Medicaid Expansion: Frequently Asked Questions
End Notes
[1] Jesse Cross-Call, “Medicaid Expansion Continues to Benefit State Budgets, Contrary to Critics’ Claims,” Center on Budget and Policy Priorities, October 9, 2018, https://www.cbpp.org/research/health/medicaid-expansion-continues-to-benefit-state-budgets-contrary-to-critics-claims.
[2] Bryce Ward, “The Impact of Medicaid Expansion on States’ Budgets,” Commonwealth Fund, May 5, 2020, https://www.commonwealthfund.org/publications/issue-briefs/2020/may/impact-medicaid-expansion-states-budgets,
[3] Manatt Health, “Assessing the Fiscal Impact of Medicaid Expansion Following the Enactment of the American Rescue Plan Act of 2021,” April 2021, https://www.manatt.com/Manatt/media/Documents/Articles/ARP-Medicaid-Expansion.pdf.
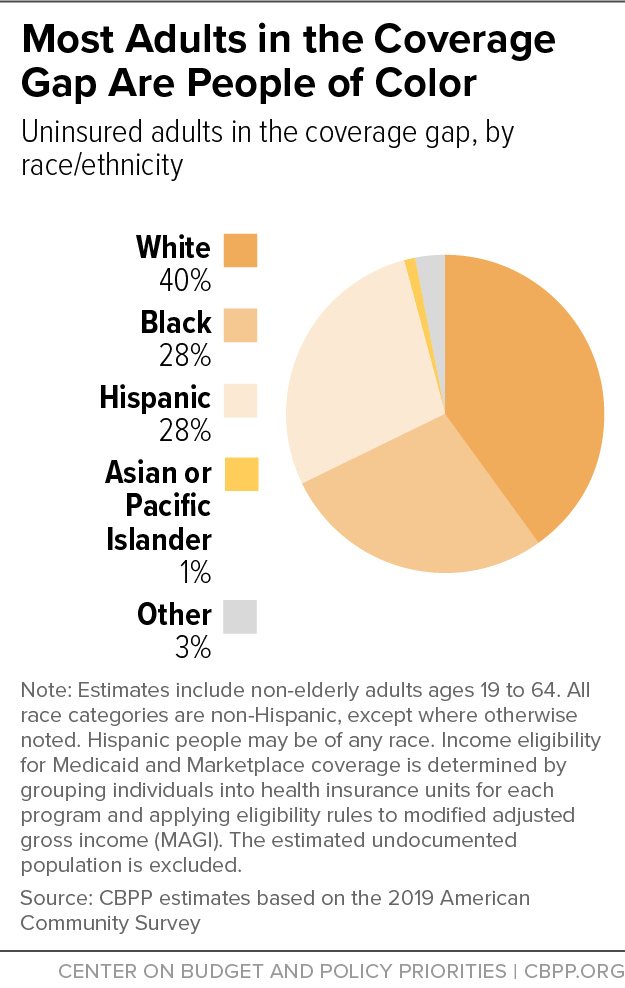
[4] Gideon Lukens and Breanna Sharer, “Closing Medicaid Coverage Gap Would Help Diverse Group and Narrow Racial Disparities,” Center on Budget and Policy Priorities, Revised June 14, 2021, https://www.cbpp.org/research/health/closing-medicaid-coverage-gap-would-help-diverse-group-and-narrow-racial.
[5] Rachel Garfield, Kendal Orgera, and Anthony Damico, “The Coverage Gap: Uninsured Poor Adults in States that Do Not Expand Medicaid,” Kaiser Family Foundation, January 21, 2021, https://www.kff.org/medicaid/issue-brief/the-coverage-gap-uninsured-poor-adults-in-states-that-do-not-expand-medicaid/.
[6] A notable exception is Wisconsin, which extends Medicaid eligibility to adults up to 100 percent of the poverty line through a federal waiver and is therefore not included in coverage gap estimates. The 2021 federal poverty guideline for a family of three is $21,960 for the 48 contiguous states and the District of Columbia.
[7] Judith Solomon, “Federal Action Needed to Close Medicaid ‘Coverage Gap,’ Extend Coverage to 2.2 Million People,” Center on Budget and Policy Priorities, May 6, 2021, https://www.cbpp.org/research/health/federal-action-needed-to-close-medicaid-coverage-gap-extend-coverage-to-22-million.
[8] Lukens and Sharer, op cit.
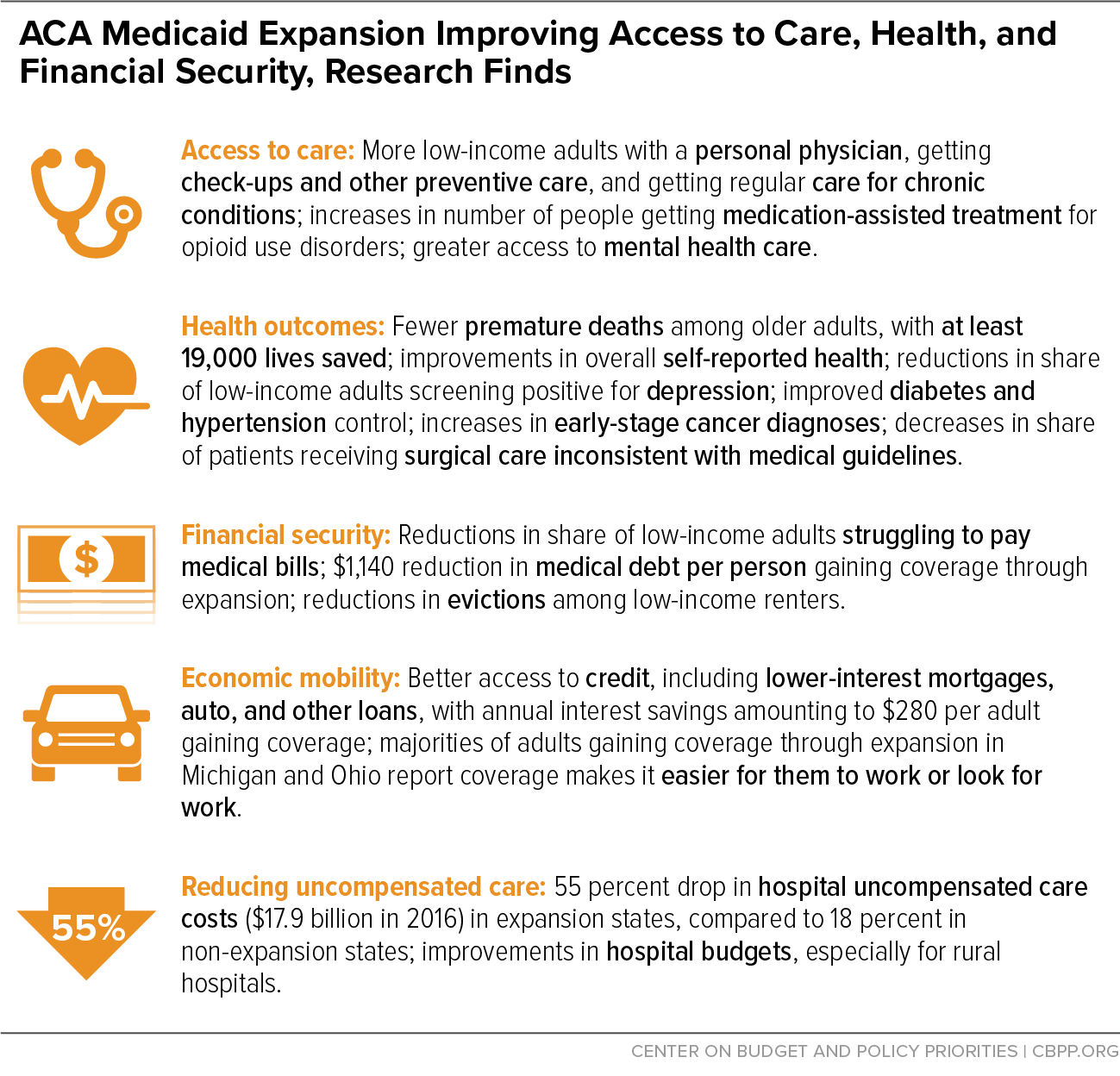
[9] Madeline Guth, Rachel Garfield, and Robin Rudowitz, “The Effects of Medicaid Expansion under the ACA: Studies from January 2014 to January 2020,” Kaiser Family Foundation, March 17, 2020, https://www.kff.org/medicaid/report/the-effects-of-medicaid-expansion-under-the-aca-updated-findings-from-a-literature-review/.
[10] Benjamin D. Sommers et al., “Three-Year Impacts of the Affordable Care Act: Improved Medical Care and Health Among Low-Income Adults,” Health Affairs, June 2017, https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0293.
[11] Susan Dorr Goold et al., “Primary Care, Health Promotion, and Disease Prevention with Michigan Medicaid Expansion,” Journal of General Internal Medicine, December 2019, https://link.springer.com/article/10.1007%2Fs11606-019-05370-3.
[12] Sommers et al., op cit.
[13] Justin M. Le Blanc et al., “Association of Medicaid Expansion Under the Affordable Care Act with Breast Cancer Stage at Diagnosis,” JAMA Surgery, July 2020, https://jamanetwork.com/journals/jamasurgery/article-abstract/2767686.
[14] Shailender Swaminathan et al., “Association of Medicaid Expansion With 1-Year Mortality Among Patients With End-Stage Renal Disease,” JAMA, December 2018, https://jamanetwork.com/journals/jama/fullarticle/2710505.
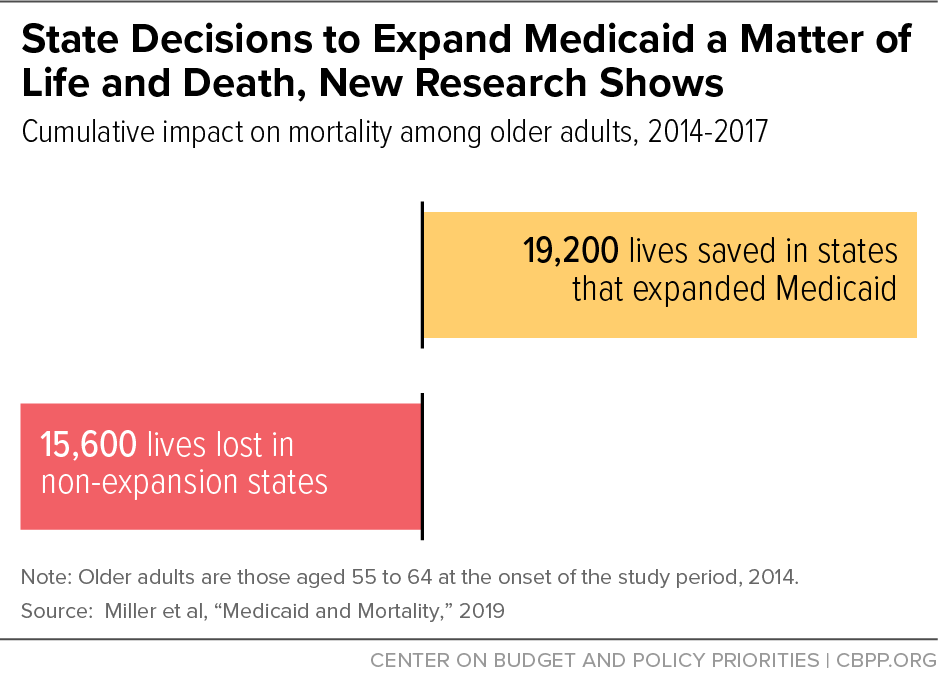
[15] Sarah Miller et al., “Medicaid and Mortality: New Evidence from Linked Survey and Administrative Data,” National Bureau of Economic Research Working Paper 26081, July 2019, https://www.nber.org/papers/w26081.
[16] Matt Broaddus and Aviva Aron-Dine, “Medicaid Expansion Has Saved at Least 19,000 Lives, New Research Finds,” Center on Budget and Policy Priorities, November 6, 2019, https://www.cbpp.org/research/health/medicaid-expansion-has-saved-at-least-19000-lives-new-research-finds.
[17] Before the ACA, low-income women were eligible for Medicaid while pregnant and for 60 days postpartum, but eligibility before and after pregnancy was very restrictive.
[18] Erica Eliason, “Adoption of Medicaid Expansion Is Associated with Lower Maternal Mortality,” Women’s Health Issues, February 2020, https://www.whijournal.com/article/S1049-3867(20)30005-0/fulltext.
[19] Chintan B. Bhatt and Consuelo M. Beck-Sagué, “Medicaid Expansion and Infant Mortality in the United States,” American Journal of Public Health, April 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5844390/.
[20] Rebecca Myerson, Samuel Crawford, and Laura R. Wherry, “Medicaid Expansion Increased Preconception Health Counseling, Folic Acid Intake, and Postpartum Contraception,” Health Affairs, November 2020, https://www.healthaffairs.org/doi/10.1377/hlthaff.2020.00106.
[21] Kenneth Brevoort et al., “Medicaid and Financial Health,” National Bureau of Economic Research Working Paper 24002, November 2017, https://www.nber.org/system/files/working_papers/w24002/w24002.pdf.
[22] Luojia Hu et al., “The Effect of the Patient Protection and Affordable Care Act Medicaid Expansions on Financial Wellbeing,” National Bureau of Economic Research Working Paper 22170, February 2018, https://www.nber.org/system/files/working_papers/w22170/w22170.pdf.
[23] Heidi Allen et al., “Early Medicaid Expansion Associated With Reduced Payday Borrowing In California,” Health Affairs, October 2017, https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0369.
[24] Heidi Allen et al., “Can Medicaid Expansion Prevent Housing Evictions?” Health Affairs, September 2019, https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2018.05071.
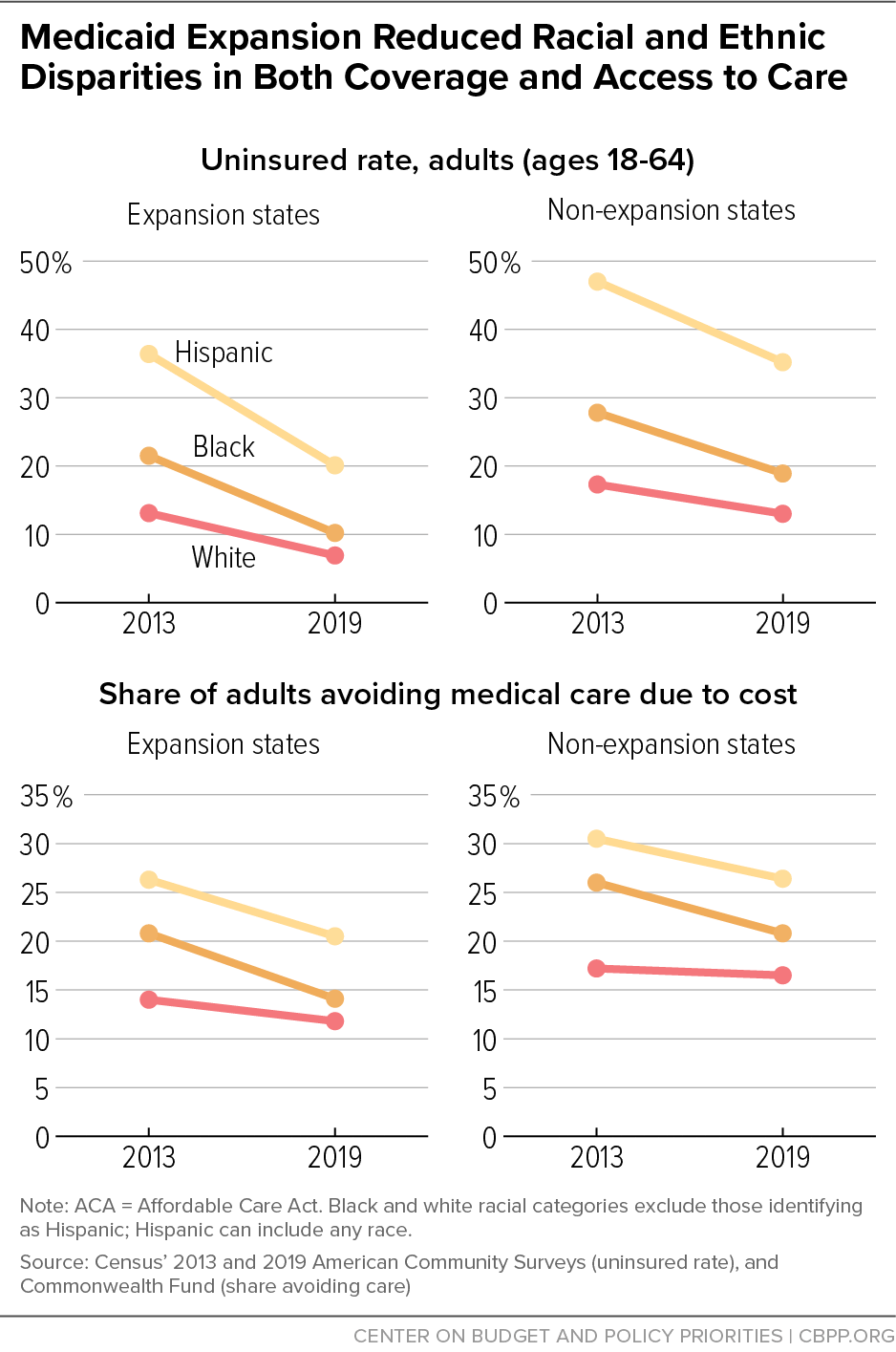
[25] Jesse C. Baumgartner., Sara R. Collins, and David C. Radley, “Racial and Ethnic Inequities in Health Care Coverage and Access, 2013-2019,” Commonwealth Fund, June 9, 2021, https://www.commonwealthfund.org/publications/issue-briefs/2021/jun/racial-ethnic-inequities-health-care-coverage-access-2013-2019.
[26] Kaiser Family Foundation, “Health and Health Care for American Indians and Alaska Natives (AIANS) in the United States,” May 10, 2019, https://www.kff.org/infographic/health-and-health-care-for-american-indians-and-alaska-natives-aians/.
[27] Lukens and Sharer, op cit.
[28] Shailender Swaminathan et al., op cit.
[29] Erica L. Eliason, “Adoption of Medicaid Expansion Is Associated with Lower Maternal Mortality,” Women’s Health Issues, February 25, 2020, https://www.whijournal.com/article/S1049-3867(20)30005-0/fulltext.
[30] Minal R. Patel et al., “Examination of Changes in Health Status Among Michigan Medicaid Expansion Enrollees From 2016 to 2017,” JAMA Network, July 10, 2020, https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2768102.
[31] Martha Heberlein et al., “Getting in Gear for 2014: Findings From a 50-State Survey of Eligibility, Enrollment, Renewal and Cost-Sharing Policies in Medicaid and CHIP, 2012-2013,” Kaiser Family Foundation, January 23, 2013, https://www.kff.org/medicaid/report/getting-into-gear-for-2014-findings-from-a-50-state-survey-of-eligibility-enrollment-renewal-and-cost-sharing-policies-in-medicaid-and-chip-2012-2013/.
[32] Lisa Dubay and Genevieve Kenney, “Expanding Public Health Insurance to Parents: Effects on Children’s Coverage under Medicaid,” Health Services Research, October 7, 2003, https://onlinelibrary.wiley.com/doi/abs/10.1111/1475-6773.00177.
[33] Julie Hudson and Asako S. Moriya, “Medicaid Expansion For Adults Had Measurable ‘Welcome Mat’ Effects on Their Children,” Health Affairs, September 2017, https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2017.0347?journalCode=hlthaff.
[34] Maya Venkataramani et al., “Spillover Effects of Adult Medicaid Expansions on Children’s Use of Preventive Services,” Pediatrics, December 2017, https://pediatrics.aappublications.org/content/140/6/e20170953.
[35] Lukens and Sharer, op cit.
[36] Molly O’Malley Watts, MaryBeth Musumeci, and Priya Chidambaram, “State Variation in Medicaid LTSS Policy Choices and Implications for Upcoming Debates,” Kaiser Family Foundation, February 26, 2021, https://www.kff.org/medicaid/issue-brief/state-variation-in-medicaid-ltss-policy-choices-and-implications-for-upcoming-policy-debates/.
[37] MaryBeth Musumeci, Molly O’Malley Watts, and Priya Chidambaram, “Key State Policy Choices About Medicaid Home and Community-Based Services,” Kaiser Family Foundation, February 4, 2020, https://www.kff.org/report-section/key-state-policy-choices-about-medicaid-home-and-community-based-services-appendix-tables/.
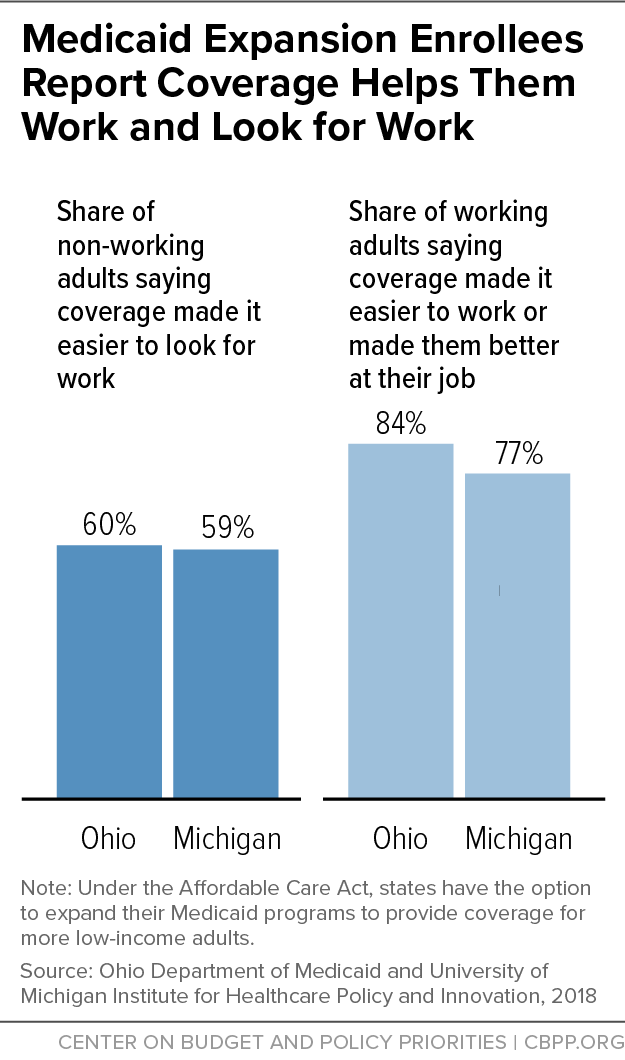
[38] Rachel Garfield et al., “Work Among Medicaid Adults: Implications of Economic Downturn and Work Requirements,” Kaiser Family Foundation, February 2021, https://www.kff.org/report-section/work-among-medicaid-adults-implications-of-economic-downturn-and-work-requirements-issue-brief/.
[39] For example, one study found that low-income workers in expansion states did not lose jobs, switch jobs, or change from full- to part-time work more frequently than low-income workers in non-expansion states. Angshuman Gooptu et al., “Medicaid Expansion Did Not Result In Significant Employment Changes Or Job Reductions In 2014,” Health Affairs, January 2016, https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2015.0747.
[40] Jean P. Hall et al., “Effect of Medicaid Expansion on Workforce Participation for People With Disabilities,” American Journal of Public Health, February 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5227925/.
[41] David Dranove, Craig Garthwaite, and Christopher Ody, “The Impact of the ACA’s Medicaid Expansion on Hospitals’ Uncompensated Care Burden and the Potential Effects of Repeal,” Commonwealth Fund, May 2017, https://www.commonwealthfund.org/publications/issue-briefs/2017/may/impact-acas-medicaid-expansion-hospitals-uncompensated-care.
[42] Fredric Blavin and Christal Ramos, “Medicaid Expansion: Effects on Hospital Finances and Implications for Hospitals Facing COVID-19 Challenges,” Health Affairs, January 2021, https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2020.00502.
[43] Richard C. Lindrooth et al., “Understanding The Relationship Between Medicaid Expansions And Hospital Closures,” Health Affairs, January 2018, https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0976.
[44] Cecil G. Sheps Center for Health Services Research, “Rural Hospital Closures,” accessed June 16, 2021, https://www.shepscenter.unc.edu/programs-projects/rural-health/rural-hospital-closures/.
[45] Michael Topchik et al., “The Rural Health Safety Net Under Pressure: Rural Hospital Vulnerability,” Chartis Center for Rural Health, February 2020, https://www.ivantageindex.com/wp-content/uploads/2020/02/CCRH_Vulnerability-Research_FiNAL-02.14.20.pdf.