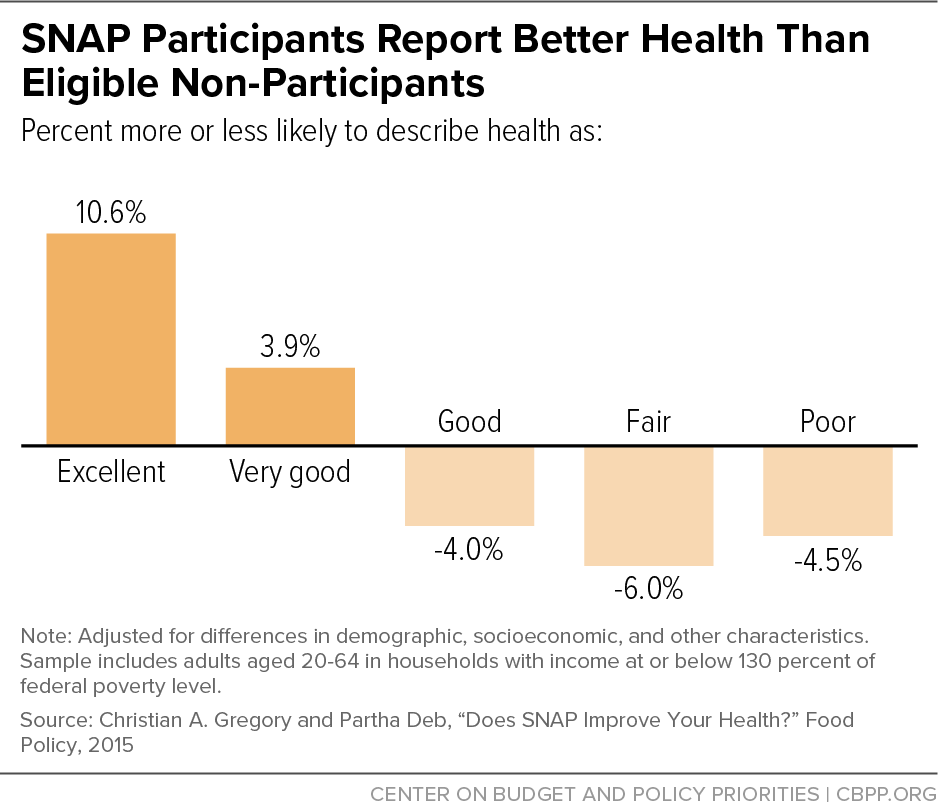
[44] Christian A. Gregory and Partha Deb, “Does SNAP Improve Your Health?” Food Policy, 50: 11-19, 2015, http://www.sciencedirect.com/science/article/pii/S0306919214001419; Daniel Miller and Taryn Morrissey, “SNAP Participation and the Health and Health Care Utilization of Low-Income Adults and Children,” Public Health Nutrition, 24(18): 6543-6554, 2021, https://www.cambridge.org/core/journals/public-health-nutrition/article/snap-participation-and-the-health-and-health-care-utilization-of-lowincome-adults-and-children/F0889E87B0104D151582D0C574EE0577; Vanessa Oddo and James Mabli, “Participation in the Supplemental Nutrition Assistance Program and Psychological Distress,” American Journal of Public Health, 6: e30-e35, June 2015, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4431109/pdf/AJPH.2014.302480.pdf; and Harry Adynski, Todd Schwartz, and Hudson Santos, “Does Participation in Food Benefit Programs Reduce the Risk for Depressive Symptoms?” Journal of the American Psychiatric Nurses Association, January 3, 2021, https://journals.sagepub.com/doi/full/10.1177/1078390320983904.
[45] Katherine M. Joyce et al., “Household Hardships, Public Programs, and Their Associations with the Health and Development of Very Young Children: Insights from Children’s HealthWatch,” Journal of Applied Research on Children: Informing Policy for Children at Risk, 3(1), 2012, http://www.childrenshealthwatch.org/wp-content/uploads/KJ_JARC_2012.pdf; Stephanie Ettinger de Cuba et al., “The SNAP Vaccine: Boosting Children’s Health,” Children’s HealthWatch, February 1, 2012, http://childrenshealthwatch.org/the-snap-vaccine-boosting-childrens-health/; and Stephanie Ettinger de Cuba et al., “SNAP, Young Children’s Health, and Family Food Security and Healthcare Access,” American Journal of Preventive Medicine, 57(4): 525-532, 2019, https://www.researchgate.net/profile/Mariana-Chilton/publication/335916252_SNAP_Young_Children's_Health_and_Family_Food_Security_and_Healthcare_Access/links/5d8371da299bf1996f77762d/SNAP-Young-Childrens-Health-and-Family-Food-Security-and-Healthcare-Access.pdf.
[46] Allison Bovell et al., “Making SNAP Work for Families Leaving Poverty,” Children’s HealthWatch, November 2014, http://www.childrenshealthwatch.org/wp-content/uploads/FINALPhilly-Food-to-web3.pdf; and Stephanie Ettinger de Cuba et al., “Punishing Hard Work: The Unintended Consequences of Cutting SNAP Benefits,” Children’s HealthWatch, December 12, 2013, http://childrenshealthwatch.org/punishing-hard-work-the-unintended-consequences-of-cutting-snap-benefits/.
[47] Katelin Alfaro-Hudak et al., “SNAP and Cardiometabolic Risk in Youth,” Nutrients, 14(13): 2756, 2022, https://www.mdpi.com/2072-6643/14/13/2756.
[48] Tae-Young Pak and GwanSeon Kim, “Food Stamps, Food Insecurity, And Health Outcomes Among Elderly Americans,” Preventive Medicine, 130: 105871, 2020, https://www.sciencedirect.com/science/article/abs/pii/S0091743519303470.
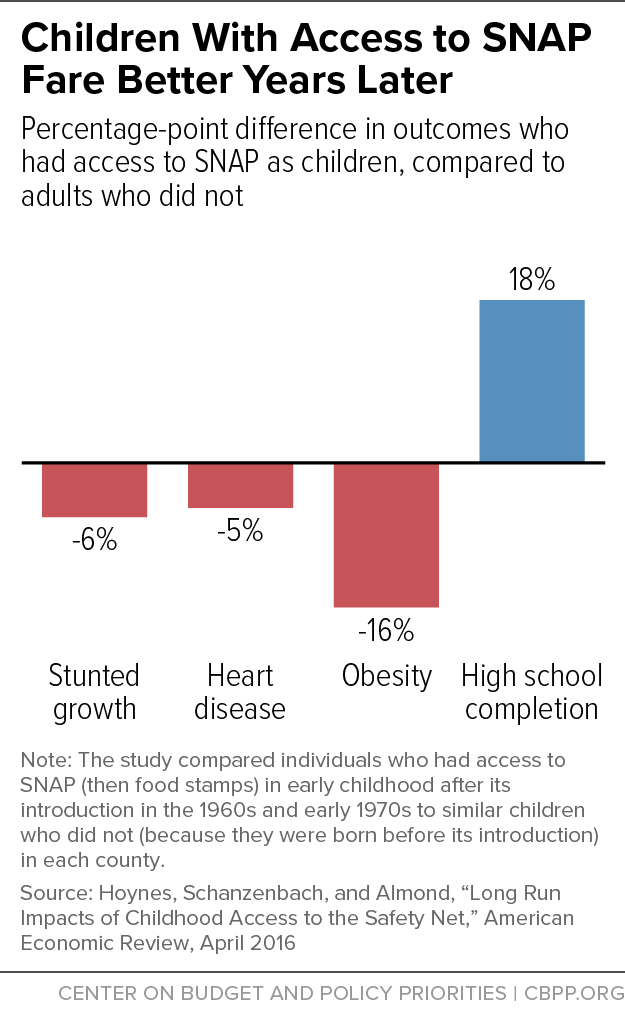
[49] Douglas Almond, Hillary Hoynes, and Diane Schanzenbach, “Inside the War on Poverty: The Impact of Food Stamps on Birth Outcomes,” Review of Economics and Statistics, 93(2), May 2011, https://www.mitpressjournals.org/doi/pdfplus/10.1162/REST_a_00089; Hilary Hoynes and Diane Whitmore Schanzenbach, and Douglas Almond, “Long-Run Impacts of Childhood Access to the Safety Net,” American Economic Review, 106(4): 903-934, April 2016, https://pdfs.semanticscholar.org/c94b/26c57bb565b566913d2af161e555edeb7f21.pdf. (It is important to note that much has changed since the initial introduction of the Food Stamp Program, including the introduction and growth of the Special Supplemental Nutrition Program for Women, Infants, and Children, and Medicaid.) An unpublished paper using a similar research approach found mixed results that indicate small or non-existent overall effects of access to food stamps on mortality rates. See Jordan Jones, Charles Courtemanche, and James Marton, “The Impacts of the Food Stamp Program on Mortality,” prepared for presentation at the 2018 Agricultural & Applied Economics Association Annual Meeting, August 2018, https://ageconsearch.umn.edu/record/273845?ln=en..
[50] Angela Fertig, “The Long-Term Health Consequences of Childhood Food Insecurity,” University of Kentucky Center for Poverty Research Discussion Paper 2019-03, May 2019, https://ukcpr.org/sites/ukcpr/files/research-pdfs/DP2019-03.pdf.
[51] Chloe East, “The Effect of Food Stamps on Children’s Health: Evidence from Immigrants’ Changing Eligibility,” Journal of Human Resources, 55(2): 387-427, 2020, http://jhr.uwpress.org/content/55/2/387.
[52] Irma Arteaga, Leslie Hodges, and Colleen Heflin, “Giving Kids a Boost: The Positive Relationship Between Frequency of SNAP Participation and Infant's Preventative Health Care Utilization," SSM-Population Health, 15: 100910, 2021, https://www.sciencedirect.com/science/article/pii/S2352827321001853#bib45.
[53] Hilary Hoynes, Erin Bronchetti, and Garret Christensen, “The Real Value of SNAP Benefits and Health Outcomes,” University of Kentucky Center for Poverty Research, Discussion Paper Series, DP2017-03, January 2017, https://uknowledge.uky.edu/cgi/viewcontent.cgi?referer=&httpsredir=1&article=1104&context=ukcpr_papers; and Erin Bronchetti, Garret Christensen, and Hilary Hoynes, “Local Food Prices, SNAP Purchasing Power, and Child Health,” Journal of Health Economics, 68: 102231, 2019, https://www.sciencedirect.com/science/article/abs/pii/S0167629619304151.
[54] Conversely, some low-income people may spend less on basic needs (such as food, clothing, housing, and transportation) to afford their medications. Research focusing on such individuals who choose medication over basic needs is limited. A study of a small number of low-income adults in St. Louis, Missouri, found that those eligible for or receiving SNAP were somewhat less likely to spend less on basic needs to pay for medication though the difference was not statistically significant. See Karthik Rohatgi et al., “Medication Adherence and Characteristics of Patients Who Spend Less on Basic Needs to Afford Medications,” Journal of the American Board of Family Medicine, 34(3): 561-570, 2021, https://www.jabfm.org/content/jabfp/34/3/561.full.pdf.
[55] Among older SNAP participants in Missouri, for example, about 69 percent were diagnosed with hypertension and 40 percent were diagnosed with diabetes. See Colleen Heflin et al., “Hypertension, Diabetes and Medication Adherence among the Older Supplemental Nutritional Assistance Program Population,” Journal of Applied Gerontology, June 17, 2021, https://journals.sagepub.com/doi/abs/10.1177/07334648211022493.
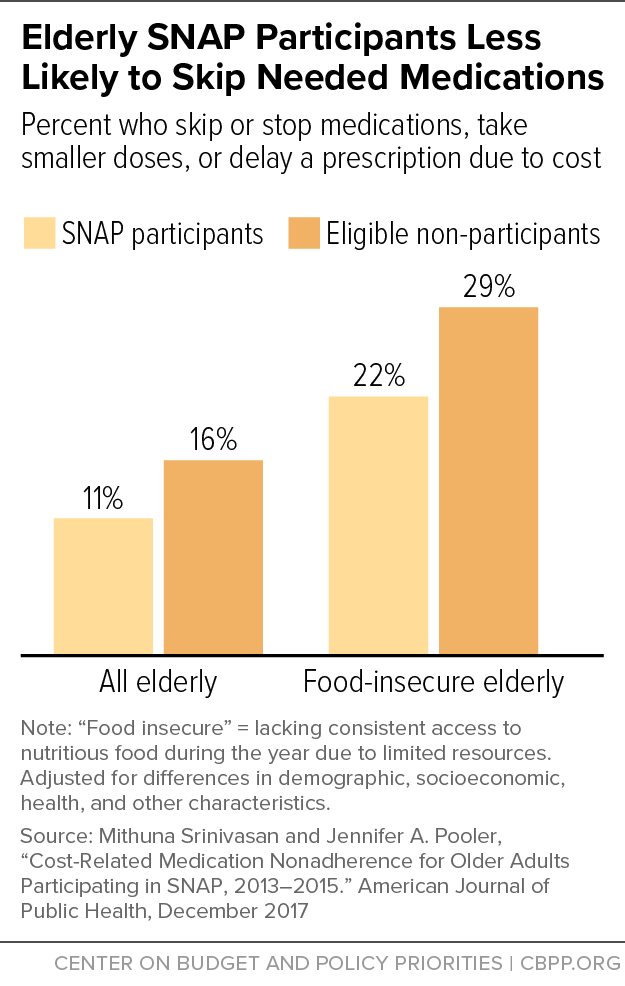
[56] Mithuna Srinivasan and Jennifer A. Pooler, “Cost-Related Medication Nonadherence for Older Adults Participating in SNAP, 2013–2015,” American Journal of Public Health, 108(2): 224-230, 2018, http://ajph.aphapublications.org/doi/10.2105/AJPH.2017.304176; Jennifer Pooler and Mithuna Srinivasan, “Association Between Supplemental Nutrition Assistance Program Participation and Cost-Related Medication Nonadherence Among Older Adults with Diabetes,” JAMA Internal Medicine, 179(1): 63-70, 2019, https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2715159.
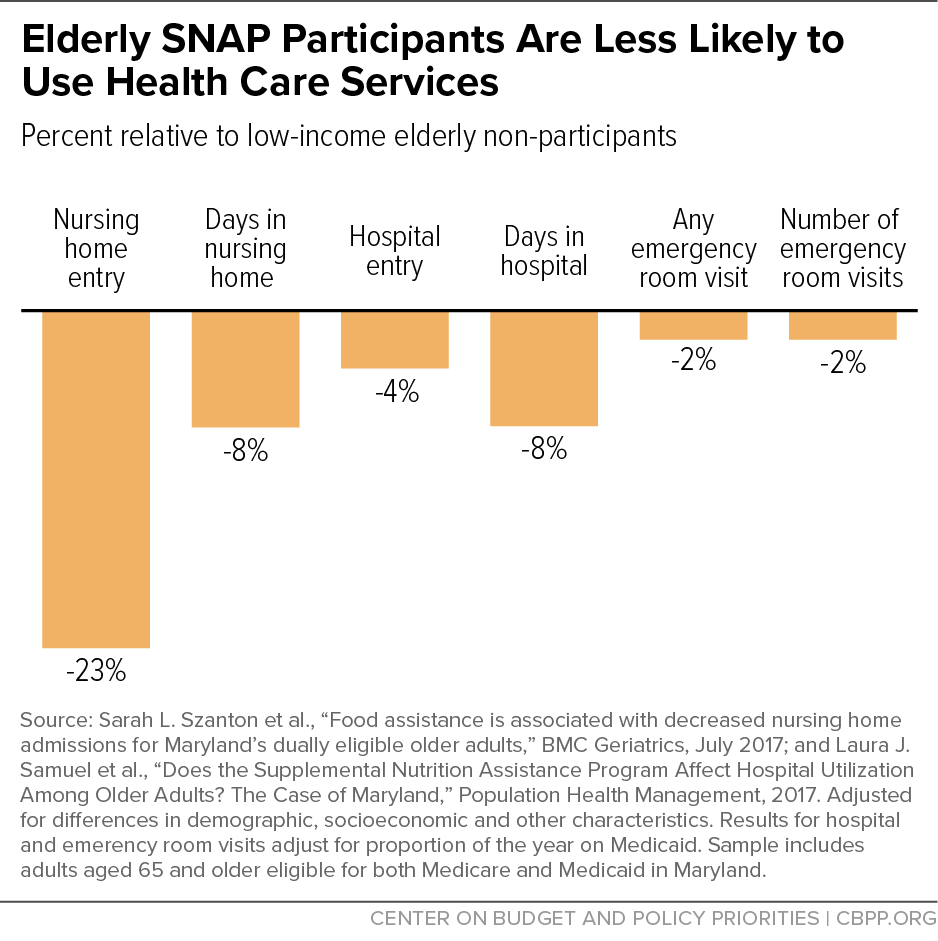
[57] See Sarah L. Szanton et al., “Food assistance is associated with decreased nursing home admissions for Maryland’s Dually Eligible Older Adults,” BMC Geriatrics, 17(1), 162, 2017, https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-017-0553-x; and Laura J. Samuel et al., “Does the Supplemental Nutrition Assistance Program Affect Hospital Utilization Among Older Adults? The Case of Maryland,” Population Health Management, 21(2): 88-95, 2018, https://www.liebertpub.com/doi/full/10.1089/pop.2017.0055. In addition to controlling for demographic and socioeconomic factors that may contribute to differences between SNAP participants and non-participants, hospitalization findings include a control for proportion of time spent on Medicaid. As the authors note, SNAP participants are more likely to participate in Medicaid, and Medicaid participation is linked with hospital utilization. Models that do not include this control (but do control for demographic and socioeconomic factors) find that SNAP participants had a 14 percent lower probability of hospitalization compared to non-participants.
[58] Seth Berkowitz et al., “Supplemental Nutrition Assistance Program Participation and Health Care Use in Older Adults: A Cohort Study,” Annals of Internal Medicine, 174(12): 1674-1682, 2021, https://www.acpjournals.org/doi/abs/10.7326/M21-1588.
[59] Chinedum Ojinnaka and Colleen Heflin, “Supplemental Nutrition Assistance Program Size and Timing and Hypertension-Related Emergency Department Claims Among Medicaid Enrollees,” Journal of the American Society of Hypertension, 12(11): e27-e34, 2018, https://www.sciencedirect.com/science/article/abs/pii/S1933171118302869.
[60] Chloe East and Andrew Friedson, “An Apple A Day? Adult Food Stamp Eligibility and Health-Care Utilization among Immigrants,” American Journal of Health Economics, 6(3): 289-323, 2020, https://research.upjohn.org/cgi/viewcontent.cgi?article=1313&context=up_workingpapers. As noted above, the changes in immigrant eligibility due to the 1996 law that changed basic needs programs and subsequent legislation allow for a relatively strong test of the impact of SNAP on health care utilization and outcomes.
[61] J. Kim, “Are Older Adults Who Participate in the Supplemental Nutrition Assistance Program Healthier Than Eligible Nonparticipants? Evidence from the Health and Retirement Study,” Gerontologist, 55 (Supplement Issue 2): 672, November 1, 2015, https://academic.oup.com/gerontologist/article/55/Suppl_2/672/2489236.
[62] A study focused on children found that those who participated consistently in SNAP over the course of two years had lower unadjusted health care expenditures compared to children who did not participate, but these differences were not significant after controlling for characteristics of the child, parent, and household. It is possible that longer time horizons, likely well beyond 24 months, are needed to detect the effects that programs which moderate food insecurity among children have on health care expenditures. See Stephen Rogers et al., "Supplemental Nutrition Assistance Program Participation and Health Care Expenditures in Children," BMC Pediatrics, 22(155), 2022, https://link.springer.com/article/10.1186/s12887-022-03188-3.
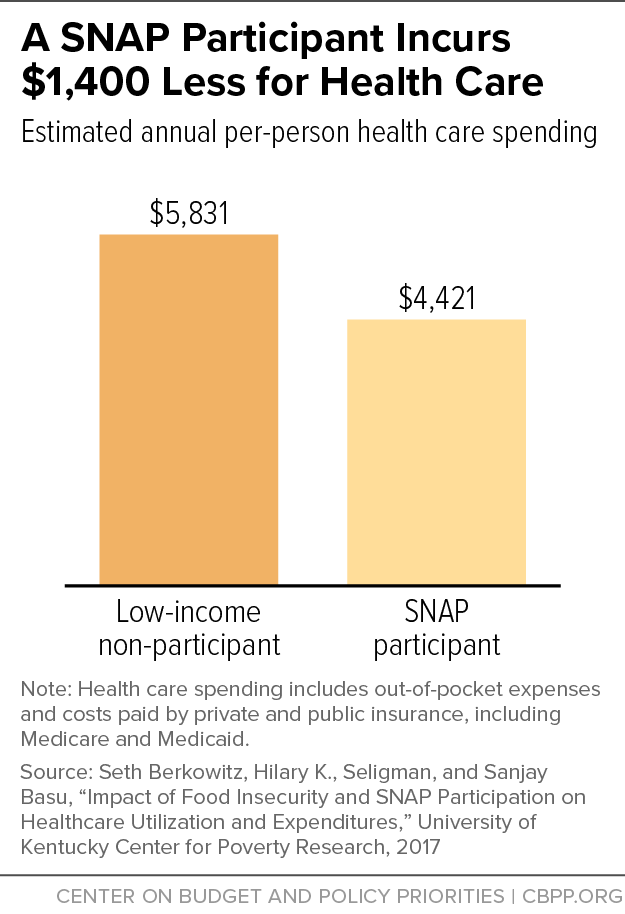
[63] Seth A. Berkowitz et al., “Supplemental Nutrition Assistance Program (SNAP) Participation and Health Care Expenditures Among Low-Income Adults,” JAMA Internal Medicine, November 2017, https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2653910?amp%3butm_source=JAMA+Intern+MedPublishAheadofPrint&utm_campaign=25-09-2017; and Seth Berkowitz, Hilary K. Seligman, and Sanjay Basu, “Impact of Food Insecurity and SNAP Participation on Healthcare Utilization and Expenditures,” University of Kentucky Center for Poverty Research Discussion Paper Series, DP2017-02, 2017, http://uknowledge.uky.edu/cgi/viewcontent.cgi?article=1105&context=ukcpr_papers. An older study that did not fully account for unobserved differences did not find a significant difference in Medicare spending among low-income elderly with diabetes between those who received food stamps (as SNAP was known then) and those who did not.
[64] See Lauren H. Nicholas, “Can Food Stamps Help to Reduce Medicare Spending on Diabetes?” Economics and Human Biology, 9(1): 1-13, January 2011, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3032985/. Still older work using a different data set and analytic approach concluded that SNAP increased medical expenses of non-elderly women by $300 to $700 per year, mainly because program benefits freed up additional discretionary income that could be spent on medical care. See Chad D. Meyerhoefer and Yuriy Pylypchuk, “Does Participation in the Food Stamp Program Increase the Prevalence of Obesity and Health Care Spending?” American Journal of Agricultural Economics, 90(2): 287-305, May 1, 2008, https://onlinelibrary.wiley.com/doi/10.1111/j.1467-8276.2007.01125.x.
[65] Some enrollment groups, such as adults who gained eligibility through Affordable Care Act Medicaid expansions, receive federal match rates outside of this range.
[66] While states are responsible for half of the administrative cost of eligibility determinations, employment and training, nutrition education, and anti-fraud activities, these costs represent a small part of SNAP’s overall costs. In fiscal year 2021, the federal government spent about $114 billion on SNAP, including emergency relief funding in response to the COVID-19 pandemic. Ninety-five percent went directly to benefits that households used to purchase food, and less than 4 percent went to state administrative costs.
[67] Joseph Llobrera, Matt Saenz, and Lauren Hall, “USDA Announces Important SNAP Benefit Modernization,” Center on Budget and Policy Priorities, August 26, 2021, https://www.cbpp.org/research/food-assistance/usda-announces-important-snap-benefit-modernization.
[68] Mark Nord and Mark Prell, “Food Security Improved Following the 2009 ARRA Increase in SNAP Benefits,” Economic Research Service, USDA, April 2011, https://www.ers.usda.gov/publications/pub-details/?pubid=44839; Jiyoon Kim, “Do SNAP Participants Expand Non-Food Spending When They Receive More SNAP Benefits? — Evidence from the 2009 SNAP Benefits Increase,” Food Policy, 65: 9-20. 2016, https://www.sciencedirect.com/science/article/abs/pii/S0306919216304341.
[69] Taryn Morrissey and Daniel Miller, “Supplemental Nutrition Assistance Program Participation Improves Children’s Health Care Use: An Analysis of the American Recovery and Reinvestment Act's Natural Experiment,” Academic Pediatrics, 20(6): 863-870, 2020, https://www.sciencedirect.com/science/article/abs/pii/S1876285919304619.
[70] Katelin Hudak, Elizabeth Racine, and Lisa Schulkind, “An Increase in SNAP Benefits Did Not Impact Food Security or Diet Quality in Youth,” Journal of the Academy of Nutrition and Dietetics. 121(3): 507-519, 2020, https://www.sciencedirect.com/science/article/abs/pii/S2212267220313198.
[71] Laura Samuel et al., “Supplemental Nutrition Assistance Program 2009 Expansion and Cardiometabolic Markers among Low-Income Adults,” Preventive Medicine, 150: 106678, 2021, https://www.sciencedirect.com/science/article/abs/pii/S0091743521002474.
[72] Rajan Sonik, “Massachusetts Inpatient Medicaid Cost Response to Increased Supplemental Nutrition Assistance Program Benefits,” American Journal of Public Health, 106(3): 443-44, 2016, https://ajph.aphapublications.org/doi/full/10.2105/AJPH.2015.302990; and Rajan Sonik, Susan Parish, and Monika Mitra, “Inpatient Medicaid Usage and Expenditure Patterns After Changes in Supplemental Nutrition Assistance Program Benefit Levels,” Preventing Chronic Disease, 15: E120, 2018, https://stacks.cdc.gov/view/cdc/60010.
[73] See Stacy Gleason, Dani Hansen, and Breanna Wakar, “Indicators of diet quality, nutrition, and health for Americans by program participation status: SNAP Report,” Food and Nutrition Service, USDA, December 2021, https://www.fns.usda.gov/snap/indicators-diet-quality-nutrition-and-health-americans-program-participation-status-2011; Chelsea Singleton et al., “Examining disparities in diet quality between SNAP participants and non-participants using Oaxaca-Blinder decomposition analysis,” Preventive Medicine Reports, 19: 101134, 2020, https://www.sciencedirect.com/science/article/pii/S2211335520300942; Yu Chen et al., “Nutritional quality of retail food purchases is not associated with participation in the Supplemental Nutrition Assistance Program for nutrition-oriented households,” Plos One, 15(12): e0240263, 2020, https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0240263; and Fang Zhang et al., “Trends and disparities in diet quality among US adults by Supplemental Nutrition Assistance Program Participation status,” JAMA Network Open, 1(2): e180237, 2018, https://jamanetwork.com/journals/jamanetworkopen/article-abstract/2684625.
[74] See Steven Garasky et al., “Foods typically purchased by Supplemental Nutrition Assistance Program (SNAP) households,” Food and Nutrition Service, USDA, November 2016, https://www.fns.usda.gov/snap/foods-typically-purchased-supplemental-nutrition-assistance-program-snap-household; Anna Grummon and Lindsey Smith Taillie, “Nutritional profile of Supplemental Nutrition Assistance Program household food and beverage purchases,” American Journal of Clinical Nutrition, 105(6): 1433-1442, 2017, https://academic.oup.com/ajcn/article/105/6/1433/4633995; Gleason, Hansen, and Wakar, op. cit; and Marilyn Tseng et al., “Fruit and Vegetable Purchasing Patterns and Supplemental Nutrition Assistance Program Participation: Findings From a Nationally Representative Survey,” Journal of the Academy of Nutrition and Dietetics, 120(10): 1633-1642, 2020, https://www.sciencedirect.com/science/article/pii/S2212267220305165.
[75] See Mary Kay Fox, William Hamilton, and Biing-Hwan Lin (eds.), “Effects of Food Assistance and Nutrition Programs on Nutrition and Health: Volume 3, Literature Review,” Economic Research Service, USDA, 2004, https://www.ers.usda.gov/webdocs/publications/46556/30240_fanrr19-3_002.pdf?v=0 ; IOM (Institute of Medicine) and NRC (National Research Council), “Supplemental Nutrition Assistance Program: Examining the Evidence to Define Benefit Adequacy, 2013, https://pubmed.ncbi.nlm.nih.gov/23858096/; Tatiana Andreyeva, Amanda Tripp, and Marlene Schwartz, “Dietary Quality of Americans by Supplemental Nutrition Assistance Program Participation Status: A Systematic Review,” American Journal of Preventive Medicine, 49(4): 594-604, 2015, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6022372/; and Prageet Sachdev, Mahsa Babaei, and Jeanne Freeland-Graves, “Supplemental Nutrition Assistance Program (SNAP): does receiving assistance impact food choices?” Nutrition and Dietary Supplements, 11: 19-35, 2019, https://www.proquest.com/openview/34b4a3e3e255d405728b6e51449c7107/1?pq-origsite=gscholar&cbl=3933339.
[76] Geetha Waehrer, Partha Deb, and Sandra L. Decker, “Did the 2009 American Recovery and Reinvestment Act affect dietary intake of low-income individuals?” Economics & Human Biology, 19: 170-183, 2015, https://www.sciencedirect.com/science/article/pii/S1570677X1500060X; and Hudak, Racine, and Schulkind, op. cit.
[77] Michele Ver Ploeg and Chen Zhen, “Changes in SNAP Benefit Levels and Food Spending and Diet Quality: Simulations from the National Household Food Acquisition and Purchase Survey,” Center on Budget and Policy Priorities, May 12, 2022, https://www.cbpp.org/research/food-assistance/changes-in-snap-benefit-levels-and-food-spending-and-diet-quality.
[78] Marianne P. Bitler, “The Health and Nutrition Effects of SNAP: Selection into the Program and a Review of the Literature on Its Effects,” in SNAP Matters: How Food Stamps Affect Health and Well-Being, 2016, http://www.ukcpr.org/sites/www.ukcpr.org/files/documents/DP2014-02_0.pdf; Gregory and Deb (2015); and Zach Conrad, Colin D. Rehm, Parke Wilde, and Dariush Mozaffarian, “Cardiometabolic Mortality by Supplemental Nutrition Assistance Program Participation and Eligibility in the United States,” American Journal of Public Health, 107(3): 466-474, March 2017, https://www.ncbi.nlm.nih.gov/pubmed/28103061.
[79] Charles Courtemanche, Augustine Denteh, and Rusty Tchernis, “Estimating the Associations Between SNAP and Food Insecurity, Obesity, and Food Purchases with Imperfect Administrative Measures of Participation,” Southern Economic Journal, 86(1): 202-228, 2019, https://www.nber.org/system/files/working_papers/w24412/w24412.pdf. Although this paper assesses the associations between SNAP participation and food security, obesity, and diet quality, it does so without accounting for self-selection into the program as this was outside the scope of the project. The results are best interpreted as indications of negative selection, that those with greatest need (that is, more food insecure and less healthy) are more likely to participate than others.
[80] An exception in the literature is Brent Kreider et al., “Identifying the Effects of SNAP (Food Stamps) on Child Health Outcomes When Participation Is Endogenous and Misreported,” Journal of the American Statistical Association, 107(499): 958-975, September 2012, http://batten.virginia.edu/sites/default/files/research/attachments/JASA_KPGJ_online(1).pdf. Using relatively strong but plausible assumptions to address self-selection and classification errors simultaneously, the authors estimate that SNAP reduces the prevalence of child food insecurity by at least 8 percentage points.