BEYOND THE NUMBERS
Since the start of the Affordable Care Act’s (ACA) Medicaid expansion to low-income adults, evidence has poured in that the expansion is helping enrollees access and afford care. But as more time passes, researchers can also examine how expansion is affecting other health and financial outcomes. New research finds the policy is delivering on its promise to improve both financial security and health – including by saving lives.
Medicaid expansion saved the lives of at least 19,200 older low-income adults from 2014 to 2017 in states that adopted it, while state decisions not to expand cost the lives of 15,600. (Hover on the map below for state-by-state estimates.) Expansion was most consequential in preventing premature deaths from causes such as cardiovascular disease and diabetes, which are conditions responsive to medical care.
| TABLE 1 | |
|---|---|
| Lives Saved, and Lost, Due to States’ Medicaid Expansion Decisions, Adults Aged 55-64 | |
| State | Lives at stake, 2014 to 2017 |
| Alabama | 768 |
| Alaska* | 76 |
| Arizona | 808 |
| Arkansas | 440 |
| California | 4,448 |
| Colorado | 520 |
| Connecticut | 304 |
| Florida | 2,776 |
| Georgia | 1,336 |
| Hawaii | 156 |
| Idaho** | 180 |
| Illinois | 1,380 |
| Indiana* | 796 |
| Iowa | 272 |
| Kansas | 288 |
| Kentucky | 704 |
| Louisiana* | 764 |
| Maine* | 180 |
| Maryland | 528 |
| Michigan* | 1,196 |
| Minnesota | 460 |
| Mississippi | 540 |
| Missouri | 776 |
| Montana* | 132 |
| Nebraska** | 152 |
| Nevada | 356 |
| New Hampshire* | 120 |
| New Jersey | 828 |
| New Mexico | 284 |
| North Carolina | 1,400 |
| North Dakota | 44 |
| Ohio | 1,452 |
| Oklahoma | 476 |
| Oregon | 484 |
| Pennsylvania* | 1,476 |
| Rhode Island | 120 |
| South Carolina | 788 |
| South Dakota | 84 |
| Tennessee | 964 |
| Texas | 2,920 |
| Utah** | 216 |
| Virginia* | 900 |
| Washington | 688 |
| West Virginia | 348 |
| Wisconsin | 576 |
| Wyoming | 64 |
Figures colored orange represent lives lost in states that have not adopted Medicaid expansion for low-income adults under the Affordable Care Act. Blue represents lives saved in expansion states. Table omits the District of Columbia, Massachusetts, New York, and Vermont, because they expanded Medicaid prior to 2014 and are therefore excluded from the analysis.
* Some states expanded Medicaid to low-income adults effective after January 1, 2014: Michigan (April 2014), New Hampshire (August 2014), Pennsylvania (January 2015), Indiana (February 2015), Alaska (September 2015), Montana (January 2016), Louisiana (July 2016), Virginia (January 2019), and Maine (January 2019). In these states, estimates represent lives saved over the first four years with expansion fully in effect.
** Estimates for Idaho, Nebraska, and Utah are lives lost from 2014 to 2017. These states have adopted Medicaid expansion but have yet to implement it.
Source: CBPP calculations based on Miller et al. supplemental estimates.
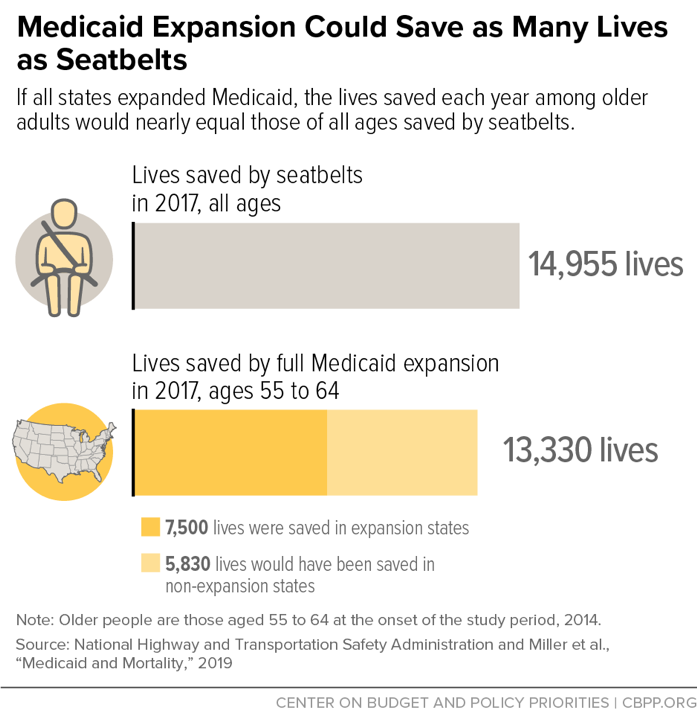
As our new paper explains, the study likely underestimates the lives saved by expansion because it doesn’t capture the policy’s long-term benefits or include certain expansion states. Nonetheless, expansion’s lifesaving potential ranks with other major public health interventions: if all states had expanded Medicaid, the lives saved just among older adults in 2017 would roughly equal the lives saved by seatbelts among the full population. (See figure below.)
The estimates translate to a 39 to 64 percent annual mortality rate reduction for low-income older adults who gained coverage. That’s almost as large as the gap in mortality rates between poor and middle-income older adults, showing that expanding Medicaid can sharply reduce health disparities.
This research is only one of many recent studies that show how Medicaid expansion is improving health and well-being. For example:
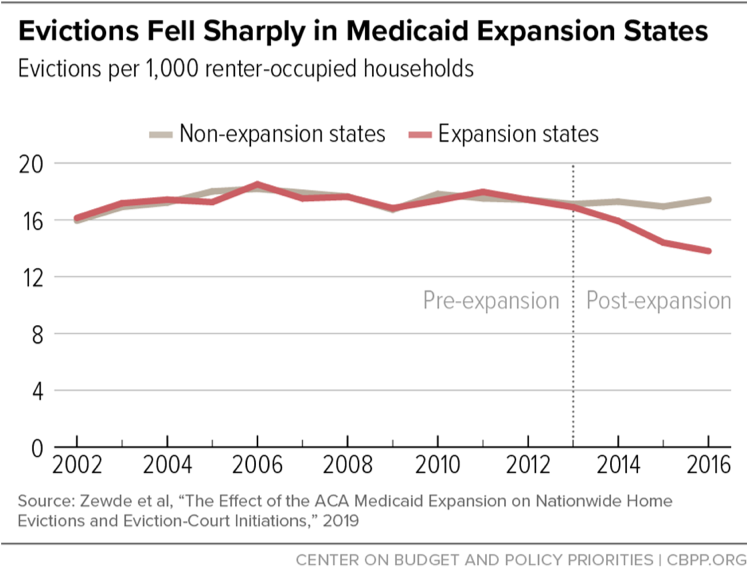
- Preventing evictions. A study last month in the National Journal of Public Health finds that evictions fell about 20 percent in expansion compared to non-expansion states (see figure), while another study in Health Affairs finds similar effects from California’s Medicaid expansion. While earlier studies found that expansion reduces medical debt and improves low-income households’ access to credit, the new studies document that improved financial security is helping people avoid one of the most harmful consequences of financial stress. After eviction, renters often end up in homeless shelters, extremely poor-quality housing, or dangerous neighborhoods, or they must move frequently among homes of family and friends. All of these outcomes can cause long-term harm, especially for children.
- Additional evidence of lives saved. Corroborating the mortality study’s findings discussed above, two other recent studies find that Medicaid expansion reduced mortality from specific, serious health conditions that people can manage with appropriate medical treatment. A 2018 JAMA study finds an almost 10 percent reduction in one-year mortality from end-stage renal disease (kidney failure) in expansion compared to non-expansion states, with larger improvements for African Americans (who are at higher risk for kidney failure). A 2019 JAMA Cardiology study finds a roughly 3 percent reduction in cardiovascular deaths.
- Improving quality of care. Even when the uninsured receive care for acute health needs, the quality of care and health outcomes may be worse because problems are detected later, patients can’t afford appropriate follow-up care, or for other reasons. Several recent studies document how Medicaid expansion addresses these shortcomings, showing that it’s increasing early-stage cancer diagnoses as well as the share of people getting surgical care consistent with clinical guidelines, such as less invasive surgical techniques when feasible.
- Expanding access to treatment for opioid use disorder. A 2018 Journal of Health Economics study finds that Medicaid expansion increased treatment facility admissions in which patients were given medication assisted treatment (MAT) — the gold standard treatment for opioid use disorder — by about 50 percent. While earlier research showed that Medicaid expansion led to large increases in Medicaid-financed MAT prescriptions, the newer study looks at MAT treatment across all payers, concluding that expansion drove a rise in the total number of people getting help, not just the share of treatment covered by Medicaid.
Our Medicaid expansion chartbook summarizes this and other research.
These findings should give the 14 states that haven’t yet decided to expand Medicaid more reason to do so. They should also finally put to rest claims that Medicaid doesn’t provide quality coverage, such as Centers for Medicare & Medicaid Services Administrator Seema Verma’s suggestion that Medicaid gives low-income adults “a[n] insurance card without care.” Instead, the evidence shows, Medicaid expansion lets low-income adults get preventive services, medications, and other care they couldn’t otherwise, and lets them get the care they need without incurring burdensome medical debt. And we now know that it’s sometimes literally a matter of life and death, particularly for people with serious but treatable health needs.