How Medicaid Work Requirements Will Harm Rural Residents – And Communities
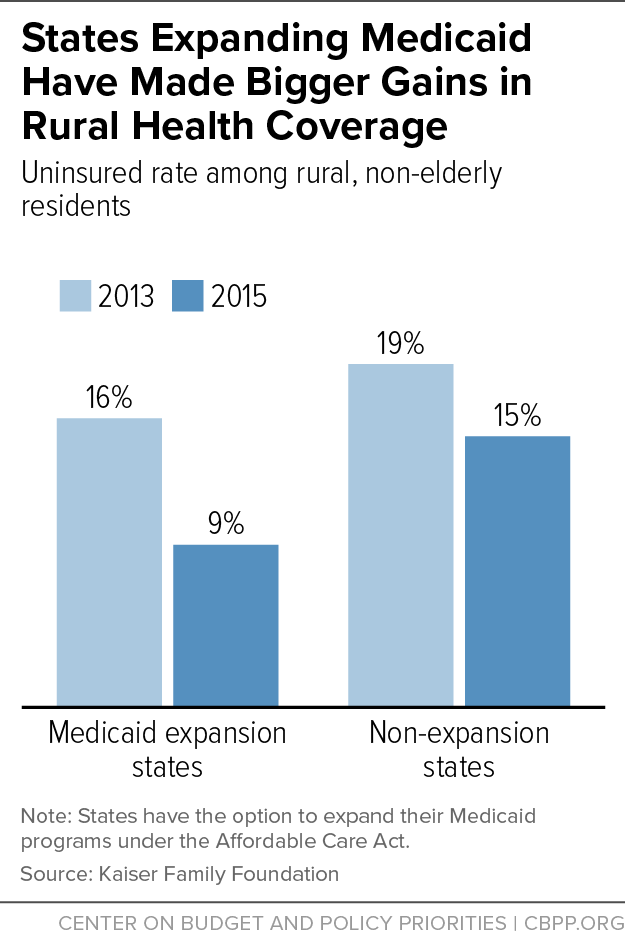
Medicaid plays an essential role in delivering health care in rural America and is an economic lifeline to many communities. Nearly 1 in 4 non-elderly adults in rural areas have health coverage through Medicaid. The Affordable Care Act’s (ACA) expansion of Medicaid to low-income adults has produced major benefits for rural America: in states that have adopted the expansion, rural areas have seen larger coverage gains than rural areas in non-expansion states, rural hospitals have experienced larger declines in uncompensated care costs, and fewer rural hospitals are closing.
But coverage for many rural Americans is at risk due to the Trump Administration’s decision to allow states, for the first time, to take away Medicaid coverage from people who don’t document that they are working or participating in work-related activities for a specified number of hours each month. These policies will especially harm rural America. Not only do many rural communities rely heavily on Medicaid, but rural unemployment is often higher, work can be more variable, and transportation and infrastructure challenges make it harder for people to comply with the requirements. These factors will cause large numbers of rural residents to lose health coverage, worsening access to care and exacerbating economic challenges for rural hospitals and providers.
The Administration is allowing states to impose work requirements on adult Medicaid enrollees other than those who are 65 or older, pregnant, or qualify for Medicaid because they receive disability benefits through the Supplemental Security Income program. Most of these policies require enrollees to document that they work or engage in other work activities (e.g., job training or volunteer work) for at least 80 hours per month, unless they prove that they qualify for limited exemptions. In Arkansas, the first state to implement such a policy, over 18,000 Medicaid beneficiaries lost coverage in 2018 due to the new requirements. While a federal court halted Arkansas’ policy, the Administration is continuing to approve similar policies in other states.
Medicaid Is Especially Important in Rural Communities
About 1 in 5 Americans live in rural areas, which have distinct economic and health conditions. Unemployment is higher and incomes are lower than in metropolitan areas, and rural employers are less likely to offer health insurance. These facts, plus the prevalence of farming and other forms of self-employment, mean Medicaid is often the only coverage option for low-income rural residents.
So it’s not surprising that Medicaid plays such an important role in delivering health care in rural America. Medicaid covered 24 percent of non-elderly adults in rural areas in 2015, versus 22 percent in urban areas. And the uninsured rate among rural, non-elderly individuals dropped much further in states that expanded Medicaid (from 16 percent in 2013 to 9 percent in 2015) than in non-expansion states (from 19 percent to 15 percent), as the graph shows.
Rural Residents at Particular Risk of Losing Coverage
Independent experts and states with work requirement proposals project that many Medicaid enrollees will lose coverage as a result of a work requirement and that most will end up uninsured. Kaiser Family Foundation researchers estimate that 1.4 to 4 million people would lose coverage if work requirements were imposed nationwide. People will lose coverage for a variety of reasons — for example, they can’t navigate paperwork requirements to claim an exemption for which they qualify, they can’t find work, or they can’t get enough work hours each month to meet their state’s threshold.
Meeting Medicaid work requirements will be especially difficult in rural economies, with their higher unemployment and lower labor force participation. In addition, most state work requirement proposals would take coverage away from people if they fail to document 80 hours of work or work activities each month. Yet many jobs in rural areas (like farming, manufacturing, and retail) have variable hours and above-average levels of involuntary part-time work and irregular scheduling. Thus, many working people in rural areas would risk losing health coverage, simply because they couldn’t obtain enough hours of work each and every month. Rural residents are also older, on average, than non-rural residents, and older Americans face particular challenges maintaining steady employment, such as work-limiting health conditions.
States adopting work requirements are also constructing administrative hurdles that create added barriers for rural residents. For example, Arkansas required enrollees to demonstrate compliance through an online portal, even though many Arkansans lack Internet access and, across the country, access to broadband is lower in rural areas.
Meanwhile, the Trump Administration isn’t requiring states implementing work requirements to provide any work supports — such as transportation assistance, child care, or job training — to help people meet the requirements. In fact, it specifically prohibits them from using federal Medicaid funding to do so. Transportation can be a particularly big barrier in rural areas, since there’s generally little or no public transportation and low-income residents may not have cars.
Coverage Losses Will Make It Harder for Rural Americans to Access Care
Rural residents who lose coverage due to these policies could face significant harm. Before the ACA, rural residents had higher rates of chronic health conditions and worse physical and mental health than their urban counterparts. Studies have found that Medicaid expansion increased the share of people with a personal physician, the share getting check-ups, and the share getting recommended preventive care such as cholesterol and cancer screenings, while lowering the share delaying care due to cost, skipping medications due to cost, or relying on the emergency room for care. Taking away coverage from people not meeting work requirements could reverse a large share of these gains.
Losing health coverage worsens health for all groups; that’s why physician organizations like the American Medical Association, American Academy of Family Physicians, American Academy of Pediatrics, and others oppose Medicaid work requirements. But coverage losses and interruptions in coverage are especially harmful for people with serious health needs. Loss of access to medications and other treatment can lead to serious deterioration in health, more emergency room visits and hospitalizations, and higher health care costs, research shows.
Exemptions for High-Unemployment Areas Won’t Mitigate Harm
Some state proposals include provisions that are supposed to make it easier for people living in areas with higher unemployment — which often include largely white and rural parts of the state — to meet the work requirements. But these carveouts won’t address the harm of a work requirement in rural areas. Some of them don’t exempt residents of areas with high unemployment from the work requirement; they simply expand the list of job-related activities that count toward the monthly requirement. And others only exempt a small number of rural residents.
Coverage Losses Will Add to Challenges Facing Rural Hospitals and Providers
In recent decades it’s become more challenging for rural hospitals and providers to remain in business because of a declining rural population, higher poverty rates, and lower levels of private insurance. But coverage gains under Medicaid expansion have helped many hospitals stay afloat, especially in rural areas. While both rural and non-rural hospitals in expansion states saw improvements in operating margins (that is, the difference between their revenue from providing services to patients and their total operating expenses) after the expansion, these gains were larger for rural hospitals. Most of the 121 rural hospitals that have closed since 2010 are in southern states that haven’t expanded Medicaid.
Work requirements could reverse a meaningful share of recent coverage gains in expansion states and cause coverage losses in other states, making it harder for rural hospitals to stay in business and continue serving their communities.