más allá de los números
Emergency Vouchers Can Help Seniors and People With Disabilities Live in Safer, Community-Based Settings
As of July 1 public housing agencies can begin using the American Rescue Plan’s 70,000 emergency housing vouchers to serve people experiencing or at risk of homelessness — including many seniors and people with disabilities living in institutional care. Communities can couple these with Medicaid-funded home- and community-based services (HCBS), which the Rescue Plan boosted funding for, to help more seniors and people with disabilities live in their own homes instead of in nursing homes, homeless shelters, and other congregate settings.
Lawmakers should build on these investments in forthcoming recovery legislation to fund additional vouchers for low-income people struggling to afford rent — and ultimately to all households that need them — and longer-term increases in HCBS funding. Taken together, these investments would help end homelessness and unnecessary institutionalization among seniors and people with disabilities.
Seniors and people with disabilities overwhelmingly want to live in their own homes instead of institutions such as nursing homes. People who have transitioned out of institutional and into community-based care report improved mental health and community integration. But the lack of affordable housing and access to HCBS (such as help with preparing meals, dressing, working, or remembering and attending appointments) has prevented many people from leaving nursing homes and other institutions and moving into safer, community settings. During the pandemic, this contributed to large numbers of older and disabled people being unnecessarily exposed to coronavirus while living in congregate settings, causing preventable loss of life. In fact, long-term care facilities account for 5 percent of total reported COVID-19 cases and nearly one-third of deaths, the most recently available data indicate.
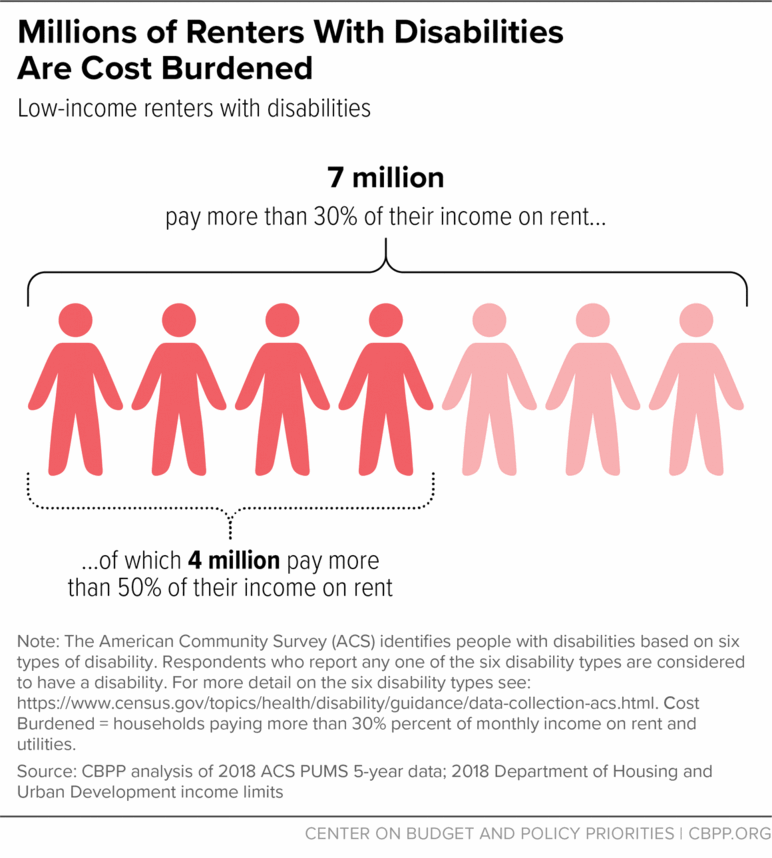
In addition, more than 4 million people with disabilities — including 1.4 million people ages 62 and older — are in low-income families paying more than half their incomes in rent and utilities. (See chart.) This puts them at risk of hardships such as eviction, food insecurity, and utility shutoffs that could jeopardize their health and access to services. And tens of thousands of disabled people continue to live on the streets or in homeless shelters where they face additional health risks that the pandemic has exacerbated.
The American Rescue Plan provides $5 billion in emergency housing voucher funding — enough for 70,000 vouchers. The new vouchers are for people facing some of the greatest hurdles to affordable housing: people experiencing or at high risk of homelessness. This includes people who have been living in an institutional care setting for 90 days or fewer who were homeless before entering the institution (who meet the definition of “homeless”), and people leaving institutional care after any length of time who are without a place to live (who are considered “at risk” of homelessness).
Therefore, many older and disabled people who need rental assistance to move out of nursing homes, psychiatric institutions, or other institutional care settings could benefit from these vouchers. Communities should also use thousands of available Mainstream vouchers — which are targeted to adults with disabilities under the age of 62 — to provide the housing stability needed to help more people transition out of institutional care settings or homelessness.
States and communities can use vouchers and Medicaid-funded services together to help more seniors and people with disabilities live in the community. Most states operate Money Follows the Person (MFP) programs, which help Medicaid enrollees transition out of institutional settings by coordinating services, locating housing, paying for home modifications to make housing accessible, and more. Since 2007 MFP has helped over 100,000 Medicaid beneficiaries in 44 states transition from institutional settings, but the lack of rental assistance has prevented many other eligible people from participating.
Emergency and Mainstream vouchers can help more Medicaid enrollees participate in MFP to transition out of institutions. And Medicaid-funded HCBS can provide the ongoing supportive services many older and disabled people need to maintain stability after a period of institutional care or homelessness.
As we explain in this blog post, the Rescue Plan provides a 12-month increase in federal Medicaid funding for HCBS, which could provide over $11 billion in additional federal funding. States must use the increased federal funds to supplement their current spending on HCBS and to enhance, expand, or strengthen their HCBS programs.
However, long-term investments will be needed to meet the growing demand for HCBS. For instance, President Biden proposed to expand access to HCBS and strengthen the direct care workforce. The Better Care Better Jobs Act, introduced by Senator Bob Casey in June, would carry forward this proposal by letting states continue to receive enhanced funding for HCBS, beyond 12 months, so that they can make more sustainable improvements including increasing access to services, ensuring adequate reimbursement rates, and strengthening data collection. Additional housing vouchers will also be needed to build a future in which people with low incomes have the rental assistance they need to access HCBS.