|
Revised September 28, 2006
NEW DEVELOPMENTS IN HEALTH SAVINGS ACCOUNTS:
HOUSE COMMITTEE APPROVES BILL, MAJOR NEW GAO STUDY
On September 27, the House Ways
and Means Committee approved H.R. 6134, which would make Health Savings Accounts
(HSAs) more attractive as tax shelters for high-income individuals. Ways and
Means Chairman Bill Thomas (R-CA) stated that the bill could be enacted before
the 109th Congress adjourns. The bill is particularly disturbing in light
of an important new Government Accountability Office (GAO) report finding that
HSAs already are used disproportionately by affluent households and provide
disproportionate tax subsidies to them. The GAO report also provides new
evidence that HSAs could raise the cost of health care for less healthy
Americans by encouraging “adverse selection.”
What Are Health Savings
Accounts?
Established by the 2003 Medicare
drug legislation, Health Savings Accounts (HSAs) are accounts in which
individuals who have a high-deductible health policy can save money to pay
out-of-pocket health expenses. In tax year 2006, someone who enrolls in a
health plan with a deductible of at least $1,050 for individual coverage and
$2,100 for family coverage may establish an HSA.
HSA contributions are tax
deductible and may be placed in stocks, bonds, or other investment vehicles,
with the earnings accruing tax free. Withdrawals also are tax exempt if used
for out-of-pocket medical costs. No other savings vehicle offers both
tax-deductible contributions and tax-free withdrawals. And since
there are no income limits on HSA participation, affluent individuals whose
incomes exceed IRA participation limits — or who have “maxed out” their IRA or
401(k) contributions — can use HSAs to shelter more money. As a result,
many analysts have warned that HSAs are likely to be used extensively as tax
shelters by high-income individuals.
What Would the House HSA Bill
Do?
The bill approved by the Ways and
Means Committee would make HSAs even more attractive as tax shelters to
high-income households, in two ways:
- Relaxing the HSA contribution
limits. Currently, the amount that HSA participants can contribute to their
account each year is limited to the amount of the deductible in their health
insurance plan or the statutory limit on HSA contributions ($2,700 for
individuals and $5,450 for family coverage in 2006), whichever is lower.
The bill would allow all HSA participants to contribute up to the statutory
limit, irrespective of the deductible in their health plan.
Under the bill, some
high-income individuals who may wish to use an HSA as a tax shelter but whose
contributions are currently limited by their health plan’s deductible would be
able to contribute considerably more to their account. The likely result would
be to induce more high-income individuals to establish an HSA and to increase
the amounts that high-income HSA participants contribute. Furthermore, since
these individuals would be contributing funds not needed to cover health
costs incurred under their deductible, a substantial share of the additional
contributions would likely be used for tax-sheltering purposes.
This provision also
would likely lead to an increase in health care spending by individuals
with HSAs, undermining the rationale advanced for HSAs in the first place — that
they can reduce health care expenditures. There are two reasons why:
-
HSAs provide a tax subsidy for
virtually any out-of-pocket health care costs, including elective
procedures not normally covered by health insurance. By enabling individuals to
“overfund” their HSAs (contributing up to $5,450 annually for family coverage
while facing a deductible as low as $2,100 for such coverage), the bill could
encourage some people to spend a portion of their excess HSA balances on
elective services they would not otherwise consume.
-
HSA proponents have argued that the
high deductibles required under HSA-eligible plans encourage people to limit
their health care use to necessary, cost-effective services (although many
health care analysts question this claim). The current rule tying the HSA
contribution limit to the amount of the deductible gives HSA participants an
incentive to choose plans with higher deductibles, because the higher the
deductible, the larger the HSA contribution allowed. By severing this link, the
House bill would encourage individuals with HSAs to switch to plans with lower
deductibles, thereby weakening whatever incentives the high deductibles may
provide in curbing health care expenditures, and leaving HSAs exposed primarily
as tax shelters.
- Allowing one-time transfers of
funds from Individual Retirement Accounts (IRAs) to HSAs. Under current
law, individuals generally may not withdraw funds from IRAs for purposes other
than retirement without paying income taxes and a financial penalty. The House
bill would add an exemption to this rule by allowing individuals, on a one-time
basis, to transfer funds from an IRA to an HSA without tax or penalty, so long
as their total contributions to the HSA that year do not exceed the HSA
contribution limit.
This would allow people to convert several thousand dollars in tax-deferred
savings into entirely tax-free savings by shifting them from an IRA to a
traditional HSA. That is because unlike IRA withdrawals in retirement, which
are taxed as ordinary income, HSA withdrawals in retirement are tax-free as long
as they do not exceed a family’s out-of-pocket health care costs that year.
The change would
primarily benefit high-income individuals, since they are the people most likely
to make such a transfer. Data on IRAs show that high-income individuals are
much more likely to have IRA accounts than the less affluent and make larger
contributions to them.
The change also could
open the door to future exemptions that allow people to transfer funds from IRAs
— or 401(k) plans, which have the same tax-deferred treatment as traditional
IRAs — to HSAs on an ongoing basis. That could cause substantial
long-term budgetary damage. If individuals can avoid taxation of significant
savings by transferring them from tax-deferred IRAs and 401(k)s to tax-free
HSAs, the already alarming budget forecast for coming decades will grow still
worse.
What Does the New GAO Report
Tell Us About Actual HSA Use?
Until recently, little or no solid data have been available to assess whether
HSAs are being used disproportionately by affluent individuals. The new GAO
study breaks new ground, by providing data from the Internal Revenue Service on
all Americans who made HSA contributions in 2004. The GAO study also contains
data from three large employers who offer both HSA-eligible plans and
traditional coverage on which option their employees have chosen. (To
supplement these data, the GAO conducted focus groups of individuals at these
three firms.) Finally, the GAO reviewed data on enrollment in HSA-eligible
plans from several national surveys of employers.
As
the first solid, broad-based data on actual HSA use by people in different
income groups, the GAO findings are now the premier data in the field to
determine whether HSAs are being disproportionately used by high-income
households. The GAO’s principal findings are:
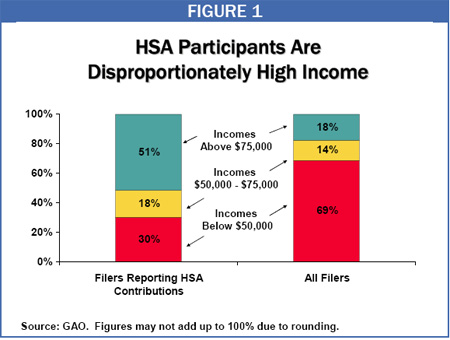
- HSA participants are
disproportionately high-income. People with adjusted gross income of more
than $75,000 made up 51 percent of all HSA participants in 2004 but only 18
percent of all tax filers under age 65. (At the other end of the income scale,
people with incomes below $30,000 made up half of all tax filers but only 16
percent of all HSA participants.) Moreover, the average adjusted gross income
of tax filers reporting HSA contributions in 2004 was $133,000, as compared to
$51,000 for all tax filers under age 65.
-
Many HSA participants appear to be
using their accounts purely as a tax shelter. About 55 percent of tax
filers reporting HSA contributions in 2004 did not withdraw any funds
from their accounts and “appeared to use their HSA as a savings vehicle,”
according to the GAO. Moreover, the GAO reported that when individuals are
given a choice between HSA plans and more traditional health insurance plans,
HSA plans attract “higher-income individuals with the means
to pay higher deductibles and the desire to accrue tax-free savings.”
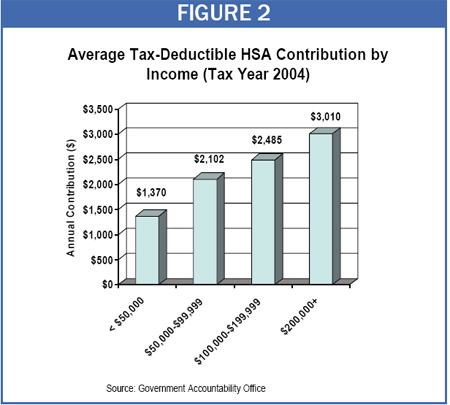
- High-income HSA participants
contribute much more to their accounts than other participants. HSA
participants who had incomes over $200,000 contributed an average of $3,010 to
their accounts in 2004, more than double the average contribution of $1,370 for
HSA participants who had incomes below $50,000. The fact that higher-income
individuals not only are more likely to have HSAs but also contribute more to
their accounts further skews the tax benefits of HSAs to high-income households,
as does the fact that higher one’s tax bracket, the richer the subsidy that HSAs
provide.
- HSAs reduce costs for the healthy,
but raise costs for the less healthy. The GAO compared the total
out-of-pocket costs (premiums, deductibles, and co-payments) that would be
incurred under the traditional plans and HSA-eligible plans offered by three
large employers. It found that healthy enrollees who use little health care
would tend to incur lower costs under the HSA-eligible plans, while people who
use more extensive health care services would tend to incur higher costs under
the HSA plans. Consistent with this finding, HSA participants in the GAO focus
groups said they would recommend HSAs to healthy people but would not
recommend such plans “to those who use maintenance medication, a chronic
condition, have children, or may not have the funds to meet the high
deductible.”
- HSAs are likely to provoke “adverse
selection.” Health policy experts have long counseled policymakers to avoid
the separation of healthier and less-healthy people into separate insurance
arrangements. The GAO report essentially warned that HSAs may bring this about
on a significant scale: “when individuals are given a choice between
HSA-eligible and traditional plans . . . HSA-eligible plans may attract
healthier individuals who use less health care or, as we found, higher-income
individuals with the means to pay higher deductibles and the desire to accrue
tax-free savings.” When less-healthy individuals are no longer pooled with
healthier people, they can become too costly to insure, leading to an increase
in the number of Americans with below-average health who are uninsured or
underinsured.
- HSAs have not led to greater
consumer “shopping” for health care. The GAO found that “contrary to the
hopes of CDHP [Consumer-Directed Health Plan] proponents, few of the
HSA-eligible plan enrollees who participated in our focus groups researched cost
before obtaining health care services,” other than for prescription drugs. The
GAO noted that accordingly to CDHP proponents, such research is necessary if
HSAs and other consumer-driven health care approaches are going to reduce health
care spending, as proponents claim.
In sum, evidence suggests that HSAs already are
of disproportionate benefit to high-income taxpayers and are being used by many
participants primarily as tax shelters. The House bill would
exacerbate both of these problems.
End Notes:
For a more complete discussion of the issues in this summary, see the
following Center reports: Edwin Park and Robert Greenstein, “GAO Study
Confirms Health Savings Accounts Primarily Benefit High-Income Individuals,”
September 20, 2006, and Edwin Park, Robert Greenstein, and Joel Friedman,
“House Bill Would Make Health Savings Accounts More Attractive as Tax
Shelters for High-Income Individuals,” revised September 28, 2006. The House
bill also contains several smaller HSA provisions.
An individual making such a transfer would have to remain enrolled in a
HSA-eligible high-deductible health plan for at least 12 months.
|

