BEYOND THE NUMBERS
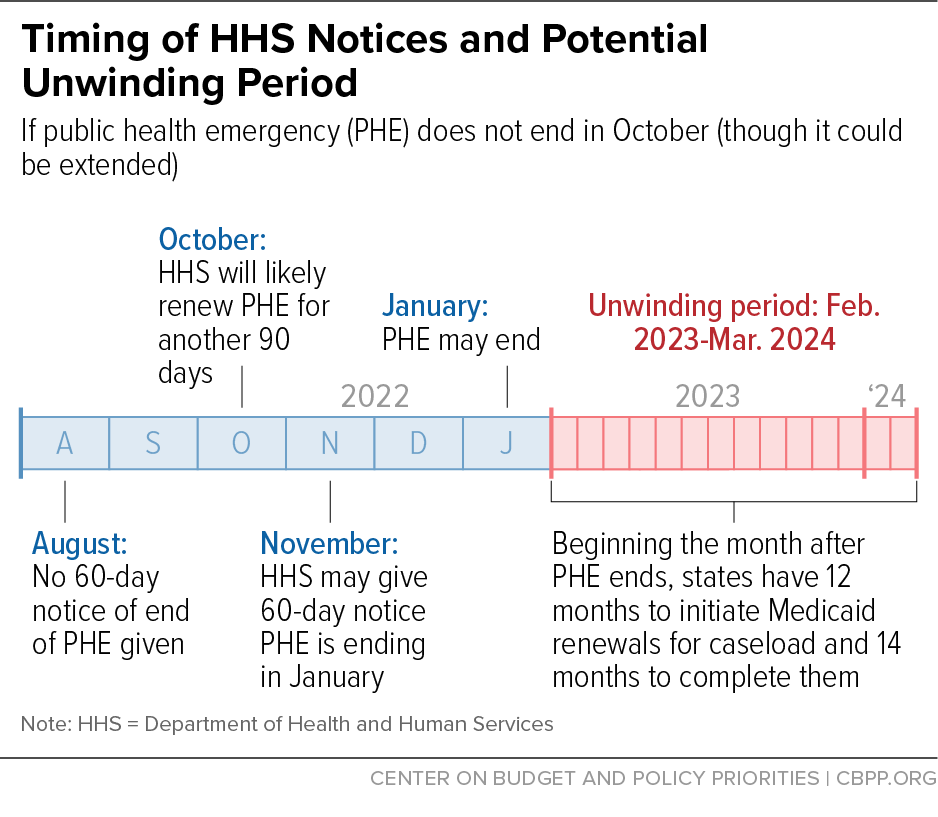
The Department of Health and Human Services (HHS) has promised states that it will give 60 days’ notice before ending the COVID-19 public health emergency (PHE). With less than 60 days before the end of the current PHE — which lasts through mid-October — and no notice from HHS, it is expected that the PHE will be renewed again. State Medicaid agencies now likely have until at least mid-January to prepare for the end of the PHE and can take steps now to ensure that eligible people stay covered when the PHE expires.
The “continuous coverage” requirement, part of the 2020 Families First Coronavirus Response Act, prohibits states from ending coverage for most enrollees during the PHE in exchange for enhanced Medicaid funding. When the PHE ends, state and local agencies will have to begin reviewing the eligibility of everyone enrolled in Medicaid, often referred to as “unwinding.”
With over 80 million Medicaid enrollees, unwinding the continuous coverage requirement will be a huge undertaking for state Medicaid agencies. Within 14 months of the end of the PHE, they will have to review the eligibility of every Medicaid enrollee. That work will include connecting with enrollees who haven’t been in contact with the agency in over two years, may have moved, and may not understand the renewal process. Medicaid agencies will have to make significant updates to their eligibility systems, train eligibility workers, and deal with many inquiries from enrollees confused about renewal notices or why they lost coverage, all while facing unprecedented staffing shortages.
Recognizing the importance of predictability and the substantial undertaking required by Medicaid agencies, HHS pledged last year to provide 60 days’ advance notice before ending the PHE. States are relying on this promise for sufficient time to plan and implement changes like technology system updates, collaborative outreach with local organizations to enrollees about the upcoming renewals, and initiation of their renewal processes. In fact, many groups requested that HHS provide more than 60 days’ notice to ensure states are fully prepared for the task ahead and to minimize coverage losses. HHS’ promise remains at 60 days but will nonetheless be critical in giving states time to plan. (See graphic.)
During the unwinding period, there is a substantial risk that eligible Medicaid enrollees could lose coverage for procedural reasons such as not receiving notice to renew or not returning requested paperwork on time. Other enrollees could become uninsured if they are no longer eligible for Medicaid and fall into the coverage gap because their state hasn’t adopted the Affordable Care Act’s (ACA) Medicaid expansion or if they don’t successfully transition to marketplace coverage.
But massive coverage losses aren’t inevitable. With the PHE likely to be extended at least through mid-January, states have valuable time to plan ahead to improve the renewal process during the unwinding and beyond. With guidance from the Centers for Medicare & Medicaid Services, states should focus their efforts on:
- Conducting proactive outreach and communicating with enrollees about actions they need to take now and when the PHE ends,
- Strengthening their renewal processes to prevent procedural coverage losses, and
- Ensuring they can effectively transition enrollees who are no longer eligible for Medicaid to other types of low-cost coverage such as through the ACA marketplace.
Medicaid agencies likely have at least five more months to prepare for unwinding. Agencies should use this time to prepare and make necessary changes to their systems so eligible people don’t lose their coverage when the PHE ends.