off the charts
POLICY INSIGHT
BEYOND THE NUMBERS
BEYOND THE NUMBERS
Health Reform’s Medicaid Expansion a Plus for States
Receive the latest news and reports from the Center
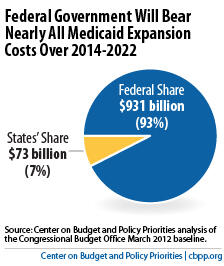
In fact, states — and their residents — will benefit in a number of ways from the expansion, and the federal government will pick up almost all of the tab, as our report explains.
Under health reform, Medicaid and the Children’s Health Insurance Program (CHIP) will cover an estimated 17 million more low-income adults and children by 2022, most of whom are now uninsured. States will bear little of the cost:
Health reform will also save states money in a number of ways. States and localities pay for many health services for the uninsured: they paid more than $10 billion toward hospital care for the uninsured in 2008, for example, and provided nearly $15 billion in funding for state mental health agencies in 2006.
In 2014, when millions of the uninsured qualify for Medicaid, the federal government will pick up a substantial share of these costs. In fact, Urban Institute researcher John Holahan has observed that states’ savings on care for the uninsured may fully offset their new costs related to the Medicaid expansion.