Taking Away Medicaid for Not Meeting Work Requirements Harms Children
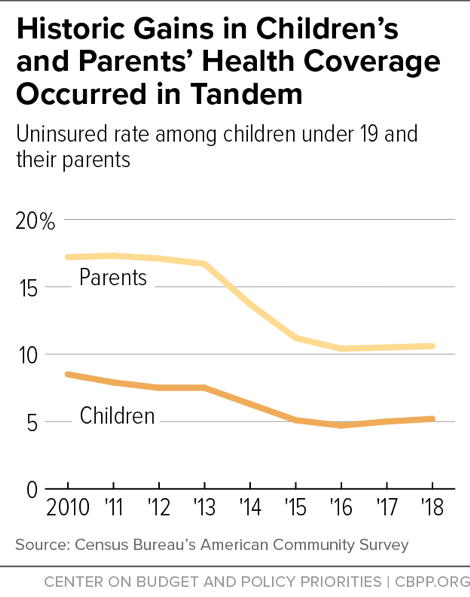
When parents have health insurance, their children are more likely to be insured, research shows. That’s a big reason why the Affordable Care Act’s (ACA) Medicaid expansion for parents and other adults significantly increased children’s health coverage, which helped drive the uninsured rate for children to a historic low (see chart). Unfortunately, the uninsured rate for children has since risen, from 4.7 percent in 2016 to 5.2 percent in 2018.
Now, the Trump Administration is letting states take away Medicaid coverage from people who don’t work a specified number of hours each month. That policy will cause many parents to lose coverage, which will harm their children as well. When parents lack health coverage, children are also more likely to go uninsured. Children also benefit directly when their parents can access the health care they need and have greater financial security, which is why parents losing coverage hurts children’s health and long-term development.
The Administration is letting states impose work requirements on adult Medicaid beneficiaries, other than those who are 65 or older, pregnant, or qualify for Medicaid because they are receiving disability benefits through the Supplemental Security Income program. In Arkansas, the first state to implement such a policy, over 18,000 Medicaid beneficiaries lost coverage in 2018 due to the new requirements. While a federal court halted Arkansas’ policy, the Administration is continuing to approve similar policies in other states. Many of these policies require enrollees to document that they work or engage in other work activities (e.g., job training or volunteer work) for at least 80 hours per month unless they prove that they qualify for limited exemptions.
Work Requirements Will Cause Parents to Lose Coverage
While some states’ work requirement policies exempt parents, others do not.
In states that expanded Medicaid under the ACA, both parents and adults without children with incomes up to 138 percent of the federal poverty line are eligible for Medicaid. Among expansion states with approved work requirement policies, some states (including Arkansas) generally exempt parents of minor children, but other states only exempt parents of children age 6 and under. In New Hampshire, which began implementing such a policy, almost 17,000 people, including parents of older children, would have lost coverage had state policymakers not put the policy on hold.
In states that haven’t expanded Medicaid, low-income parents are the primary target of work requirements, since adults without children are generally ineligible for Medicaid. Many of these states’ proposed work requirements would put parents in a catch-22: if they don’t comply, they’ll lose coverage, but if they do comply, they’ll likely still lose coverage because their income will exceed their state’s very low Medicaid eligibility limit.
For example, Mississippi is proposing to require parents with Medicaid coverage to participate in work-related activities, such as working 20 hours per week, volunteering, or participating in an alcohol or other drug abuse treatment program. But if a parent works 20 hours per week at the minimum wage, her monthly earnings would equal $580 — above Mississippi’s income limit of $468 per month for Medicaid eligibility for a family of three. Mississippi itself projects that about 8 percent of parents subject to the work requirement would lose coverage within the first year of implementation. Most of these parents would become uninsured, because the low-wage jobs they’d likely get may not offer health insurance and wouldn’t pay enough to raise their income above the poverty line so they could qualify for premium tax credits to help them pay for coverage in the health insurance marketplaces.
Requiring work or work-related activities as a condition of Medicaid eligibility will also make it harder for parents to stay covered even if they are already working or are supposed to qualify for exemptions. In many low-wage jobs, hours are volatile and job loss is common, meaning that even parents who work substantial hours over the course of the year may fall short of state work requirements in a particular month. Work requirements also make it harder for parents to stay enrolled because they will have to provide paperwork documenting their compliance or eligibility for exemptions. Red tape and paperwork requirements have consistently proved to reduce enrollment in Medicaid.
Documentation requirements are likely to be burdensome for parents of children with special health care needs. While they would qualify for exemptions in most states, they would have to prove they’re caring for a child with a disability or special health care need, adding one more burden for parents who already face major challenges.
When Parents Lose Coverage, Children Get Hurt
When parents lose health insurance coverage, children get hurt.
Children are less likely to get the care they need. Most children in low-income families were already eligible for Medicaid before the implementation of the ACA. A recent study shows, however, that Medicaid enrollment increased disproportionately for children whose parents became newly eligible. More than 700,000 children in Medicaid expansion states gained coverage from 2013 to 2015 — more than double the number of children in non-expansion states who gained coverage during this period. That’s consistent with earlier evidence that gains in coverage for parents translate into gains in coverage for children. Research also confirms that gains in coverage for parents, and the associated gains for children, improve children’s access to care. For example, increases in adult Medicaid eligibility are associated with a greater likelihood of children in low-income families receiving preventive care, according to a recent study, which finds that children are 29 percentage points more likely to have an annual well-child visit if their parents are enrolled in Medicaid. Unfortunately, undoing coverage gains for parents will likely undo gains for children as well.
Families are less financially secure. Losing coverage would also put children and their parents at risk of going without needed medical care and incurring significant medical debt for any care they do receive. Medicaid expansion led to a decrease in debts being sent to third-party collection agencies, and the share of low-income adults in Arkansas and Kentucky reporting that they had trouble paying their medical bills dropped by 25 percent. Financial insecurity doesn’t just affect adults — children’s development can be negatively affected by issues resulting from poverty, such as toxic stress.
Children’s health and development are at risk. Children’s health and development rely in part on their parents’ health and well-being, and research shows Medicaid expansion has improved access to care and health for low-income adults. Low-income adults in Arkansas and Kentucky saw significant gains in access to medical care and improvements in self-reported health compared to those in Texas, which hasn’t expanded Medicaid. And mental health outcomes improved among parents who gained Medicaid coverage prior to expansion. Healthy parents help ensure their children’s health and development as children’s relationships with their parents can influence their brain structure and function, and in turn, mitigate the negative effects of trauma or adverse childhood experiences, including poverty.
Coverage Losses Jeopardize Children’s Long-Term Health and Development
The potential loss of coverage for both children and their parents jeopardizes children’s long-term health and development. Children losing coverage would lose access to various important health services under Medicaid’s Early Periodic Screening, Diagnostic and Treatment (EPSDT) benefit. This benefit guarantees that children and adolescents under the age of 21 have access to a robust set of comprehensive and preventive health services, including regular well-child exams; hearing, vision, and dental screenings; and other services to treat physical, mental, and developmental illnesses and disabilities. The loss of EPSDT would be particularly harmful to children with special health care needs, as Medicaid serves as the sole source of coverage for over one-third of these children.
Medicaid coverage has a significant positive impact on children’s health not only while they’re enrolled, but also on their long-term outcomes. Children covered by Medicaid during their childhood have better health as adults, with fewer hospitalizations and emergency room visits, research shows. Moreover, children covered by Medicaid are more likely to graduate from high school and college, have higher wages, and pay more in taxes. Medicaid work requirements that cost parents their coverage will put low-income children’s short- and long-term health-related gains at risk.