off the charts
POLICY INSIGHT
BEYOND THE NUMBERS
BEYOND THE NUMBERS
Legislation to help address the opioid epidemic that Congress plans to consider in the coming days includes several provisions enhancing Medicaid’s role in providing comprehensive access to treatment for substance use disorders (SUDs). But states don’t need to wait for this legislation to expand access to opioid treatment through Medicaid. They can take four steps right now:
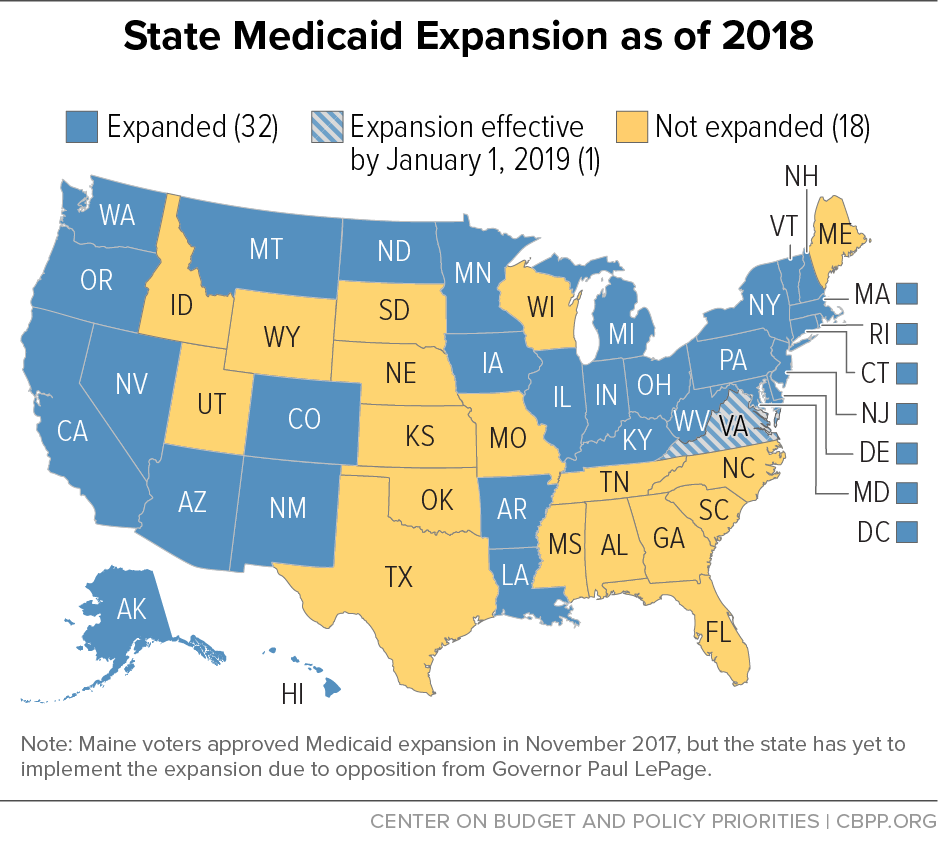
- Expand Medicaid. By itself, having an SUD isn’t considered a disabling condition so, before the Affordable Care Act (ACA), low-income adults with SUDs didn’t qualify for Medicaid unless they also had a serious mental or physical health condition. Now, in states that adopt the ACA’s Medicaid expansion, adults with incomes below 138 percent of the poverty line can enroll regardless of disability. That has enabled millions of people with behavioral health conditions, including opioid disorders, to gain health coverage. In expansion states, the share of people with substance use or mental health disorders who were hospitalized but uninsured fell from about 20 percent in 2013 to 5 percent by mid-2015. But 18 states still haven’t expanded Medicaid.
- Provide access to a full continuum of SUD services. State Medicaid programs can cover a broad range of SUD treatment services, including recovery services such as peer supports, supported employment, and case management; inpatient treatment; emergency detoxification; counseling; and clinical care. Moreover, both the Obama and Trump Administrations have issued guidance allowing states to use flexibility under federal waivers to spend federal Medicaid funds on short-term residential treatment for people with SUDs. Fifteen states have federally approved SUD waivers, and 11 states have waivers pending with the Department of Health and Human Services.
- Reduce barriers for Medicaid beneficiaries to access substance use treatment. Nearly 90 percent of people who needed SUD treatment in 2014 didn’t receive it. State Medicaid agencies can improve access to SUD treatment services such as medication assisted treatment (MAT), which combines medication with therapy. States should eliminate unnecessary barriers to getting MAT and other needed services, such as requiring prior authorization from the state or Medicaid managed care plan.
- Enforce the 2008 Mental Health Parity and Addiction Equity Act. This law requires health plans (including Medicaid plans) to provide mental health and substance use treatment services in “parity” with medical and surgical services. That means they must provide behavioral health services, such as psychotherapy or antipsychotic medications, to the same extent as similar physical health services, such as physical therapy or cancer drugs. The law also prohibits plans from placing greater limits on behavioral health services than on medical and surgical benefits — either financial limits (such as copays or caps on the number of appointments) or treatment limits (such as stricter prior authorization requirements for behavioral health services). Federal regulations from 2016 require state Medicaid agencies to ensure that their managed care plans comply with the parity requirements, but Medicaid beneficiaries still report significant challenges in getting behavioral health services.
Topics:
Policy Basics
Health
Report
Final Opioid Package Should Include Several Medicaid Provisions That Improve Access to Care
September 18, 2018
Stay up to date
Receive the latest news and reports from the Center