
|
Revised February 22, 2007
FREEZING SCHIP FUNDING IN COMING YEARS WOULD
REVERSE RECENT GAINS IN CHILDREN'S HEALTH COVERAGE
By Matthew Broaddus and Edwin Park
Due in large part to the State Children’s Health Insurance Program (SCHIP), the percentage of low-income children in the United States without health coverage has fallen by one-third since SCHIP was created in 1997, despite the erosion of private health coverage over this period. More than 4 million low-income children, most of whom would otherwise be uninsured, are enrolled in SCHIP.[1]
This remarkable success, however, is now threatened. Unlike Medicaid, an entitlement program whose federal funding increases automatically to compensate for increases in health-care costs (as well as increases in caseloads), SCHIP is a block grant with a fixed annual funding level. Consequently, the federal SCHIP funding that states receive has not been keeping pace with the rising cost of health care or population growth.
In fiscal year 2007, the final year of SCHIP’s original ten-year authorization, many states are expected to have inadequate SCHIP funds to cover the same number of beneficiaries as in 2006.[2] We estimate, based on states’ most recent SCHIP spending projections for fiscal year 2007 and taking into account stop-gap SCHIP legislation enacted in December 2006, that 14 states will face a combined shortfall this year of nearly $745 million — equivalent to the average annual cost of covering 510,000 children through SCHIP in 2007.[3]
Shortfalls will become much more severe and widespread after 2007 if Congress freezes the annual SCHIP block grant at its 2007 level of $5.04 billion when it reauthorizes SCHIP this year. Because of how the federal budget baseline rules are constructed, the Congressional Budget Office baseline assumes SCHIP funding will remain frozen at its 2007 level for the entire 2008-2012 period.[4]
That the baseline reflects a long-term freeze is not because this is the amount states will need over this period to continue insuring the same number of low-income beneficiaries; rather, the baseline assumes a freeze because SCHIP is a mandatory program that has an annual funding cap and contains no automatic adjustment mechanism. In such cases, the budget baseline simply assumes that funding will remain frozen in perpetuity at the level set in law for the final year for which the program is currently authorized. In other words, under the baseline, the annual SCHIP funding level will still be $5.04 billion in all future fiscal years, from 2008 to 2050 and beyond.
Thus, the CBO baseline for SCHIP — unlike the baseline for Medicaid — fails to reflect the effects of the increases that CBO projects will occur in health care costs in the years ahead. As a result, the baseline falls well short of the cost of maintaining SCHIP at its current level of operation, with the gap between the baseline and the cost of maintaining SCHIP’s services growing wider with each passing year.
This analysis finds that if SCHIP is reauthorized but funding is frozen over the 2008-2012 period:[5]
-
in 2008, some 20 states will face a combined shortfall of $1.5 billion,[7] equivalent to the average annual cost of insuring up to 940,000 low-income children; and
In SCHIP’s early years, when many states’ SCHIP programs were just getting started, states that could use more than their full annual SCHIP allotment were able to draw on unspent funds from other states. Now, however, most states have mature SCHIP programs and fully spend their annual allotments over the three-year period for which such funds are available (see Figure 2). In addition, states’ total spending has exceeded the annual federal SCHIP grant since fiscal year 2002 (see Figure 3). As a result, the amount of unspent funds is shrinking rapidly. Over the next few years, the amount of unspent funds available for redistribution to other states will be much too small to make up for the funding shortfalls that would result from freezing annual SCHIP funding.[10]
States facing inadequate federal SCHIP funds will either have to increase their own state funding to make up for the shortfalls (which, in turn, will generally force them to raise taxes or cut other programs) or cut back their SCHIP programs by reducing eligibility, capping enrollment, eliminating benefits, increasing beneficiary cost-sharing, or cutting provider payments. In states that cut back their programs, substantial numbers of low-income children could lose health coverage.[11]
Improved SCHIP Financing System Cannot Eliminate Shortfall if Federal Funding Is Frozen
As Congress prepares for SCHIP reauthorization next year, some policymakers may assume that changes to make the distribution of SCHIP funds among states more efficient can, by themselves, address the looming funding shortfalls. Proposals may be offered to modify some of the more arcane aspects of the program’s financing structure, such as the formula used to determine each state’s share of the annual federal SCHIP allotment, the number of years that states are permitted to retain their SCHIP funds, and the method of redistributing unspent funds from states that have not used them to states that need additional funds.
For example, states currently have three years to spend their annual SCHIP allotments. As one component of the SCHIP reauthorization proposal in its fiscal year 2008 budget, the Administration has proposed to reduce from three years to one year the period of availability of annual SCHIP allotments and to target such funds to shortfall states.[12] Yet, while such an accelerated redistribution process deserves serious consideration on its own merits, by itself it would close only a modest fraction of the shortfalls: it would eliminate the shortfalls in fiscal year 2008 but do little or nothing to eliminate the shortfalls in years after that.
-
The shortfall in 2008 is projected to be $1.5 billion. Redistributing funds after one year, rather than three, would fully close the shortfall in 2008 but still leave a shortfall in 2009 of between $550 million and $615 million.
-
Moreover, for the five-year period from 2008 through 2012, the shortfall would still be $10.5 billion to $11.9 billion.[13] (The low end of the range in these estimates reflects the assumption of relatively low health-care cost growth of 5 percent per year, while the high end of the range reflects an assumption of moderate cost growth of 7.5 percent per year; see Appendix I for more details.) Although this proposal would lower the shortfall in the first year, it would actually widen the shortfalls that states experience in later years. This would occur because most of the funds that would be moved forward into 2008 under this approach would be funds that states otherwise would use in subsequent years. Moving the funds forward would narrow the gap initially but enlarge it after that.
Other changes that might be made in SCHIP reauthorization legislation to improve the targeting of SCHIP funds also could not compensate for more than a modest portion of the funding shortfalls. Even if all federal SCHIP funds could somehow be perfectly targeted to states. so not a single state would be left with a dollar in unspent funds at the end of 2012 (which, as explained below, is impossible to do), states would still face a shortfall of $10.4 billion to $11.7 billion over the 2008-2012 period. In other words, even if “perfect” targeting of funds among the states could somehow be achieved, that would close only one-seventh to one-eighth of the shortfall over the next five years.
These results reflect three basic realities. First, the amount of unspent funds available for redistribution will shrink over the next few years, as rising health-care costs cause states that are now leaving some funds unspent to spend more of their SCHIP allotments simply to continue covering the same number of beneficiaries. Second, SCHIP’s block-grant structure makes it impossible to target funds perfectly among the states. Each state’s annual SCHIP allotment is based on a formula built into federal statute, not on the state’s precise funding needs;[14] under such a system, some states inevitably will have either too much funding or too little.[15] Third and most important, the fundamental factor driving the shortfalls is not some deep flaw in SCHIP’s financing structure; rather, it is health care cost inflation. With health care costs rising significantly throughout the U.S. health care system — in the private and public sectors alike — it costs more each year just to keep insuring the same number of SCHIP beneficiaries.
Funds Available for Redistribution Are Shrinking
As noted, any SCHIP funds remaining unspent after three years are redistributed to states that have spent their available funds and can use additional funds to cover more low-income beneficiaries.[16] Unfortunately, this redistribution system is now falling increasingly short of meeting states’ funding needs, because the amounts available for redistribution are shrinking. The amounts redistributed reached a peak of $1.6 billion when unspent funds from fiscal year 2002 were provided to states; the redistribution of those funds provided more than enough money to states that needed additional resources that year. By 2006, however, Congress had to appropriate $283 million in additional SCHIP funds to avert projected state shortfalls because the amount of unspent funds available for redistribution had contracted and was no longer sufficient to close the shortfalls by itself. Over the next few years, no more than a few hundred million dollars per year are expected to be available for redistribution (see Figure 4), which is far below the projected size of the annual shortfalls.[17]
In addition, even if Congress provided the full $12.3 billion to $13.4 billion in additional funds we estimate are needed to close the shortfalls for 2008-2012, and sought to target these funds exclusively to shortfall states, some states likely would still face shortfalls, since it would be virtually impossible to target all of the funds to precisely the right states at exactly the right times, with none of the funds sitting unused in other states.[18]
|
The Cost to the Federal Treasury of Averting SCHIP Caseload Declines Would Likely Be Smaller than the Size of the Shortfall
CBO’s estimate of the cost of legislation that would provide sufficient increases in federal SCHIP funding to fully avert the shortfalls is likely to be as much as one-third to one-half lower than the $12.3 billion to $13.4 billion shortfall estimate presented here. CBO’s estimate of the cost of such legislation will reflect the fact that in the absence of additional federal SCHIP funds, some states facing SCHIP shortfalls are likely to switch some of the beneficiaries now covered through SCHIP to the Medicaid program.
In states that have used their SCHIP funds to expand their Medicaid programs, this would occur automatically. In states that have used their SCHIP funds to establish a separate state child health insurance program, the state could modify its Medicaid program so the program covered some of the beneficiaries previously covered by SCHIP, although states would not have to do so. Since the federal matching rate (i.e., the percentage of program costs that the federal government covers) is, on average, lower in Medicaid (57 percent) than in SCHIP (70 percent), many states likely would be unable or unwilling to expand Medicaid to cover these beneficiaries.
CBO assumes that if faced with SCHIP shortfalls, some states would move some SCHIP beneficiaries into Medicaid despite the lower federal matching rate (and the higher state costs) under the Medicaid program. CBO consequently assumes that federal Medicaid spending will increase if SCHIP shortfalls are not closed, and that averting SCHIP shortfalls will result in lower federal Medicaid costs than if the shortfalls are not addressed. In the past, when estimating the cost of SCHIP legislation, CBO has estimated this “Medicaid offset” at about one-third to one-half of SCHIP costs. (Similarly, the Congressional Research Service has estimated that about one-third of any SCHIP funding shortfalls would be offset by increases in Medicaid expenditures.) As a result, while CBO has not yet issued publicly an estimate of the cost of closing the SCHIP shortfalls, such an estimate could be in the range of $6.2 billion to $8.9 billion. ($6.2 billion is half of $12.3 billion, the low end of our estimate of the SCHIP shortfalls; $8.9 billion is two-thirds of $13.4 billion, the high end of our estimate of the shortfalls.) |
As a result, to ensure that federal SCHIP funding is adequate to avert shortfalls in all states, the overall SCHIP funding levels would have to be set somewhat higher than the levels that appear, on paper, to be required to close the shortfalls. (It should be noted that while the increase in federal SCHIP funding that would be needed to avert shortfalls is somewhat larger than the shortfall’s estimated size, the actual cost to the U.S. Treasury of providing the funds needed to close the shortfall would be significantly less than the size of the shortfall. For an explanation of why the cost to the Treasury would be lower, see the box on this page.)
Funding Shortfall Could Threaten Coverage for Several Million Low-Income Children
Congress established SCHIP in 1997 on the shoulders of Medicaid to reduce the number of uninsured low-income children. Nearly a decade later, more than 4 million low-income children — most of whom would otherwise be uninsured — receive comprehensive health insurance coverage through SCHIP-funded programs.
These SCHIP expansions, along with more effective Medicaid outreach efforts and actions to simplify the Medicaid enrollment process, have significantly improved children’s access to health coverage. While the percentage of low-income non-elderly adults without insurance increased from 1997 to 2005, the percentage of low-income children without insurance declined significantly — from 24.6 percent of low-income children to 18.7 percent. Medicaid and SCHIP were entirely responsible for this progress. Employer-based coverage for children eroded over this period.[19]
Now, however, the looming SCHIP shortfalls could cause large numbers of low-income children to lose health coverage. As noted earlier, if federal funding for 2008-2012 is frozen at its 2007 level, a $1.5 billion shortfall is projected for 2008. That represents the estimated average annual cost of providing SCHIP coverage for up to 940,000 children in 2008. In addition, the $3.3 billion to $3.9 billion shortfall projected for 2012 represents the estimated average annual cost of providing SCHIP coverage to between 1.6 million and 1.9 million children that year (see Figure 5).[20]
Similarly, while the Office of the Actuary at the Centers for Medicare and Medicaid Services has not issued any estimates of the size of the funding shortfalls for 2008 to 2012 if SCHIP funding is frozen at the 2007 levels, the CMS actuaries have estimated this year that the number of children enrolled in the SCHIP program will fall sharply — from 4.4 million in 2006 to 3.1 million by 2012 — if SCHIP funding is frozen. This would represent a reduction in coverage of 1.3 million children (see Figure 6).[21]
In sum, if SCHIP reauthorization legislation fails to give states sufficient funds to maintain their SCHIP programs, let alone the additional SCHIP funding needed to cover more uninsured children, much of the progress that SCHIP has made in reducing the ranks of uninsured children in the United States will be lost.
Appendix I: Methodology for the SCHIP Financing Estimates
The Balanced Budget Act of 1997, which established SCHIP, set the program’s annual federal funding levels for a ten-year period (1998-2007), after which SCHIP would need to be reauthorized. (States can continue to spend any unspent SCHIP funds remaining available after 2007, but will not receive any further SCHIP funds after 2007 unless the program is reauthorized.) This CBPP analysis examines the consequences of an SCHIP reauthorization under which the annual federal allotment for fiscal years 2008-2012 will be the same as the fiscal year 2007 funding level of $5.04 billion. (The CBO baseline assumes that SCHIP will be reauthorized but that funding will remain frozen at the fiscal year 2007 level.) Each state’s annual federal allotment in 2008-2012 is assumed to be the same as its expected allotment for 2007.
The CBPP analysis also projects states’ future financing needs for SCHIP based on each state’s historical SCHIP expenditure growth. The differences in state expenditure-growth rates are expected to narrow over time and eventually to disappear. In the low-expenditure-growth version of the model, we assume that growth rates in state costs converge over time to a rate of 5 percent. In the moderate-expenditure-growth version of the model, growth rates in state costs are assumed to converge ultimately to a rate of 7.5 percent. The assumption of converging state expenditure growth rates over time was included in the model originally created by the Office of the Actuary at the Centers for Medicare and Medicaid Services, on which CBPP’s SCHIP financing model is based. This assumption also continues to be used by CMS in its current SCHIP financing projections. (CMS does not provide a range of estimates; its original model assumed a single long-term growth rate of 5 percent, the same rate as is used under the low-expenditure-growth version of the CBPP expenditure model. In comparison, CRS does not factor in states’ historical growth rates but assumes instead a uniform annual growth rate of between six and seven percent starting in 2008.)
Based on these assumptions, we examine the extent to which available federal SCHIP funds will meet states’ projected financing needs and estimate the additional federal SCHIP outlays required above the CBO baseline to enable states to sustain their existing programs, given some degree of health-care cost inflation and population growth. Because of the imperfect nature of allocation formulas in block-grant programs such as SCHIP — under which some SCHIP funding is not used, or not used promptly, by states to which the funding is allocated — SCHIP funding levels likely would have to be set somewhat higher to reach these outlay levels, even if Congress modified the SCHIP funding system to improve the targeting of SCHIP funds.
Two estimates of aggregate shortfalls over the 2008-2012 period are provided in this analysis. The first estimate, $12.3 billion to $13.4 billion, assumes that SCHIP reauthorization does not change the rules governing states’ use of available SCHIP funds, that states will continue to have three years in which to spend funds from any particular year’s SCHIP allotment, and that some funds from the SCHIP allotments for fiscal years 2010-2012 will remain unspent at the end of 2012. The second estimate — $10.4 billion to $11.7 billion in shortfalls — assumes that Congress improves the targeting of SCHIP funds during reauthorization and that 100 percent of the available funds are spent by the end of 2012. As explained in this report, the latter assumption is unrealistic given the financing inefficiencies and targeting issues inherent in a block-grant financing structure.
Under both sets of CBPP estimates, the lower figure reflects the assumption of an annual growth rate of 5 percent (i.e., “low expenditure growth”), while the higher estimate reflects the assumption of a moderate growth rate of 7.5 percent (i.e., “moderate expenditure growth”). |
|
|
|
KEY FINDINGS IN THIS REPORT:
 As a result of SCHIP, the number of uninsured low-income children has fallen significantly, but a substantial share of this progress will be undone if SCHIP funding is frozen (by being held to the SCHIP “budget baseline” level) when the program is reauthorized this year. As a result of SCHIP, the number of uninsured low-income children has fallen significantly, but a substantial share of this progress will be undone if SCHIP funding is frozen (by being held to the SCHIP “budget baseline” level) when the program is reauthorized this year.
 The baseline assumes that SCHIP funding will be frozen for the next ten years at the 2007 funding level of $5 billion, with no adjustment for rising health care costs or expected increases in the number of children due to normal population growth. The baseline assumes that SCHIP funding will be frozen for the next ten years at the 2007 funding level of $5 billion, with no adjustment for rising health care costs or expected increases in the number of children due to normal population growth.
 If SCHIP funding is frozen at its 2007 level when the program is reauthorized, states will face a shortfall of $12.3 billion to $13.4 billion for 2008-2012. If SCHIP funding is frozen at its 2007 level when the program is reauthorized, states will face a shortfall of $12.3 billion to $13.4 billion for 2008-2012.
 If SCHIP funding is frozen, 20 states will face a shortfall in 2008 equivalent to the average, annual cost of covering up to 940,000 children. In 2012, some 36 states will face a shortfall equivalent to the average, annual cost of covering up to 1.9 million children. If SCHIP funding is frozen, 20 states will face a shortfall in 2008 equivalent to the average, annual cost of covering up to 940,000 children. In 2012, some 36 states will face a shortfall equivalent to the average, annual cost of covering up to 1.9 million children.
|
|
|
|
|
|
Table 1: States Projected to Face Federal Funding Shortfalls in Select Years: 2008 and 2012
(assumes moderate expenditure growth and current rules for allocating and redistributing funds across states)
|
2008 |
2012 |
|
State |
Estimated Shortfall |
State |
Estimated Shortfall |
|
Alaska |
$18,037,000 |
Alabama |
$73,741,000 |
|
California |
$203,611,000 |
Alaska |
$27,969,000 |
|
Georgia |
$154,444,000 |
Arizona |
$36,981,000 |
|
Illinois |
$291,823,000 |
Arkansas |
$35,156,000 |
|
Iowa |
$30,779,000 |
California |
$778,379,000 |
|
Kansas |
$247,000 |
Georgia |
$271,454,000 |
|
Maine |
$11,438,000 |
Hawaii |
$12,593,000 |
|
Maryland |
$93,093,000 |
Illinois |
$474,552,000 |
|
Massachusetts |
$170,863,000 |
Iowa |
$55,837,000 |
|
Minnesota |
$42,797,000 |
Kansas |
$31,095,000 |
|
Mississippi |
$54,301,000 |
Kentucky |
$40,117,000 |
|
Missouri |
$42,097,000 |
Louisiana |
$53,476,000 |
|
Nebraska |
$12,865,000 |
Maine |
$20,294,000 |
|
New Jersey |
$214,102,000 |
Maryland |
$146,770,000 |
|
North Carolina |
$44,017,000 |
Massachusetts |
$282,675,000 |
|
North Dakota |
$1,000 |
Michigan |
$99,597,000 |
|
Ohio |
$8,108,000 |
Minnesota |
$73,277,000 |
|
Rhode Island |
$54,478,000 |
Mississippi |
$92,588,000 |
|
South Dakota |
$2,240,000 |
Missouri |
$79,994,000 |
|
Wisconsin |
$33,402,000 |
Montana |
$5,762,000 |
|
|
|
Nebraska |
$24,396,000 |
|
|
|
New Jersey |
$330,732,000 |
|
|
|
New Mexico |
$67,132,000 |
|
|
|
North Carolina |
$120,150,000 |
|
|
|
North Dakota |
$3,770,000 |
|
|
|
Ohio |
$123,022,000 |
|
|
|
Oklahoma |
$36,942,000 |
|
|
|
Oregon |
$55,794,000 |
|
|
|
Pennsylvania |
$92,694,000 |
|
|
|
Rhode Island |
$77,688,000 |
|
|
|
South Dakota |
$8,604,000 |
|
|
|
Texas |
$82,620,000 |
|
|
|
Virginia |
$66,319,000 |
|
|
|
West Virginia |
$26,158,000 |
|
|
|
Wisconsin |
$67,482,000 |
|
|
|
Wyoming |
$6,230,000 |
|
Total States:
20 |
Total Shortfall: $1,482,745,000 |
Total States:
36 |
Total Shortfall:
$3,882,040,000 |
* Center on Budget and Policy Priorities' moderate expenditure growth SCHIP financing model based on a model created by the Office of the Actuary at the Centers for Medicare and Medicaid Services. Under the low expenditure growth scenario, all states listed here except Arizona are projected to experience federal financing shortfalls in 2008, and all states listed here are projected to experience federal financing shortfalls in 2012.
|
Table 2: Projected Federal SCHIP Funds Available in States as a Percentage of States’ Projected Need for Such Funds
(assumes moderate expenditure growth and current rules for allocating and redistributing funds across states) |
| |
2008 |
2009 |
2010 |
2011 |
2012 |
| # States Under 100% |
20 |
23 |
30 |
34 |
36 |
| |
|
|
|
|
|
| Alabama |
|
66% |
59% |
55% |
51% |
| Alaska |
40% |
38% |
36% |
33% |
31% |
| Arizona |
|
|
|
94% |
78% |
| Arkansas |
|
|
|
78% |
59% |
| California |
83% |
63% |
59% |
55% |
51% |
| Georgia |
53% |
48% |
46% |
42% |
39% |
| Hawaii |
|
|
66% |
60% |
55% |
| Illinois |
43% |
40% |
38% |
35% |
32% |
| Iowa |
55% |
50% |
47% |
44% |
40% |
| Kansas |
100% |
68% |
63% |
59% |
55% |
| Kentucky |
|
|
|
72% |
64% |
| Louisiana |
|
|
83% |
68% |
63% |
| Maine |
58% |
54% |
51% |
47% |
44% |
| Maryland |
43% |
41% |
39% |
36% |
33% |
| Massachusetts |
32% |
28% |
27% |
25% |
22% |
| Michigan |
|
75% |
70% |
65% |
60% |
| Minnesota |
54% |
51% |
48% |
44% |
41% |
| Mississippi |
53% |
50% |
48% |
44% |
41% |
| Missouri |
64% |
60% |
56% |
52% |
48% |
| Montana |
|
|
|
|
75% |
| Nebraska |
63% |
60% |
56% |
52% |
46% |
| New Jersey |
35% |
32% |
31% |
28% |
26% |
| New Mexico |
|
|
77% |
48% |
45% |
| North Carolina |
77% |
66% |
62% |
58% |
54% |
| North Dakota |
100% |
83% |
78% |
73% |
68% |
| Ohio |
96% |
70% |
66% |
61% |
57% |
| Oklahoma |
|
|
97% |
71% |
66% |
| Oregon |
|
|
67% |
55% |
51% |
| Pennsylvania |
|
|
|
83% |
66% |
| Rhode Island |
23% |
22% |
21% |
19% |
17% |
| South Dakota |
84% |
68% |
64% |
60% |
55% |
| Texas |
|
|
|
|
91% |
| Virginia |
|
|
72% |
64% |
59% |
| West Virginia |
|
83% |
60% |
56% |
52% |
| Wisconsin |
68% |
64% |
60% |
56% |
51% |
| Wyoming |
|
|
86% |
58% |
53% |
Source: Center on Budget and Policy Priorities' moderate expenditure growth SCHIP financing model
|
End Notes:
[1] The most recent data available for the number of children enrolled in SCHIP at any given point in time indicate that more than 4 million children were enrolled in June 2005. The Department of Health and Human Services reports that the number of children enrolled at any point over the course of a year stood at 6.6 million in fiscal year 2006.
[2] For a discussion of SCHIP’s financing structure, see Matt Broaddus, “Administration’s Fiscal Year 2007 Budget Is Still Likely to Leave SCHIP Coverage for Low-Income Children in Jeopardy,” Center on Budget and Policy Priorities, Revised March 22, 2006. For the most recent analysis of projected fiscal year 2007 SCHIP federal financing shortfalls, see Matt Broaddus and Edwin Park, “Congress Delayed SCHIP Funding Shortfalls in 2007 by Several Months but Must Act to Avert Remaining Shortfalls,” Revised February 22, 2007.
[3] See Broaddus and Park, op cit.
[4] See for example, Congressional Budget Office, “Fact Sheet for CBO’s March 2006 Baseline: Medicaid and the State Children’s Health Insurance Program,” March 2006.
[5] All estimates are from the Center on Budget and Policy Priorities’ SCHIP financing model, which is based on a SCHIP financing model developed by the Office of the Actuary at the Centers for Medicare and Medicaid Services. This model was used to assess the adequacy of federal SCHIP funding among the states if SCHIP is reauthorized at the fiscal year 2007 level of $5.04 billion for the five years from 2008 to 2012. See Appendix I for a discussion of the expenditure growth assumptions used in estimating the shortfalls for these years. The shortfall estimates do not assume any changes to current rules regarding how SCHIP funds are allocated among states, how long states have such funds available to spend, or how unspent funds are redistributed to other states.
[6] Chris Peterson, “SCHIP Financing: Funding Projections and State Redistribution Issues,” Congressional Research Service, Updated January 30, 2007. In comparison to CBPP, which uses state-specific historical growth rates that eventually converge to an annual growth rate of 5 percent for its low expenditure growth estimate and an annual growth rate of 7.5 percent for its moderate expenditure growth estimate, as described in Appendix I, CRS uses (starting in 2008) projected annual growth in national per capita health care spending, which varies between 6 percent and 7 percent.
[7] CRS also projects that 20 states will face a shortfall of $1.5 billion in fiscal year 2008. See Peterson, op cit.
[8] CRS projects that 35 states will face a shortfall of $3.3 billion in fiscal year 2012. See Peterson, op cit.
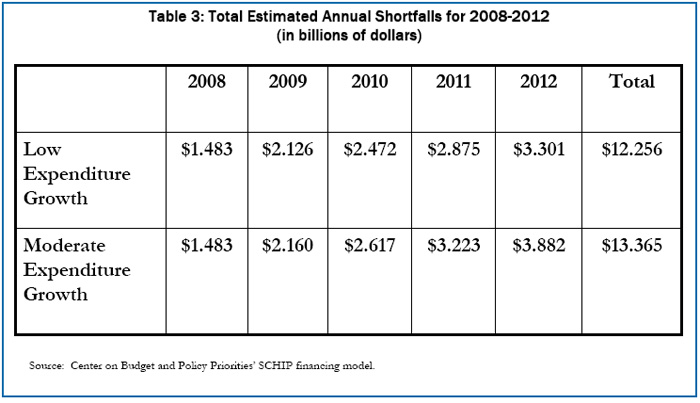
[9] For the list of states estimated to have federal funding shortfalls and an estimate of the projected shortfalls in those states for fiscal years 2008 and 2012, see Table 1. For calculations of the available funds in shortfall states as a percentage of the funds that these states are projected to need to sustain their existing programs for years from 2008-2012, see Table 2. For a year-by-year estimate of the aggregate funding shortfalls for the 2008-2012 period, see Table 3.
[10] Other factors adding to the federal funding shortfall include the “SCHIP dip” (a 26-percent reduction in federal SCHIP funding for fiscal years 2002-2004) and the expiration of $1.4 billion in unspent SCHIP funds from the early years of the program. (The funds reverted to the federal Treasury at the end of fiscal years 2004 and 2005 after Congress declined to extend their availability.)
[11] In the modest number of states facing shortfalls that have also expanded SCHIP coverage to parents, pregnant women and/or childless adults, adults also would be at risk of losing their SCHIP coverage. In the shortfall states whose SCHIP programs cover parents of low-income children enrolled in Medicaid and SCHIP, the loss of such coverage would likely adversely affect children’s coverage. An extensive body of research literature shows that covering low-income parents increases enrollment in public programs among eligible children. Scaled-back SCHIP coverage of parents therefore would likely result in reduced coverage for low-income children as well and in more children becoming uninsured. See Leighton Ku and Matthew Broaddus, “Coverage of Parents Helps Children Too,” Center on Budget and Policy Priorities, October 20, 2006.
[12] For an in-depth analysis of the budget proposal, see Edwin Park and Matt Broaddus, “SCHIP Reauthorization: President’s Budget Would Provide Less Than Half the Funds States Need to Maintain Enrollment,” Center on Budget and Policy Priorities, February 22, 2007.
[13] These estimates assume that the accelerated redistribution first takes effect in fiscal year 2008: in 2008, any unspent SCHIP funds originally allocated for fiscal year 2007 that remain unspent after 2007 would be redistributed and targeted to shortfall states in 2008, along with the regularly scheduled redistribution of remaining unspent fiscal year 2005 funds.
[14] Under the current system, each state’s share of the annual federal SCHIP allotment is based on a formula that accounts for: the state’s share of the national population of children in families with income under 200 percent of the poverty line, the state’s share of the national population of uninsured children in these families, and the state’s wages for medical professionals relative to such wages across the nation. Legislation enacted in 1999 limited the year-by-year variation in a state’s share of the allotment that would otherwise result under the formula.
[15] Only a program like Medicaid that covers a specified percentage of a state’s annual costs, without a cap on the federal funding level — i.e., only a program funded on an open-ended entitlement basis — can promptly meet states’ changing needs and target federal funds precisely to reflect those needs.
[16] The original SCHIP statute did not set forth the rules for redistributing unspent funds, but Congress subsequently enacted legislation setting rules for redistributing unspent funds from fiscal years 1998 through 2001. The statute remained silent on the rules for redistributing unspent funds from fiscal years after that. The Administration has used its discretion to target the unspent SCHIP funds from these fiscal years to states that faced immediate shortfalls. The modeling reflected in this analysis assumes that in the future, any SCHIP funds remaining unspent after three years will continue to be redistributed to shortfall states in the manner that the Administration has employed in the past few years.
[17] The estimates of annual shortfalls incorporate the effects of future anticipated redistributions of unspent SCHIP funds.
[18] Because of SCHIP’s block-grant financing structure, merely increasing annual allotments to states for 2008-2012 by $13.4 billion above the baseline levels would reduce the total estimated shortfall by something less than $13.4 billion and would not fully close the shortfall, since the targeting of the added funds would not be “perfect.” As a result, a desirable targeting approach would be to appropriate the necessary funding and to place this funding in a special redistribution pool targeted exclusively to shortfall states. Even such an approach could not ensure perfect targeting, however, due to timing issues and inevitable differences between the amount of funds projected to be needed in each state when the funds are distributed and the actual amounts that states turn out to need. Increases in health care costs are notoriously difficult to predict with precision.
[19] Based on a CBPP analysis of the 1998 and 2006 Annual Social and Economic Characteristics supplements to the Current Population Survey administered by the Census Bureau.
[20] These estimates of children whose SCHIP coverage would be at risk if funding is frozen are based on SCHIP per capita expenditure estimates for children, as derived from Medicaid per capita figures for children from CBO’s March 2006 Medicaid baseline. As noted, in the states facing shortfalls that have expanded SCHIP coverage both for children and for certain adult populations (including parents, pregnant women, and/or childless adults), those adults also would be at risk of losing their health insurance and becoming uninsured.
In addition, as noted in the box on page 7, instead of reducing SCHIP enrollment, states could choose to address part of the shortfalls by expanding their Medicaid programs to cover some of their current SCHIP beneficiaries (albeit at a higher state cost). States also could elect to address these shortfalls by scaling back benefits, increasing beneficiary cost-sharing, or reducing provider payments. As a result, the actual number of children currently enrolled in SCHIP who would lose health care coverage entirely due to the shortfalls would likely be less than the estimates noted above of the number of children who would be at risk due to the shortfalls.
[21] Office of the Actuary at the Centers for Medicare and Medicaid Services, February 2007. The CMS estimates do not include children who may be shifted from SCHIP to Medicaid by their states in response to SCHIP funding shortfalls. |
|

