BEYOND THE NUMBERS
The House Energy and Commerce Committee’s Health Subcommittee will hold a hearing tomorrow to consider the EMPOWER Care Act, which would reauthorize and fund the successful, cost-effective Money Follows the Person (MFP) demonstration through 2022. Since 2007, MFP has helped over 75,000 Medicaid beneficiaries in 44 states who need long-term services and supports (LTSS) transition from institutions back to their own homes and communities. MFP funding expired on September 30, 2016 and, while states can spend unused 2016 MFP funds through September 30, 2020, they’ll likely start to scale back their transition activities due to funding constraints.
MFP not only helps people live outside institutions; it has saved the states and the federal government money. From 2008 to 2013, MFP generated $978 million in reduced Medicare and Medicaid costs after the first year of transitioning MFP participants out of institutions and into home- and community-based care. MFP gives states federal funds to help “rebalance” how they provide long-term services and supports, moving such services from nursing homes and other institutions to people’s homes and communities — where it’s not only more cost-effective but also where most people want to live, improving their quality of life. The demonstration has played a significant role in Medicaid’s 30-year shift in funding long-term services and supports from nursing homes to home- and community-based settings.
Recent evaluations of MFP show that:
- Early access to community-based LTSS minimizes the length of institutional stays and increases the likelihood that beneficiaries will return to the community. Beneficiaries who started to receive LTSS in the community before an institutional stay were three times likelier to return to the community after an institutional stay than those who started receiving LTSS in an institution.
- Compared to others who transition out of institutions, MFP participants are less likely to be readmitted to institutional care after their initial transition to the community.
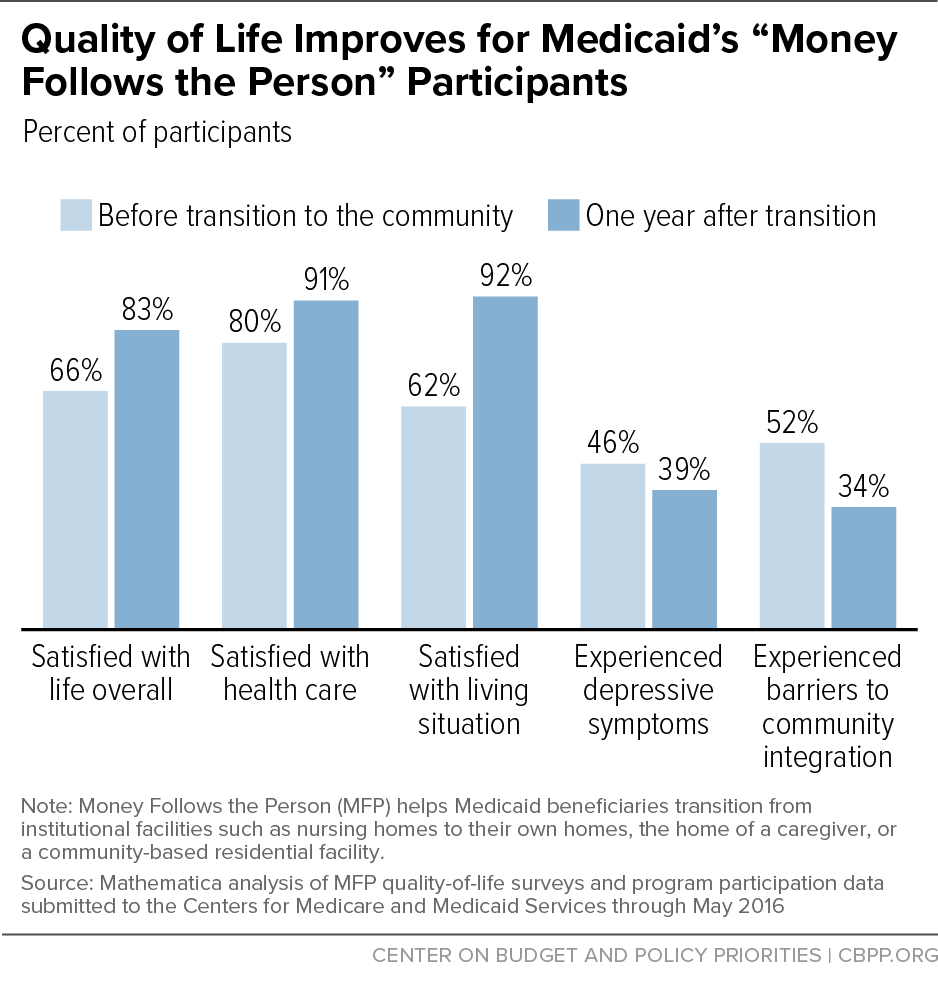
- MFP also has improved participants’ quality of life, with 92 percent reporting that they liked where they lived one year after entering community living, a 30-percentage-point increase compared to when they were receiving institutional care. (See chart.)
- MFP generated an 18-percentage-point decline in barriers to transitioning beneficiaries from institutions back to their homes and communities to get the care they need, also known as “community integration.”
- The more integrated that MFP participants are in their communities, the less likely they are to have symptoms of depression compared to participants who aren’t as integrated.
Restoring MFP funding would ensure continued progress in improving health outcomes and driving greater value in Medicaid.