IS MISSOURI’S
MEDICAID PROGRAM OUT-OF-STEP AND INEFFICIENT?
By
Leighton Ku and Judith Solomon
| PDF of report |
| If you cannot access the files through the links, right-click on the underlined text, click "Save Link As," download to your directory, and open the document in Adobe Acrobat Reader. |
Governor Matt Blunt has proposed substantial cuts in
- 61,000 low-income parents — mostly working mothers — with incomes between 30 percent and 75 percent of the poverty line (between $4,800 and $12,100 per year for a family of three), after certain deductions;[2]
- 4,600 senior citizens and people with permanent disabilities with incomes from $6,900 per year (for an individual) to $9,600;
- 9,500 low-income workers who have disabilities;
- 3,000 working people with temporary disabilities (receiving medical assistance under General Relief);
- 1,150 people who recently left welfare for work;
- 13,600 children and adults who would lose coverage because of stricter application requirements and increased paperwork; and
- 24,000 children who would lose Medicaid (MC+) coverage because their families are unable to pay increased premiums.
The Governor has also proposed to reduce significantly the health benefits covered by Medicaid, eliminating items such as crutches, wheelchairs and dental care for adults. He also has proposed to increase the amount that the poor must pay for medical care services by raising copayments.[3]
Even deeper cuts have been placed on the table since the Governor first presented these proposals in January. On March 24, the Governor proposed further reductions in Medicaid. These reductions, which are now under consideration in the Missouri House, would reduce the Medicaid income eligibility limit for parents even further to the minimum level permitted under federal law. The new income level would equal 22 percent of the poverty line for a family of three, $3,500 a year after deductions and would end coverage for an additional 7,500 extremely poor parents. (While the Governor’s office stated the new income level would equal 23 percent of the poverty line, examination of the proposal shows that the new income level for a family of three would be 22 percent of the poverty line.[4])
Furthermore, the Missouri Senate added a provision to the bill terminating
the Medicaid program after June 2008, and that provision is included in
the bill now moving through the Missouri House. Under the provision, a
commission would be charged with producing a design by
The proposed Medicaid cuts under consideration in
The reasons offered by Governor Blunt for these deep cuts are that
Missouri’s Medicaid program is too expensive — he has said it is the second
costliest program in the nation — and is inefficient.[6]
Are these claims valid? This brief analysis reviews evidence about
Is
Governor Blunt claims that cutting Medicaid expenditures is
necessary, because spending on Medicaid is affecting the state’s ability to
fund education and other state priorities. Governor Blunt claims that
In claiming that
When comparing the percentage of state general fund expenditures that are
spent on Medicaid,
A fairer comparison of the cost of Medicaid in
In
terms of state general fund Medicaid expenditures per state resident,
In
terms of state general fund Medicaid expenditures as a share of state personal
income,
Is
There is no question that
In fact, national studies demonstrate that Medicaid is less expensive than private health insurance and that Medicaid costs have been growing less rapidly in recent years than private health insurance.
- A study by Urban Institute economists Jack Hadley and John Holahan found that the average amount Medicaid spends on medical costs for adults is 30 percent less than the amount that would be spent if the same people were instead covered by private health insurance.[14]
- Another Urban Institute study conducted by Holahan found that per-person Medicaid expenditures for health care services rose 6.9 percent per year from 2000 to 2003, about half the 12.6 percent annual growth in premiums for employer-sponsored health insurance.[15]
In addition,
Contrary to the Governor’s claims,
Health Coverage in Missouri Will Erode Further if the Proposed Cuts are Made
Historically,
Since 2001, however, insurance coverage in
The erosion in health insurance coverage in
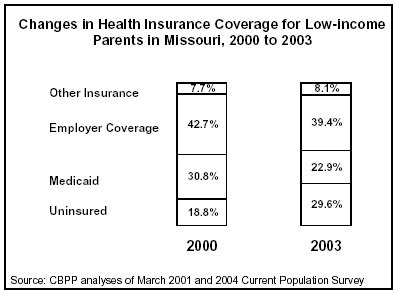 Census data reveal that while 32 percent of
Census data reveal that while 32 percent of
Governor Blunt has proposed making even deeper cuts in the eligibility of low-income parents, slicing the eligibility limit from 75 percent of the poverty line to 30 percent. If approved, this will be the deepest cut in Medicaid eligibility for working families instituted by any state.
Cutting eligibility for working parents to 30 percent of the poverty line will
penalize working parents, primarily mothers, who are working in low-wage jobs
and struggling to stay off welfare. A mother who heads a family of three who
earns over $4,800, after deductions, would make too much money to qualify for
Medicaid under the Governor’s proposal. If
About 125,000 people — primarily members of low-income working
families, retirees and people with disabilities — will lose Medicaid coverage
if Governor Blunt’s proposals are adopted. This will eliminate Medicaid
coverage for about one of every eight Medicaid beneficiaries. The cuts will
fall entirely upon the poorer half of the
|
Ending Medicaid, But Replacing It with What? The legislation that the Missouri Senate has approved would eliminate Missouri’s Medicaid program on June 30, 2008. The bill moving through the Missouri House also contains this provision. The legislation would establish a commission to make recommendations for a “new, innovative state Medicaid healthcare delivery system” by January 1, 2006. The termination of Medicaid would not be conditional, however, on enactment of some type of replacement program. A Medicaid reform commission also was created in Ohio, but that commission, and reform efforts in other states, have never operated in the context of a pre-ordained result that the current Medicaid program is to be scrapped. Moreover, the commission is Missouri would be created at the same time that severe cuts were being made in the state’s Medicaid program, limiting the commission’s flexibility to fashion recommendations that could meet the needs of the elderly, people with disabilities, children and families in Missouri. The brief description in the legislation of the alternative system that the commission would be charged with designing suggests that the establishment of such a system would necessitate a waiver from the federal Department of Health and Human Services. The new alternative could sharply limit eligibility or benefits, reduce funding for health care providers, cap enrollment, or place a cap on total funding for the program. |
Medicaid Cuts Would Weaken Missouri’s Economy and Employment
Governor Blunt proposed to cut $626 million in total Medicaid
expenditures (including expenditures financed by federal funds) in 2006, as
compared to the amount that would be spent without the cuts. The federal
matching rate for
The federal Medicaid funds that would be lost as a result of the proposed cuts provide revenue to hospitals, clinics, pharmacies, nursing homes and other health care providers, and thereby contribute to the salaries of physicians, nurses, pharmacists, therapists and other health care personnel across the state. The effect of these federal funds is multiplied through the state economy as health care workers pay mortgages and rent, purchase food and other goods, and contribute to the broader economy.
A recent study, based on analyses by economists at
Conclusion
In promoting his proposals
to cut Medicaid, Governor Blunt has claimed that
The cuts proposed by the Governor and being considered by the legislature are considerably more severe than those being considered in most other states and would significantly increase the number of uninsured Missourians. In particular, the proposal to cut the income limit for parents to 30 percent of the poverty line and the subsequent proposal to lower the level even further to 22 percent of the poverty line appear to be unprecedented and would be the harshest cuts aimed at working parents that any state has ever instituted. The cutbacks also would have a deleterious effect on the state economy, as a result of the loss of hundreds of millions in federal matching funds.
End Notes:
[1] The proposals to lower the income eligibility limit for parents and shorten the transitional eligibility period for low-income workers do not require statutory authorization and will be considered in a separate budget bill.
[2] The current income limit of 75 percent of the poverty line, and the proposed limit of 30 percent of the poverty line, apply to family income after certain deductions (or “disregards”) are taken. These disregards are substantial for a parent’s first four months on the program, but drop substantially in the fifth month and drop further in the 13th month that a parent is on the program. After the first 12 months, the disregards equal $90 a month — or $1,080 a year — in earnings.
[3] Joel Ferber, “Reviewing The Impact Of Proposed Medicaid Cuts: A Preliminary Analysis, Legal Services of Eastern Missouri, Feb. 4, 2005; Missouri Legislature, Committee on Legislative Research, Oversight Division, “Fiscal Note for Perfected SB 559,” March 16, 2005; Joel Ferber, “The Impact of the SCHIP Cut,” Legal Services of Eastern Missouri, March 2005.
[4]
The Governor’s latest proposal would set the income eligibility limit for
parents at the state’s AFDC payment levels as of
[5]
Rachel Klein and Kim Jones, “Showdown in the Show-Me State”, Families
[6]
Matt Blunt, “2005 State of the State Address,”
[7] National Association of State Budget Officers (NASBO), 2003 State Expenditure Report, Oct. 2004.
[8] Cindy Mann and Fouad Pervez, "Medicaid Cost Pressures for States: Looking at the Facts." Georgetown University Health Policy Institute, January 2005.
[9] Analyses of NASBO data for 2003, op cit.
[10] Analysis of Census Bureau data on state and local expenditures and Bureau of Economic Analysis data on personal income for 2002.
[11] Analyses of SFY 2003 Medicaid state general fund expenditures as reported by NASBO and state population data from the Census Bureau.
[12] Analyses of NASBO data on SFY 2003 state general fund Medicaid expenditures and state personal income data from the Bureau of Economic Analysis.
[13]
Center on Budget and Policy Priorities, “Future Medicaid Growth Is Not Due
to Flaws in the Program’s Design, But to Demographic Trends and General
Increases in Health Care Costs”,
[14]
Jack Hadley and John Holahan, “Is Health Care Spending Higher under
Medicaid or Private Insurance?” Inquiry, 40:323-42, Winter
2003/2004. Similar findings were reached by federal researchers: see
Edward Miller, Jessica Banthin, and John Moeller, “Covering the Uninsured:
Estimates of the Impact on Total
[15] John Holahan and Arunabh Ghosh, “Understanding the Recent Growth in Medicaid Spending, 2000-2003,” Health Affairs, January 26, 2005; Kaiser Family Foundation, news release, “A Sharp Rise in Enrollment During the Economic Downturn Triggered Medicaid Spending to Increase by One-Third from FY 2000-03,” January 26, 2005.
[16]
Analyses of data from the FY 2002 Medicaid Statistical Information System;
this excludes expenditures for administration, disproportionate share
hospital payments, and certain other costs. The average expenditure per
enrollee is standardized to adjust for differences in the composition of
each state’s Medicaid caseload (i.e., in the proportion of beneficiaries
that are children, adults, seniors and people with disabilities). Without
standardization,
[17]
Joel Ferber, Heather Bednarek and Muhammad Islam, “The