RELEASE
__________

|
FOR IMMEDIATE RELEASE: Tuesday, May 31, 2005 |
CONTACT: Michelle Bazie (202) 408-1080 |
Suite 510
Washington, DC 20002
Tel: 202-408-1080
Fax: 202-408-1056
[email protected]
www.cbpp.org
Robert Greenstein
Executive Director
Iris J. Lav
Deputy Director
Board of Directors
David de Ferranti, Chair
The World Bank
John R. Kramer, Vice Chair
Tulane Law School
Henry J. Aaron
Brookings Institution
Ken Apfel
University of Texas
Barbara B. Blum
Columbia University
Marian Wright Edelman
Children’s Defense Fund
James O. Gibson
Center for the Study of Social Policy
Beatrix Hamburg, M.D.
Cornell Medical College
Frank Mankiewicz
Hill and Knowlton
Richard P. Nathan
Nelson A Rockefeller
Institute of Government
Marion Pines
Johns Hopkins University
Sol Price
Chairman, The Price Company (Retired)
Robert D. Reischauer
Urban Institute
Audrey Rowe
AR Consulting
Susan Sechler
German Marshall Fund
Juan Sepulveda, Jr.
The Common Experience/
San Antonio
William Julius Wilson
Harvard University
NEW STUDY FINDS POOR MEDICAID BENEFICIARIES
FACE
GROWING OUT-OF-POCKET MEDICAL COSTS
Increased Cost-Sharing Could Mean Less Care,
Poorer Health for Vulnerable Families
|
Press Release: HTM
| PDF Related Reports: Out-of-Pocket Medical Expenses for Medicaid Beneficiaries Are Substantial and Growing The Effect of Increased Cost Sharing in Medicaid: A Summary of Research Findings Robert Greenstein Comments on the National Governors Association's Medicaid Recommendations |
| If you cannot access the files through the links, right-click on the underlined text, click "Save Link As," download to your directory, and open the document in Adobe Acrobat Reader. |
A new Center report finds that out-of-pocket medical expenses for poor adult Medicaid beneficiaries have grown twice as fast as their incomes in recent years. These individuals spend more than three times as much of their income on health care as middle-class adults with private insurance, the study finds.
“Some supporters of increased cost-sharing claim low-income Medicaid beneficiaries pay little or nothing and bear little financial responsibility for their health care,” noted Leighton Ku, the report’s lead author. “That is not accurate. Out-of-pocket medical costs take a bigger bite out of the wallets of Medicaid beneficiaries than of people at higher income levels who are privately insured.”
These findings are significant because increased cost-sharing, or requiring Medicaid beneficiaries to pay more for medical care, is being considered as a way to reduce Medicaid costs. Congress, the National Governors Association, and a recently announced Medicaid Commission being formed by the Bush Administration are separately discussing cost-cutting measures for the program.
Burdens Much Heavier for Medicaid Beneficiaries than Privately Insured
The Center’s report is based on data from the Medical Expenditure Panel Surveys, a series of nationally representative surveys conducted by the Department of Health and Human Services. It finds that:
-
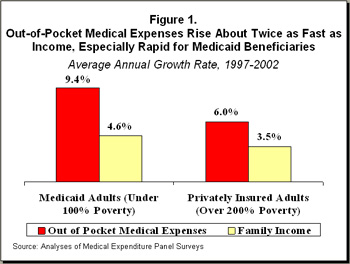
Out-of-pocket medical expenses for poor adult Medicaid beneficiaries who are not elderly or disabled grew an average of 9.4 percent annually between 1997 and 2002, twice as fast as their incomes grew during that period (4.6 percent annually). Expenses rose more slowly for middle-class privately insured adults: 6 percent per year.
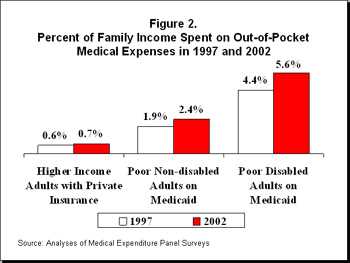
- In 2002, poor adult Medicaid beneficiaries spent more than three times as large a percentage of their income on out-of-pocket medical expenses as middle-class adults with private insurance; disabled Medicaid beneficiaries spent eight times as large a percentage as adults with private insurance.
- Average out-of-pocket prescription drug expenses nearly doubled between 1997 and 2002 for Medicaid beneficiaries who are not elderly or disabled. For Medicaid beneficiaries with disabilities, they more than doubled.
Higher Cost-Sharing Causes Cutbacks in Essential Care
Increasing cost-sharing, such as through higher copayments or premiums or the elimination of certain benefits (such as dental or vision coverage), has been suggested as a way to reduce Medicaid costs and promote “personal responsibility.” As a second new Center report shows, however, a substantial body of research finds that increased copayments cause low-income beneficiaries to cut back on essential care, and higher premiums lead to fewer people being covered by health insurance.
Increasing cost-sharing also can trigger the subsequent use of more expensive forms of care, such as emergency room care or hospitalization, as beneficiaries’ failure to receive needed treatment contributes to more serious health problems.
The risks of increased cost-sharing are greatest for those with serious or chronic health conditions, such as diabetes, cancer, or mental illness, since they need the most health care services and thus would face more copayment charges or the loss of more services. Moreover, the consequences of going without a needed service can be especially severe for individuals who are in poor health.
“The research indicates that significantly raising the amount that Medicaid beneficiaries must pay out of pocket would cause many low-income individuals to go without needed doctor’s visits or prescription drugs, often leading to serious health problems,” Ku said. “Governors have asked the federal government not to shift Medicaid costs on to the states. Both state and federal officials should consider whether it is appropriate to shift those costs on to the poor.”
The following two reports are available on the Center’s website.
# # # #
The Center on Budget and Policy Priorities is a nonprofit, nonpartisan research organization and policy institute that conducts research and analysis on a range of government policies and programs. It is supported primarily by foundation grants.