BEYOND THE NUMBERS
Update, June 26: We’ve revised these posts to reflect the text of the Senate bill released June 22.
The Senate Republican health bill lowers the annual increase in state Medicaid funding under a per capita cap below the House bill’s already inadequate rate starting in 2025. That means states would have to absorb even deeper cuts in federal Medicaid funding than under the House bill — which would cut federal Medicaid spending by $834 billion over ten years and slash enrollment by 14 million by 2026, relative to current law, the Congressional Budget Office (CBO) estimates.
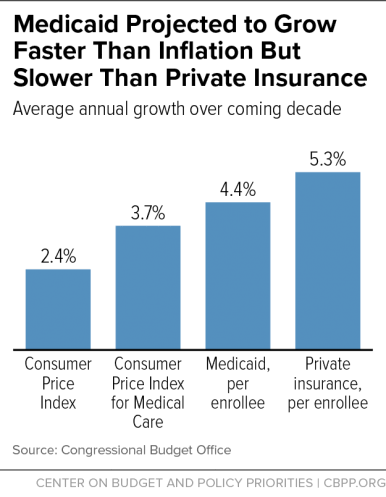
The House bill’s per capita cap is expected to grow more slowly than Medicaid costs per beneficiary, according to CBO, cutting federal Medicaid funding and shifting costs to states, which would be responsible for all Medicaid costs that exceed the cap. Specifically, CBO expects Medicaid per beneficiary costs to rise by 4.4 percent a year over the next decade, on average. But the per capita cap would take a state’s Medicaid spending per beneficiary in fiscal year 2016 and increase it annually through 2019 only by the medical care component of the Consumer Price Index (M-CPI), which CBO expects to grow by 3.7 percent per year. Starting in 2020, when the cap takes effect, it would grow by a mix of M-CPI or M-CPI plus 1 percentage point (depending on the beneficiary population group).
The Senate bill would lower the growth rate to general inflation (CPI-U) for all beneficiary groups starting around 2025. This would produce even larger cuts, as CBO projects general inflation to grow by only 2.4 percent a year. (See graph.) We expect this smaller growth rate to raise the federal Medicaid funding cut for states under the per capita cap by hundreds of billions of dollars, compared to the House bill, over the subsequent decade (2027 to 2036). This greater cost shift would force states to make even deeper and more damaging cuts to Medicaid eligibility, benefits, and provider payments than under the House bill.
Moreover, the lower growth rate would take effect just as the population’s aging is raising Medicaid costs, as the Urban Institute, Kaiser Family Foundation, and AARP note. The share of seniors who are 85 and older will rise substantially in future decades as the huge baby-boom population moves into “old-old” age. Seniors aged 85 and older have much higher health care costs than younger elderly people because they have more serious and chronic health problems and are likelier to require nursing home and other long-term services and supports. In 2011, average Medicaid costs were more than 2.5 times higher for beneficiaries 85 and older than for those aged 65 to 74. All 32 states with available projections estimate that the share of their seniors who are 85 and older will rise between 2025 and 2035, and well more than half of them project an increase of at least 25 percent. Alaska projects a 76 percent increase.
Further, cutting the growth rate in federal Medicaid funding would also leave states even less able to address higher-than-expected costs stemming from public health emergencies like another opioid crisis (which has driven up Medicaid costs among the states most deeply affected), a new epidemic, or costly breakthrough drugs and treatments.