WIC Works: Addressing the Nutrition and Health Needs of Low-Income Families for More Than Four Decades
End Notes
[1] Steven Carlson is a research analyst who previously directed the Office of Policy Support at the Agriculture Department’s Food and Nutrition Service. The opinions and conclusions expressed in this report are solely those of the authors and should not be construed as representing the views of the Agriculture Department.
[2] For more information on how WIC operates, see Policy Basics: Special Supplemental Nutrition Program for Women, Infants, and Children, Center on Budget and Policy Priorities, updated April 26, 2017, https://www.cbpp.org/cms/index.cfm?fa=view&id=5268.
[3] Fox MK, Hamilton W, Lin BH, eds., (2004). Effects of Food Assistance and Nutrition Programs on Nutrition and Health: Volume 3, Literature Review. Food Assistance and Nutrition Research Report No. 19-3, U.S. Department of Agriculture, Economic Research Service, https://www.ers.usda.gov/webdocs/publications/fanrr193/30219_fanrr19-3fm_002.pdf; Colman S, Nichols-Barrer IP, Redline JE, Devane BL, Ansell SV, and Joyce T (2012). Effects of the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC): A Review of Recent Research. Report WIC-12-WM. U.S. Department of Agriculture, Food and Nutrition Service, https://www.fns.usda.gov/effects-special-supplemental-nutrition-program-women-infants-and-children-wic-review-recent-research.
[4] See, for example, Brooks-Gunn J, Duncan G (1997). The effects of poverty on children. The Future of Children 7(2). For a comprehensive review of more recent evidence that children growing up in poor families fare worse than children in more affluent families, see Duncan G, Le Menestrel, eds., (2019). A Roadmap to Reducing Child Poverty. Washington, DC: The National Academies Press.
[5] Cook JT, Frank DA (2008). Food security, poverty, and human development in the United States. Annals of the New York Academy of Sciences, 1136(1):193-209. Food insecurity is defined as lack of access to a safe and secure source of enough food to sustain an active, healthy life.
[6] Halfon N et al (2020). Measuring equity from the start: disparities in the health development of US kindergartners. Health Affairs, 39(10): 1702-1709.
[7] Currie J, RossinSlater M (2015). Earlylife origins of lifecycle wellbeing: research and policy implications. Journal of Policy Analysis and Management, 34(1):208242; Center on the Developing Child at Harvard University (2016). From Best Practices to Breakthrough Impacts, https://developingchild.harvard.edu/wp-content/uploads/2016/05/From_Best_Practices_to_Breakthrough_Impacts-4.pdf, accessed on August 8, 2020; and Duncan and Le Menestrel (2019), op cit.
[8] Center on the Developing Child at Harvard University (2010). The foundations of lifelong health are built in early childhood, http://www.developingchild.harvard.edu/, accessed on December 5, 2014.
[9] Duncan GJ, Magnuson K, Kalil A, Ziol-Guest K (2012). The importance of early childhood poverty. Social Indicators Research 108:87-98.
[10] Ratcliffe C, McKernan SM (2012). Child Poverty and Its Lasting Consequence. Low-Income Families Working Paper 21, Washington, DC: The Urban Institute, http://www.urban.org/research/publication/child-poverty-and-its-lasting-consequence.
[11] Nelson BB et al. (2016). Predictors of poor school readiness in children without developmental delay at age 2. Pediatrics, 138(2), http://pediatrics.aappublications.org/content/pediatrics/138/2/e20154477.full.pdf.
[12] Duncan GJ, Magnuson K, Votruba-Drzal E (2017). Moving beyond correlations in assessing the consequences of poverty. Annual Review of Psychology, 68:413-434.
[13] Duncan GJ, Ziol-Guest K, Kalil A (2010). Early-childhood poverty and adult attainment, behavior, and health. Child Development, 81(1):306-325. The authors estimate that a $10,000 annual increase in low-income families’ income before a child’s fifth birthday is associated with a 68 percent increase in adult earnings and more than 500 additional work hours per year after age 25.
[14] Blair C, Raver C (2016). Poverty, stress, and brain development: New directions for prevention and intervention. Academic Pediatrics, 16(3), S30-S36.
[15] Shonkoff J, Garner A, Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, and Section on Developmental and Behavioral Pediatrics (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129(1):e232-246.
[16] Early life experiences may also affect nutrition behavior later in life. A recent systematic review identified a 46 percent increase in the odds of adult obesity following exposure to multiple adverse events in childhood. See Wiss DA, Brewerton TD (2020). Adverse childhood experiences and adult obesity: a systematic review of plausible mechanisms and meta-analysis of cross-sectional studies. Physiology & Behavior, 223(1):112964. A study of adults in Nevada suggests that fruit and vegetable consumption in adulthood may also be associated with the cumulative effects of multiple adverse childhood experiences. See Horino M, Yang W (2020). Impact of adverse childhood experiences and fruit and vegetable intake in adulthood. Public Health Nutrition, published online April 22.
[17] Cameron AJ, Spence AC, Laws R, Hesketh KD, Lioret S, Campbell K J (2015). A review of the relationship between socioeconomic position and the early-life predictors of obesity. Current Obesity Reports, 4(3):350-362.
[18] Wen X, Kong KL, Eiden RD, Sharma NN, Xie C (2014). Sociodemographic differences and infant dietary patterns. Pediatrics, 134(5):e1387-1398, https://www.researchgate.net/profile/Kai_Ling_Kong2/publication/266948125_Sociodemographic_Differences_and_Infant_Dietary_Patterns/links/55312b5c0cf27acb0dea690f.pdf.
[19] Grummer-Strawn LM, Li R, Perrine CG, Scanlon KS, Fein SB (2014). Infant feeding and long-term outcomes: results from the year 6 follow-up of children in the Infant Feeding Practices Study II. Pediatrics, 134 (Supplement 1):S1-S3.
[20] Devaney B (1992). Very Low Birthweight among Medicaid Newborns in Five States: The Effects of Prenatal WIC Participation. Alexandria, Virginia: Food and Nutrition Service, USDA; Devaney B, Bilheimer L, Schore J (1990). The Savings in Medicaid Costs for Newborns and Their Mothers from Prenatal WIC Participation in the WIC Program, Volume 1. Alexandria, VA: Food and Nutrition Service, USDA; Devaney B, Bilheimer L, Schore J (1991). The Savings in Medicaid Costs for Newborns and Their Mothers from Prenatal WIC Participation in the WIC Program, Volume 2. Alexandria, VA: Food and Nutrition Service, USDA; Devaney B, Schirm A (1993). Infant Mortality among Medicaid Newborns in Five States: The Effects of Prenatal WIC Participation. Alexandria, VA: Food and Nutrition Service, USDA. In light of the significant changes in the WIC and Medicaid participation and policy environments, USDA launched a second WIC-Medicaid Study in 2010. The study’s goal was to use linked administrative data from WIC, Medicaid, and vital records in two states (Missouri and Oklahoma) to assess the feasibility of examining the association between WIC participation during pregnancy and early childhood and birth outcomes and health care utilization and costs. While the project demonstrated the feasibility of this approach to analyze WIC’s impact on an expanded set of pregnancy and birth outcomes, the absence of cost data for the growing number of Medicaid recipients in managed care programs presented an unsurmountable challenge to measuring the association between WIC and Medicaid costs. See Kranker K, Fox MK, Caronongan P (2018). WIC−Medicaid II Feasibility Study: Final Report, Alexandria, VA: Food and Nutrition Service, USDA.
[21] This review, sponsored by USDA’s Economic Research Service, points out that “the consistency of the results across studies is noteworthy. This is especially true when . . . the bulk of the literature is comprised of relatively large, well-conducted studies, [and] includes both national samples and state-level data . . . from a number of different time periods” (Fox Hamilton and Lin (2004) op. cit.).
[22] Colman et al., op. cit.
[23] Hamad R, Collin DF, Bae, RJ, Jelliffe-Pawlowski LL (2019). Association of revised WIC food package with perinatal and birth outcomes: a quasi-experimental study. JAMA Pediatrics, 173(9): 845-852.
[24] Blakeney EL, Herting JR, Zierler BK, Bekemeier B (2020). The effect of women, infant, and children (WIC) services on birth weight before and during the 2007–2009 great recession in Washington state and Florida: a pooled cross-sectional time series analysis. BMC Pregnancy and Childbirth, 20: 1-13.
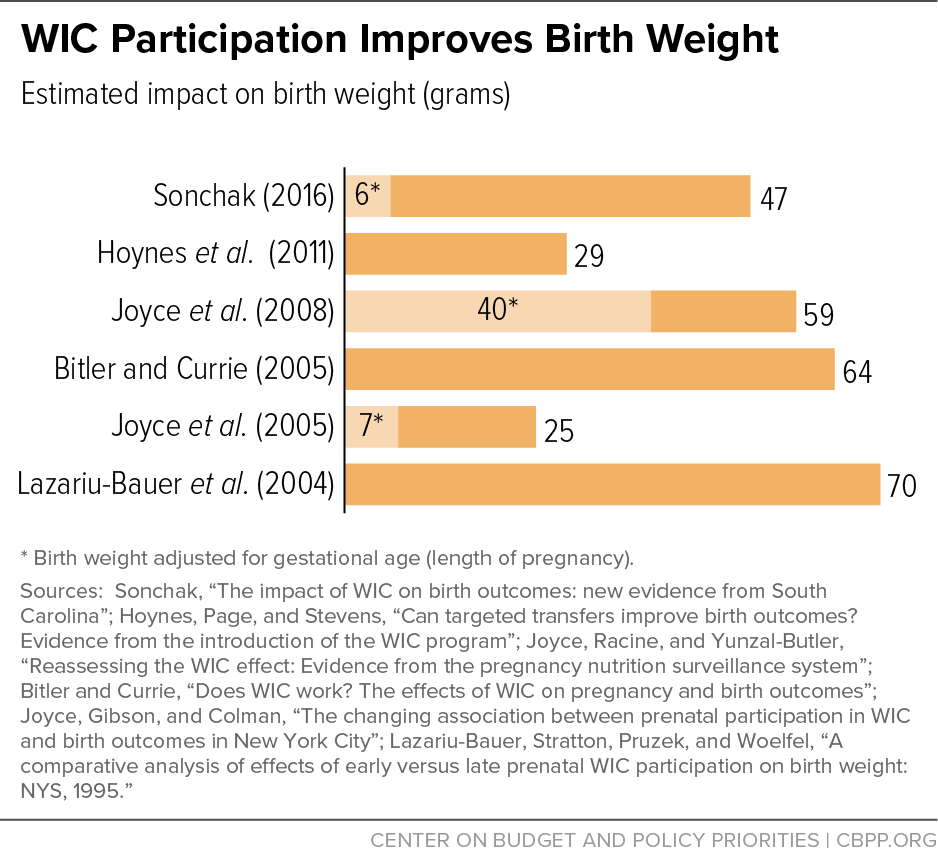
[25] See, for example, Lazariu-Bauer V, Stratton H, Pruzek R, Woelfel ML (2004). A comparative analysis of effects of early versus late prenatal WIC participation on birth weight: NYS, 1995. Maternal and Child Health Journal, 8(2):77-86; Bitler MP, Currie J (2005).
Does WIC work? The effects of WIC on pregnancy and birth outcomes. Journal of Policy Analysis and Management, 24(1):73-91; Joyce T, Gibson D, Colman S (2005). The changing association between prenatal participation in WIC and birth outcomes in New York City. Journal of Policy Analysis and Management, 24(4):661-685; Joyce T, Racine A, Yunzal-Butler C (2008). Reassessing the WIC effect: evidence from the pregnancy nutrition surveillance system. Journal of Policy Analysis and Management, 27(2):277-303; Hoynes HW, Page ME, Stevens AH (2011). Can targeted transfers improve birth outcomes? Evidence from the introduction of the WIC program. Journal of Public Economics, 95(7):813-827; and Rossin-Slater M (2013). WIC in your neighborhood: new evidence on the impacts of geographic access to clinics. Journal of Public Economics, 102:51-69.
[26] These increases are likely to be clinically relevant. “Small WIC impacts on birth outcomes may be sufficient for program benefits to exceed costs, given the relatively modest program costs per pregnant mother and the substantial medical and other social savings associated with averting even a small number of poor birth outcomes” (Ludwig J Miller M (2005). Interpreting the WIC debate. Journal of Policy Analysis and Management 24(4):691-701.)
[27] Bitler and Currie (2005), op. cit.
[28] Joyce et al. (2008), op. cit.; Currie J, Rajani I (2014). Within-mother estimates of the effects of WIC on birth outcomes in New York City. Working Paper 20400, Cambridge, MA: National Bureau of Economic Research; Sonchak L (2016). The impact of WIC on birth outcomes: new evidence from South Carolina. Maternal and Child Health Journal, 20(7):15181525; and Chorniy A, Currie J, Sonchak L (2020). Does prenatal WIC participation improve child outcomes? American Journal of Health Economics, 6(2): 169-198. In addition, the last reference cited here suggests that WIC may have larger effects on more disadvantaged mothers who are at higher risk of adverse birth outcomes. The WIC-Medicaid II Feasibility Study found no evidence of WIC’s impact on birthweight in Missouri or Oklahoma (Kranker, Fox, and Caronongan (2018) op. cit.).
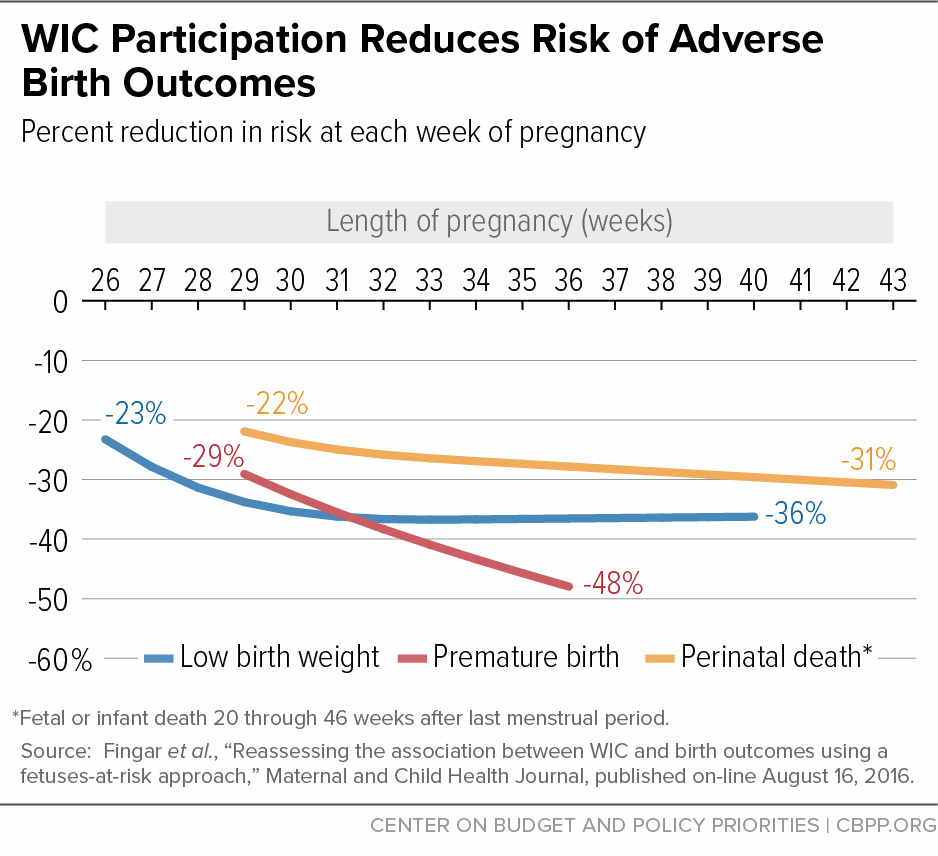
[29] Fingar KR, Lob SH, Dove MS, Gradziel P, Curtis MP (2016). Reassessing the association between WIC and birth outcomes using a fetusesatrisk approach. Maternal and Child Health Journal, 21(4), 825-835.
[30] Kranker, Fox, and Caronongan (2018) op. cit. These researchers note that the estimated reductions in the probability of preterm birth obtained from their approach (using discrete time hazard models) are smaller than those estimated in previous research that did not adjust for gestational-age bias. They suggest that the difference in average gestational lengths between WIC participants and non-participants is, to a large extent, driven by gestational-age bias (not impacts of WIC on gestational age).
[31] There is also some limited evidence that WIC participation may be associated with reductions in the risk of pregnancies that end with a stillbirth among non-Hispanic Black women. See Angley M et al. (2018). Association of participation in a supplemental nutrition program with stillbirth by race, ethnicity, and maternal characteristics. BMC Pregnancy and Childbirth, 18(1): 306.
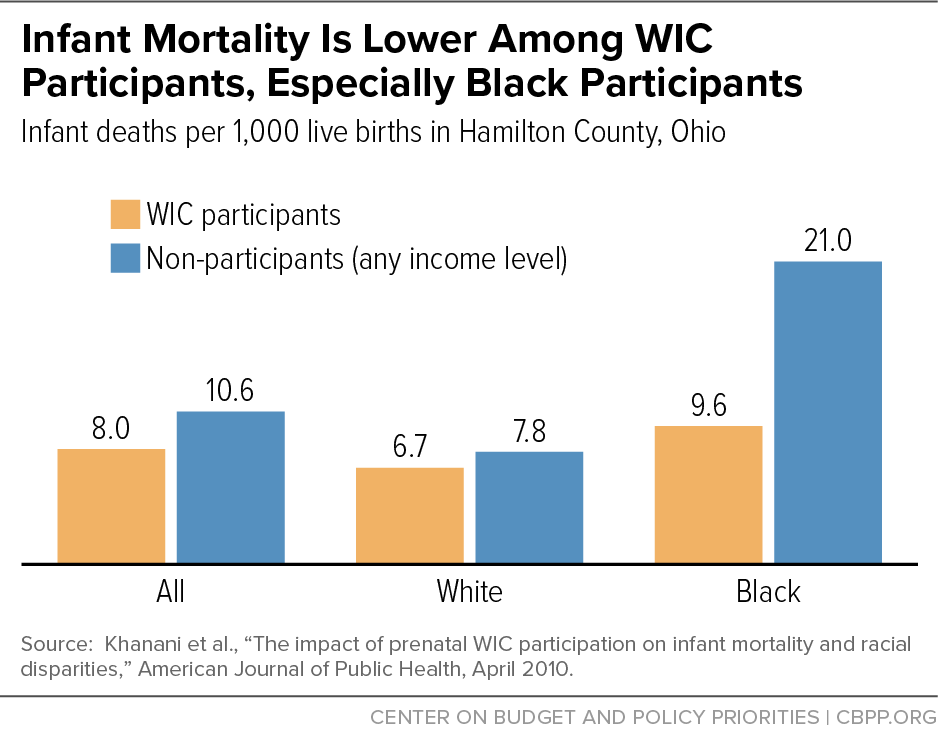
[32] See, for example, the summary in Table 18 of USDA, Economic Research Service (2004). More recently, however, the WIC-Medicaid II feasibility study found no impact of WIC on infant mortality in Missouri and Oklahoma (Kranker, Fox and Caronongan (2018) op. cit.).
[33] Soneji S, Beltrán-Sánchez H (2019). Association of Special Supplemental Nutrition Program for Women, Infants, and Children with preterm birth and infant mortality. JAMA Network Open, 2(12): e1916722-e1916722.
[34] Khanani I, Elam J, Hearn R, Jones C, Maseru N (2010). The impact of prenatal WIC participation on infant mortality and racial disparities. American Journal of Public Health, 100(Supplement 1):S204-S209.
[35] Keene-Woods N, Reyes J, Chesser A (2016). Infant mortality and race in Kansas: associations with women, infants, and children services. Journal of Primary Care and Community Health, 7(3):194198, http://journals.sagepub.com/doi/pdf/10.1177/2150131916635572.
[36] Li R, Dee D, Li CM, Hoffman HJ, Grummer-Strawn LM (2014). Breastfeeding is associated with reduced risk of infections at age 6 years. Pediatrics, 134(Supplement 1):S13–S20; Pan L, Li R, Park S, Galuska D, Sherry B, Freedman DS (2014). A longitudinal analysis of sugar-sweetened beverage intake during infancy and obesity at six years old. Pediatrics, 134(Supplement 1):S29–S35; Park S, Pan L, Sherry B, Li R (2014). A longitudinal analysis of sugar-sweetened beverage and 100% juice intake during infancy with sugar-sweetened beverage intake at six years old. Pediatrics, 134(Supplement 1):S56–S62; and Grimm KA, Kim SA, Yaroch AL, Scanlon KS (2014). Association of fruit and vegetable intake during infancy and early childhood. Pediatrics, 134(Supplement 1):S63–S69.
[37] On February 28, 2014, USDA released a final rule, replacing the interim rule issued in December 2007. The final rule raised the dollar amount for children’s fruit and vegetable purchases by more than 30 percent. It also expanded whole-grain options available to participants, provided yogurt as a partial milk substitute for women and children, allowed parents of older infants to purchase fresh fruits and vegetables instead of jarred infant food if they choose, and gave state and local agencies more flexibility to meet the nutritional and cultural needs of participants.
[38] National Academies of Sciences, Engineering, and Medicine (2017). Review of WIC Food Packages: Improving Balance and Choice (Final Report). Washington, DC: The National Academies Press, https://www.nap.edu/catalog/23655/review-of-wic-food-packages-improving-balance-and-choice-final. USDA has not acted on these recommendations as of this writing. USDA and HHS released the Scientific Report of the 2020 Dietary Guidelines Advisory Committee to the Secretaries of USDA and HHS (the basis for forthcoming 2020 Dietary Guidelines) in July 2020.
[39] Colman et al. (2012) op. cit.
[40] Au LE, Gurzo K, Paolicelli C, Whaley SE, Weinfield NS, Ritchie LD (2018). Diet quality of US infants and toddlers 7–24 months old in the WIC Infant and Toddler Feeding Practices Study-2. The Journal of Nutrition, 148(11):1786-1793. The HEI is a measure of diet quality used to assess how well a set of foods aligns with key recommendations of the Dietary Guidelines for Americans. An HEI score of 100 indicates that an individual has consumed at least the recommended daily values of 10 dietary components.
[41] Weinfield NS, Borger C, Au LE, Whaley SE, Berman D. Ritchie LD (2020). Longer participation in WIC is associated with better diet quality in 24-month-old children. Journal of the Academy of Nutrition and Dietetics, 120(6), 963-971; Au LE, Paolicelli C, Gurzo K, Ritchie LD, Weinfield NS, Plank KR, Whaley SE (2019). Contribution of WIC-eligible foods to the overall diet of 13-and 24-month-old toddlers in the WIC Infant and Toddler Feeding Practices Study-2. Journal of the Academy of Nutrition and Dietetics, 119(3): 435-448.
[42] Borger C et al. (2020). WIC Infant and Toddler Feeding Practices Study-2 Fourth Year Report. Prepared by Westat, Inc. for USDA Food and Nutrition Service, September.
[43] This analysis also suggests that the improvements in nutritional quality are not simply a reflection of unobserved differences between participants and non-participants. WIC households had healthier purchases only when benefits were redeemed. During weeks when benefits were not redeemed, the nutritional quality of purchases among WIC households was no different from that of eligible non-participating households. In addition, among those redeeming WIC benefits, the improvements in purchase quality disappeared once shopping baskets filled mainly with WIC-eligible foods were excluded from the analysis. Taken together, the evidence suggests that foods provided by WIC can explain most if not all of the improvement in the quality of food purchases. See Fang D, Thomsen MR, Nayga RM, Novotny AM (2019). WIC participation and relative quality of household food purchases: Evidence from FoodAPS. Southern Economic Journal, 86(1), 83-105.
[44] Khan R, Zhu T, Dhar S (2018). The effect of the WIC program on consumption patterns in the cereal category. Quantitative Marketing and Economics, 16(1): 79-109.
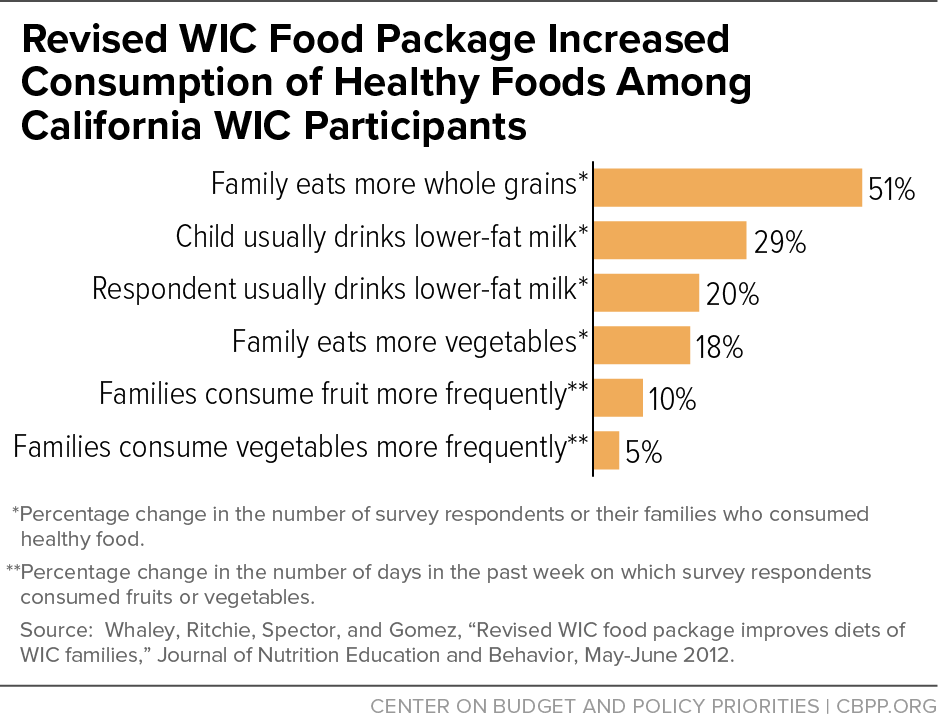
[45] Schultz DJ, Byker Shanks C, Houghtaling B (2015). The impact of the 2009 Special Supplemental Nutrition Program for Women, Infants, and Children food package revisions on participants: A systematic review. Journal of the Academy of Nutrition & Dietetics, 115:1832–46; Zhang Q, Alsuliman MA, Wright M, Wang Y, Cheng X (2020). Fruit and vegetable purchases and consumption among WIC participants after the 2009 WIC food package revision: a systematic review. Advances in Nutrition, published online May 26.; Hartline-Grafton H (2019). Impact of the Revised WIC Food Packages on Nutrition Outcomes and the Retail Food Environment. Food Research and Action Center, https://frac.org/wp-content/uploads/frac_brief_revised_wic_food_package_impact_nutrition_retail.pdf.
[46] Zhang et al., op. cit.
[47] Whaley SE, Ritchie LD, Spector P, Gomez J (2012). Revised WIC food package improves diets of WIC families. Journal of Nutrition Education and Behavior, 44(3):204-209.
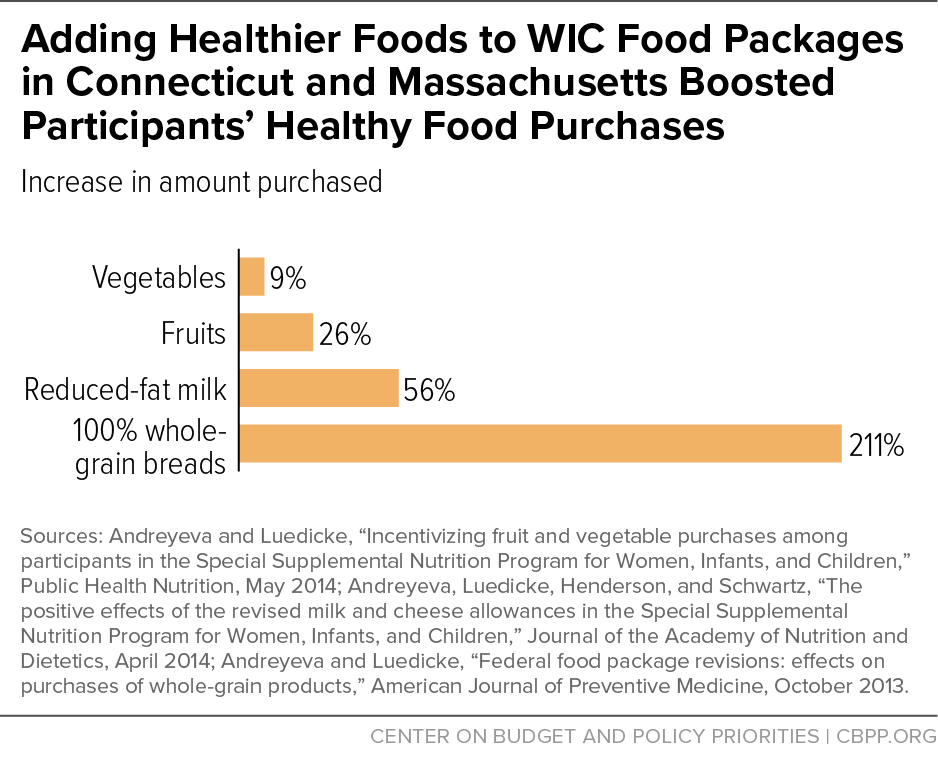
[48] Andreyeva T, Luedicke J (2014). Incentivizing fruit and vegetable purchases among participants in the Special Supplemental Nutrition Program for Women, Infants, and Children. Public Health Nutrition, 1-9; Andreyeva T, Luedicke J (2013). Federal food package revisions: effects on purchases of whole-grain products. American Journal of Preventive Medicine, 45(4):422-429; Andreyeva T, Luedicke J, Tripp AS, Henderson KE (2013). Effects of reduced juice allowances in food packages for the women, infants, and children program. Pediatrics, 131(5):919-927; Andreyeva T, Luedicke J, Henderson KE, Schwartz MB (2014). The positive effects of the revised milk and cheese allowances in the special supplemental nutrition program for women, infants, and children. Journal of the Academy of Nutrition and Dietetics, 114(4):622-630.
[49] Chiasson MA, Findley SE, Sekhobo JP, Scheinmann R, Edmunds LS, Faly AS, McLeod NJ (2013). Changing WIC changes what children eat. Obesity, 21(7): 1423-1429.
[50] Ng SW, Hollingsworth BA, Busey EA, Wandell JL, Miles DR, Poti JM (2018). Federal nutrition program revisions impact low-income households’ food purchases. American Journal of Preventive Medicine, 54(3): 403-412.
[51] Meiqari L, Torre L, Gazmararian JA (2015). Exploring the impact of the new WIC food package on lowfat milk consumption among WIC recipients: a pilot study. Journal of Health Care for the Poor and Underserved, 26(3):712725.
[52] Odoms-Young AM, Kong A, Schiffer LA, Porter SJ, Blumstein L, Bess S, Berbaum ML, Fitzgibbon ML (2014). Evaluating the initial impact of the revised Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) food packages on dietary intake and home food availability in African-American and Hispanic families. Public Health Nutrition, 17(1): 83-93.
[53] Kong A, Odoms-Young AM, Schiffer LA, Kim Y, Berbaum ML, Porter SJ, Blumstein L, Bess S, Fitzgibbon ML (2014). The 18-month impact of special supplemental nutrition program for women, infants, and children food package revisions on diets of recipient families. American Journal of Preventive Medicine, 46(6): 543-551.
[54] Ishdorj A, Capps O (2015). Rural vs. urban Texas WIC children food choices and intakes before and after changes in the food benefits. Department of Agricultural Economics, Texas A&M University; and Ishdorj A, Capps O (2013). The effect of revised WIC food packages on Native American children. American Journal of Agricultural Economics, 95(5):1266-1272.
[55] Tester JM, Leung CW, Crawford PB (2016). Revised WIC food package and children’s diet quality. Pediatrics, 137(5):e20153557 .
[56] Chaparro MP, Crespi CM, Anderson CE, Wang MC, Whaley SE (2019). The 2009 Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) food package change and children's growth trajectories and obesity in Los Angeles County. The American Journal of Clinical Nutrition, 109(5):1414-1421. Subsequent studies by the same research team suggest that the WIC food package changes may not have benefited all children equally: obesity reduction was weaker for girls in some circumstances. See Chaparro MP, Anderson CE, Crespi CM, Whaley SE, Wang MC (2019). The effect of the 2009 WIC food package change on childhood obesity varies by gender and initial weight status in Los Angeles County. Pediatric Obesity, 14(9):e12526; Anderson CE, Crespi CM, Wang MC, Whaley SE, Chaparro MP (2020). The neighborhood food environment modifies the effect of the 2009 WIC food package change on childhood obesity in Los Angeles County, California. BMC Public Health, 20: 1-11.
[57] Chaparro MP, Wang MC, Anderson CE, Crespi CM, Whaley SE (2020). The association between the 2009 WIC food package change and early childhood obesity risk varies by type of infant package received. Journal of the Academy of Nutrition and Dietetics, 120(3):371-385 and Chaparro MP, Anderson CE, Crespi CM, Wang MC, Whaley SE (2020). The new child food package is associated with reduced obesity risk among formula fed infants participating in the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) in Los Angeles County, California, 2003–2016. International Journal of Behavioral Nutrition and Physical Activity, 17(1):18.
[58] Daepp MI, Gortmaker SL, Wang YC, Long MW, Kenney EL (2019). WIC food package changes: Trends in childhood obesity prevalence. Pediatrics, 143(50): e20182841.
[59] Oberle MM, Freese R, Shults J, Stallings VA, Virudachalam S (2020). Impact of the 2009 WIC food package changes on maternal dietary quality. Journal of Hunger & Environmental Nutrition, published online February 10.
[60] Section on Breastfeeding, American Academy of Pediatrics (2012). Breastfeeding and the use of human milk. Pediatrics, 129(3):e827-e841.
[61] Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, Trikalinos T, Lau J (2007). Breastfeeding and Maternal and Infant Health Outcomes in Developed Countries. Evidence Report/Technology Assessment No. 153 (Prepared by Tufts-New England Medical Center Evidence-based Practice Center, under Contract No. 290-02-0022). AHRQ Publication No. 07-E007. Rockville, MD: Agency for Healthcare Research and Quality.
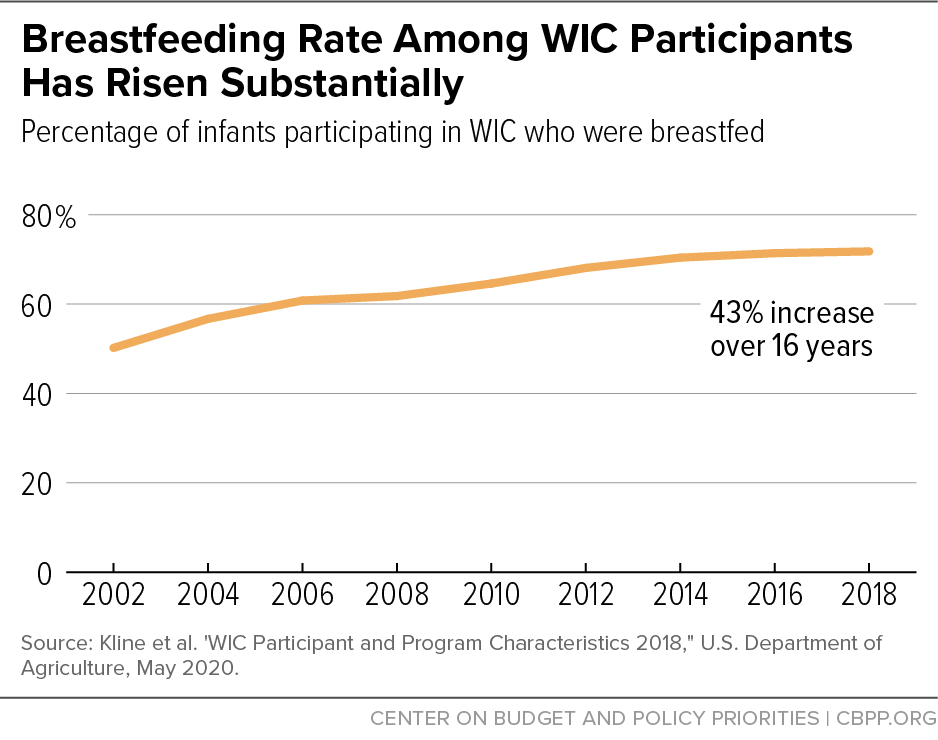
[62] See, for example, Zhang Q, Lamichhane R, Wright M, McLaughlin PW, Stacy B (2019). Trends in breastfeeding disparities in US infants by WIC eligibility and participation. Journal of Nutrition Education and Behavior, 51(2): 182-189.
[63] Gregory EF, Gross SM, Nguyen TQ, Butz AM, Johnson SB (2016). WIC participation and breastfeeding at 3 months postpartum. Maternal and Child Health Journal, 20(8):17351744.
[64] This study controlled for self-selection bias by focusing on mothers who gave birth after participating in WIC during one pregnancy but not a second. Each mother in this model essentially serves as her own control. Because the analysis is limited to mothers with multiple births and only those in South Carolina, the results may not apply to mothers with single births or to other parts of the country. See Sonchak L (2017). The impact of WIC on breastfeeding initiation and gestational weight gain: Case study of South Carolina Medicaid mothers. Children and Youth Services Review, 79:115-125.
[65] Centers for Disease Control and Prevention. Breastfeeding among U.S. children born 2002–2013, CDC National Immunization Survey accessed on February 6, 2017; Breastfeeding among U.S. children born 2010–2017, CDC National Immunization Survey available online at https://www.cdc.gov/breastfeeding/data/nis_data/results.html; accessed on September 12, 2020.
[66] Kline N, Thorn B, Bellows D, Wroblewska K. Wilcox-Cook E (2020). WIC Participant and Program Characteristics 2018. Prepared by Insight Policy Research for the Food and Nutrition Service, USDA (Appendix Table A.32). While these are the best data available, it is important to note that some of the increase in breastfeeding rates among women participating in WIC may be due to improved reporting over this period. In 2002, 68 state agencies reported WIC breastfeeding rates; by 2018 this had grown to 88 state agencies (covering 98 percent of all WIC participants). While the true increase between 2002 and 2018 may be somewhat smaller than reported, the growth in breastfeeding rates among WIC mothers still exceeds the national trend.
[67] Few studies examine the role of participants’ preference for and perceived value of WIC foods and packages in program participation and retention. Based on a survey and in-depth interviews of participants at eight WIC clinics in Illinois, researchers found that participants prioritized the infant packages over other WIC foods and packages, influenced by the high cost of infant formula. Weber S, Uesugi K, Greene H, Bess S, Reese L, and Odoms-Young A (2018). Preferences and Perceived Value of WIC Foods Among WIC Caregivers. Journal of Nutrition Education and Behavior, 50(7):695-704.
[68] Jacknowitz A Tiehen L (2010). WIC Participation Patterns: An Investigation of Delayed Entry and Early Exit. Economic Research Service, USDA, December, https://www.ers.usda.gov/webdocs/publications/44781/8018_err109.pdf?v=4458.5.
[69] Whaley SE, Whaley M, Au LE, Gurzo K, Ritchie LD (2017). Breastfeeding is associated with higher retention in WIC after age 1. Journal of Nutrition Education and Behavior, 49(10):810-816. Based on detailed discussions with a small number of WIC participants in Los Angeles, researchers speculate that mothers who formula-feed and predominantly receive material supports from WIC are less motivated to stay in the program after the formula benefits end, while breastfeeding mothers who receive both material and social supports feel more connected to WIC and are motivated to continue using WIC services even when material supports are reduced. See Almeida R, Gutierrez SA, Whaley SE, Ventura AK (2020). A qualitative study of breastfeeding and formula-feeding mothers’ perceptions of and experiences in WIC. Journal of Nutrition Education and Behavior, 52(6):615-625.
[70] Whaley SE, Martinez CE, Paolicelli C, Ritchie LD, Weinfield NS (2020). Predictors of WIC participation through 2 years of age. Journal of Nutrition Education and Behavior, 52(7): 672-679.
[71] As the committee’s report noted, “[a] breastfeeding mother — especially one who intends to combine breastfeeding and formula feeding, who needs to return to work, or who faces other personal challenges to breastfeeding — may need some formula to nourish her infant adequately during the first month postpartum. Some mothers who might otherwise try breastfeeding may choose formula feeding to be sure they can obtain formula (a high-cost item) if they run into breastfeeding difficulties.”
[72] This evaluation assessed initiation, intensity, and duration of breastfeeding. It also found that after the change, fewer WIC participants who were mothers of new infants received the partially breastfeeding package and more received the fully breastfeeding package, but more mothers also received the fully formula feeding package. Wilde P, Wolf A, Fernandez M, Collins A (2011). Evaluation of the Birth Month Breastfeeding Changes to the WIC Food Packages. Alexandria, VA: Food and Nutrition Service, USDA, https://www.fns.usda.gov/evaluation-birth-month-breastfeeding-changes-wic-food-packages.
[73] Rasmussen KM, Latulippe ME, Yaktine AL (2016). Review of WIC food packages: proposed framework for revisions (interim report). Food and Nutrition Board, Institute of Medicine, https://www.fns.usda.gov/wic/review-wic-food-packages-proposed-framework-revisions.
[74] Whaley SE, Koleilat M, Whaley M, Gomez J, Meehan K, Saluja K (2012). Impact of policy changes on infant feeding decisions among low-income women participating in the Special Supplemental Nutrition Program for Women, Infants, and Children. American Journal of Public Health, 102(12):2269-2273. It is possible that some of this increase was due to a successful breastfeeding promotion campaign for WIC participants and staff that began shortly before the introduction of the revised food packages. As noted above, Wilde et al. (2011) report a reduction in the number of mothers receiving the partial breastfeeding package but an increase in the number receiving the full-formula package in a random sample of 17 local WIC agencies.
[75] Langellier BA, Chaparro MP, Wang MC, Koleilat M, and Whaley SE (2014). The new food package and breastfeeding outcomes among women, infants, and children participants in Los Angeles County. American Journal of Public Health, 104(2):S112–S118.
[76] Thornton HE, Crixell SH, Reat AM, Von Bank JA (2014). Differences in energy and micronutrient intakes among central Texas WIC infants and toddlers after the package change. Journal of Nutrition Education and Behavior, 46(3 Supplement): S79-S86.
[77] Di H, Ishdorj A, McKyer L (2018). Impact of revised WIC food packages on infant feeding and transition to complementary foods. Presented at 2018 Agricultural and Applied Economics Association Annual Meeting, Washington, DC; and Ishdorj A, Di H, Samman E, McKyer ELJ (2020). Are rural infants benefiting from WIC food package rule changes? Breastfeeding and infant feeding behaviors. Southwest Rural Health Research Center.
[78] Li K, Wen M, Reynolds M, Zhang Q (2019). WIC participation and breastfeeding after the 2009 WIC revision: a propensity score approach. International Journal of Environmental Research and Public Health, 16(15):2645. The authors note that several earlier studies have found breastfeeding rates (initiation and duration) to be lower among WIC participants than eligible non-participants.
[79] At least one study, while observing that the rate at which children are ever breastfed increased across the nation, concluded that the increase is not associated with changes in the WIC food packages. See Joyce T, Reeder J (2015). Changes in breastfeeding among WIC participants following implementation of the new food package. Maternal and Child Health Journal, 19(4):868-876.
[80] Houghtaling B, Byker Shanks C, Jenkins M (2017). Likelihood of breastfeeding within the USDA’s Food and Nutrition Service Special Supplemental Nutrition Program for Women, Infants, and Children population: a systematic review of the literature. Journal of Human Lactation, 33(1): 83-97.
[81] Metallinos-Katsaras E, Brown L, Colchamiro R 2015. Maternal WIC participation improves breastfeeding rates: a statewide analysis of WIC participants. Maternal and Child Health Journal, 19(1):136-143.
[82] May L et al. (2017). WIC Infant and Toddler Feeding Practices Study – 2: Infant Year Report. Prepared by Westat, Inc., for the Food and Nutrition Service, USDA; Guthrie JF et al. (2018). WIC and non-WIC infants and children differ in usage of some WIC-provided foods. The Journal of Nutrition, 148 (Supplement 3): 1547S-1556S.
[83] Cook JT et al. (2013). Are food insecurity’s health impacts underestimated in the U.S. population? Marginal food security also predicts adverse health outcomes in young U.S. children and mothers. Advances in Nutrition: An International Review Journal, 4(1):51-61.
[84] We would expect WIC’s impact on food security to be relatively modest given the value of the monthly WIC food benefit — about $63 per person in fiscal year 2019. (Note that the average monthly cost to the federal government was much lower — about $41 — due to discounts on infant formula.) By way of comparison, the Supplemental Nutrition Assistance Program (food stamps) provided a monthly benefit of $130 per person in 2019.
[85] Kreider B, Pepper JV, Roy M (2016). Identifying the effects of WIC on food insecurity among infants and children. Southern Economic Journal, 82(4):1106-1122. More recent technical work suggests that participating in both SNAP and WIC may improve the food security rate by 24 percentage points compared with participating in SNAP alone. Because of the small sample used in this analysis, however, the positive impact could be as little as 1.9 percentage points. See Jensen HH, Kreider B, Zhylyevskyy O (2019). Investigating treatment effects of participating jointly in SNAP and WIC when the treatment is validated only for SNAP. Southern Economic Journal, 86(1), 124-155. Similarly, participation in both SNAP and WIC as a young child may increase the odds of being more food secure in young adulthood than in childhood compared to low-income children who do not participate in either SNAP or WIC. See Wolfson J, Insolera N, Cohen A (2019). The influence of nutrition assistance program participation, parental nutritional knowledge, and family foodways on food security and child well-being. University of Kentucky Center for Poverty Research Discussion Paper Series, DP2019-02. University of Kentucky Center for Poverty Research.
[86] Arteaga I, Heflin C, Gable S (2016). The impact of aging out of WIC on food security in households with children. Children and Youth Services Review, 69:82-96.
[87] Metallinos-Katsaras E, Gorman KS, Wilde P, Kallio J (2011). A longitudinal study of WIC participation on household food insecurity. Journal of Maternal and Child Health, 15(5):627-633.
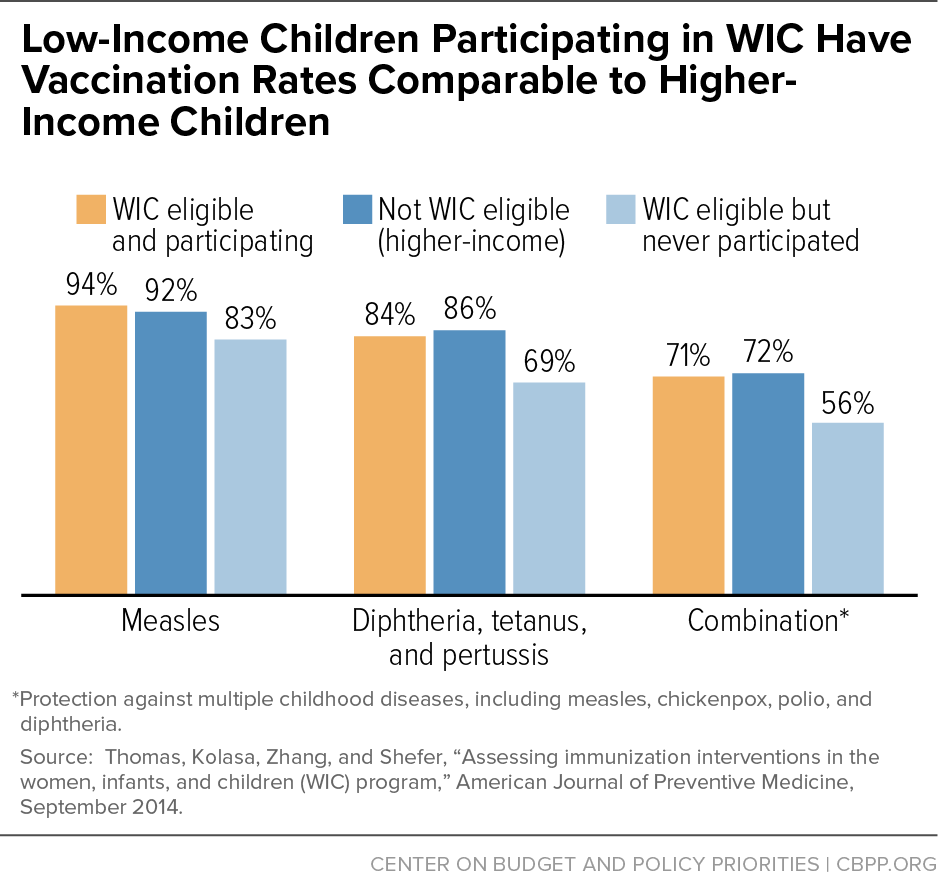
[88] Bersak T, Sonchak L (2018). The impact of WIC on infant immunizations and healthcare utilization. Health Services Research, 53.S1:2952-2969.
[89] Thomas TN, Kolasa MS, Zhang F, Shefer AM (2014). Assessing immunization interventions in the women, infants, and children (WIC) program. American Journal of Preventive Medicine, 47(5):624-628.
[90] Borger et al. (2020) op. cit.
[91] Buescher P et al. (2003). Child participation in WIC: Medicaid costs and use of health care services. American Journal of Public Health, 93(1):145-150; Chatterji P, Brooks-Gunn J (2004). WIC participation, breastfeeding practices, and well-child care among unmarried, low-income mothers. American Journal of Public Health, 94(8):1324-1327; Bersak and Sonchak (2018). One study (Chorniy, Currie, Sonchak L 2020) found no difference in access to health care between WIC children and non-WIC siblings within families. If, however, all children in a family benefit when one child gains access to health care, these estimates could underestimate WIC’s true impact on health care utilization.
[92] Anderson, PM, Butcher, KF, and Schanzenbach, DW (2019). Understanding recent trends in childhood obesity in the United States. Economics & Human Biology, 34:16-25.
[93] Fryar CD, Carroll MD, Ogden CL (2018). Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 through 2015–2016. National Center for Health Statistics, September.
[94] Pan L, Freedman DS, Park S, Galuska DA, Potter A, Blanck, H. M. (2019). Changes in obesity among US children aged 2 through 4 years enrolled in WIC during 2010-2016. Journal of the American Medical Association, 321(23), 2364-2366; Pan L, Blanck HM, Park S, Galuska DA, Freedman DS, Potter A, Petersen R (2019). State-specific prevalence of obesity among children aged 2–4 years enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children—United States, 2010–2016. Morbidity and Mortality Weekly Report, 68(46):1057.
[95] Baker RD, Greer FR, Committee on Nutrition (2010). Clinical report — Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0–3 years of age). Pediatrics, 126(5):1040-1050.
[96] Butte NF, Fox MK, Briefel, RR, Siega-Riz AM, Dwyer JT, Deming DM, Reidy KC. (2010). Nutrient intakes of US infants, toddlers, and preschoolers meet or exceed dietary reference intakes. Journal of the American Dietetic Association, 110(12):S27-S37.
[97] Yip R, Binkin NJ, Fleshood L, Trowbridge FL (1987). Declining prevalence of anemia among low-income children in the United States. Journal of the American Medical Association, 258(12):1619-1623; Yip R, Parvanta I, Scanlon K, Borland E, Russell C, Trowbridge F (1992). Pediatric nutrition surveillance system — United States, 1980-1991. Morbidity and Mortality Weekly Report, 41(7):1-24.
[98] Yen ST (2010). The effects of SNAP and WIC programs on nutrient intakes of children. Food Policy, 35(6):576-583; and Siega-Riz AM, Kranz S, Blanchette D, Haines PS, Guilkey DK, Popkin BM (2004). The effect of participation in the WIC program on preschoolers’ diets. The Journal of Pediatrics, 144(2):229-234.
[99] Jun S, Catellier DJ, Eldridge AL, Dwyer JT, Eicher-Miller HA, Bailey RL (2018). Usual nutrient intakes from the diets of US children by WIC participation and income: findings from the Feeding Infants and Toddlers Study (FITS) 2016, The Journal of Nutrition, 148(Suppl_3):1567S–1574S.
[100] U.S. Department of Agriculture, Food and Nutrition Service (2012). National Survey of WIC Participants II: Participant Characteristics Report, prepared by ICF Macro for the Office of Research and Analysis, https://www.fns.usda.gov/national-survey-wic-participants-ii.
[101] Jackson MI (2015). Early childhood WIC participation, cognitive development and academic achievement. Social Science & Medicine, 126:145-153, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4703081/. There is some evidence that brief gaps in coverage may have short-term but not long-term consequences for achievement. Children who enter kindergarten after aging out of WIC and experience a gap in nutrition assistance coverage score lower on math and reading tests in the fall of their kindergarten year, but not in the spring (see Arteaga et al. (2019). Design flaws: consequences of the coverage gap in food programs on children at kindergarten entry. Applied Economic Perspectives and Policy, 41(2): 265-283. Another study that focused on socioemotional rather than cognitive development in a small sample of Medicaid recipients in Memphis, TN found no association between WIC participation at 12 and 24 months and an assessment of infants’ and toddlers’ socioemotional competence and behavioral problems; see Arons A, Bolbocean C, Bush NR, Tylavsky FA, LeWinn KZ (2016). Participation in the special supplemental nutrition program for women, infants, and children is not associated with early childhood socioemotional development: results from a longitudinal cohort study. Preventive Medicine Reports, 4:507511, http://www.sciencedirect.com/science/article/pii/S2211335516301103.
[102] Chorniy, Currie, Sonchak L (2020) op. cit. Note that some of those whose mothers participated during pregnancy may also have received WIC benefits as children. Among children in South Carolina who were covered prenatally, 89.3 percent continued to receive WIC services in their first year of life, dropping to 60.6 percent, 42.8 percent, 31.0 percent, and 22.0 percent in the four years that follow.
[103] Although the evidence is at best anecdotal, food manufacturers may also respond to WIC’s food package requirements by reformulating their products. In the mid-1980s, for example, General Mills increased the amount of iron in Cheerio s— one of the most popular WIC-eligible cereals — so that it would meet program requirements.
[104] Ploeg MV, Breneman V, Farrigan T, Hamrick K, Hopkins D, Kaufman P, Lin BH, Tuckermanty E (2009). Access to Affordable and Nutritious Food: Measuring and Understanding Food Deserts and Their Consequences. Report to Congress. Economic Research Service, USDA, https://www.ers.usda.gov/webdocs/publications/ap036/12716_ap036_1_.pdf.
[105] USDA reports that about 1 in 5 WIC households live more than a mile from a supermarket in urban areas and more than 10 miles from a supermarket in rural areas. Nearly 90 percent of mothers agree, however, that fresh fruits and vegetables are easy to purchase and plentiful in their communities. See Borger et al. (2020) op. cit.
[106] An examination of rules in place in 2017 found a wide range of minimum stocking requirements for WIC-authorized retailers across states, which may result in disparities in food and beverage products available to WIC recipients depending on their state of residence and the size or type of stores available in their neighborhoods. See Pelletier JE, Schreiber LR, Laska MN (2017). Minimum stocking requirements for retailers in the Special Supplemental Nutrition Program for Women, Infants, and Children: disparities across US states. American Journal of Public Health, 107(7), 1171-1174.
[107] Tiehen L Frazão E (2016). Where Do WIC Participants Redeem Their Food Benefits? An Analysis of WIC Food Dollar Redemption Patterns by Store Type. Economic Research Service, USDA, https://www.ers.usda.gov/webdocs/publications/eib152/57246_eib152.pdf.
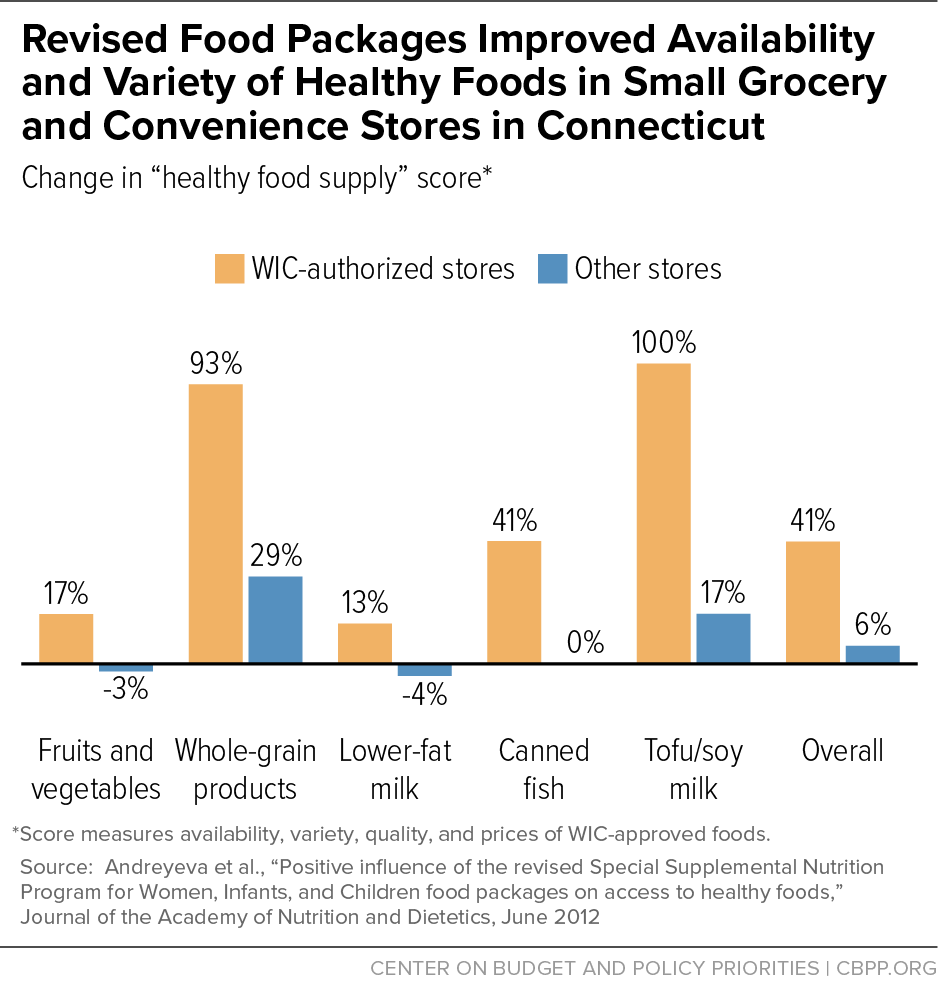
[108] Andreyeva T, Luedicke J, Middleton AE, Long MW, Schwartz MB (2012). Positive influence of the revised Special Supplemental Nutrition Program for Women, Infants, and Children food packages on access to healthy foods. Journal of the Academy of Nutrition and Dietetics, 112(6):850-858; Havens EK, Martin KS, Yan J, Dauser-Forrest D, Ferris AM (2012). Federal nutrition program changes and healthy food availability. American Journal of Preventive Medicine, 43(4):419-422.
[109] Hillier A, McLaughlin J, Cannuscio CC, Chilton M, Krasny S, Karpyn A (2012). The impact of WIC food package changes on access to healthful food in 2 low-income urban neighborhoods. Journal of Nutrition Education and Behavior, 44(3):210-216.
[110] Rose D, O’Malley K, Dunaway LF, Bodor JN (2014). The influence of the WIC food package changes on the retail food environment in New Orleans. Journal of Nutrition Education and Behavior, 46(3 Supplement):S38-44.
[111] Zenk SN, Odoms-Young A, Powell LM, Campbell RT, Block D, Chavez N, Krauss RC, Strode S, Armbruster J (2012). Fruit and vegetable availability and selection: federal food package revisions, 2009. American Journal of Preventive Medicine, 43(4):423-428.
[112] Gleason S, Morgan R, Bell L, Pooler J (2011). Impact of the Revised WIC Food Package on Small WIC Vendors. Alexandria, VA: Altarum Institute, http://altarum.org/sites/default/files/uploaded-related-files/FourStateWICFoodPackageEvaluation-Exec%20Summary-22Mar11_0.pdf.
[113] Cobb LK, Anderson CA, Appel L, JonesSmith J, Bilal U, Gittelsohn J, Franco M (2015). Baltimore City stores increased the availability of healthy food after WIC policy change. Health Affairs, 34(11):18491857.
[114] Lu W, McKyer DL, Dowdy D, Evans A, Ory M, Hoelscher DM, Wang S, Miao J (2016). Evaluating the influence of the revised Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) food allocation package on healthy food availability, accessibility, and affordability in Texas. Journal of the Academy of Nutrition and Dietetics, 116(2):292-301.
[115] Hudak KM, Paul R, Gholizadeh S, Zadrozny W, Racine EF (2020). Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) authorization of discount variety stores: leveraging the private sector to modestly increase availability of healthy foods. The American Journal of Clinical Nutrition, 111(6): 1278-1285.
[116] Chauvenet C, De Marco M, Barne, C, Ammerman AS (2019). WIC recipients in the retail environment: a qualitative study assessing customer experience and satisfaction. Journal of the Academy of Nutrition and Dietetics, 119(3), 416-424. Many of the interviews in this study were conducted in states prior to the implementation of Electronic Benefit Transfer (EBT) systems and mobile phone applications to help with WIC shopping. Participants who had experience with EBT reported a smoother checkout process since EBT’s implementation.
[117] See, for example, Besharov DJ, Germanis P (2001). Rethinking WIC: An Evaluation of the Women, Infants, and Children Program. Washington, DC: American Enterprise Institute.
[118] Bitler MP, Currie J (2005). Does WIC work? The effects of WIC on pregnancy and birth outcomes. Journal of Policy Analysis and Management, 24(1):73-91.
[119] Joyce T, Racine A, Yunzal‐Butler C (2008). Reassessing the WIC effect: evidence from the pregnancy nutrition surveillance system. Journal of Policy Analysis and Management, 27(2):277-303.
[120] Fingar KR, Lob SH, Dove MS, Gradziel P, Curtis MP (2016). Reassessing the association between WIC and birth outcomes using a fetusesatrisk approach. Maternal and Child Health Journal, published online August 16, 2016.
[121] Nobles J, Hamoudi, A (2019). Detecting the effects of early-life exposures: why fecundity matters. Population Research and Policy Review, 38(6), 783-809.