BEYOND THE NUMBERS
This is the next in our “Medicaid Works” blog series, which aims to inform the debate over Medicaid’s future by providing the latest facts and figures on this essential and popular part of the nation’s health care system.
Debates over issues like health reform’s Medicaid expansion or proposals to turn Medicaid into a block grant often raise important questions about states’ role in Medicaid. Here are two relevant points from our recently updated paper.
1. Medicaid gives states significant flexibility to design their own programs — whom they cover, what benefits they provide, and how they deliver health care services.
The federal government sets minimum standards, including the categories of people that all states must cover. Beyond that, states set their own rules. As a result, Medicaid eligibility varies substantially from state to state.
Medicaid benefits vary significantly as well. States decide whether to cover services like dental and vision care for adults and the amount, duration, and scope of the services they provide. States also decide whether Medicaid delivers health care services through managed care, fee-for-service, or other delivery systems, and how much they will pay providers and plans that serve Medicaid beneficiaries.
Many states take advantage of Medicaid’s flexibility to improve beneficiaries’ health while lowering costs, as we explain in this paper. Oregon, for example, has established accountable care organizations — groups of providers and other entities that partner with one another to provide a range of health care services in a coordinated way — to integrate hospital-based services with primary care, behavioral health care, and other social supports. Oregon has seen emergency room visits and preventable hospital admissions fall significantly, while lowering its growth in Medicaid spending per beneficiary by two percentage points below the levels projected without the waiver.
2. Health reform’s Medicaid expansion has not only helped millions of low-income people gain health coverage but also produced state savings.
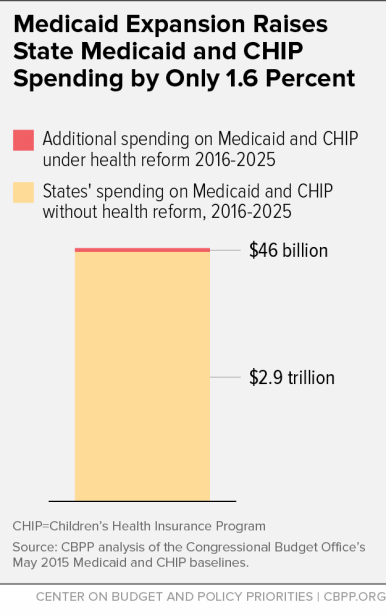
Under health reform, the federal government picks up 100 percent of the expansion’s cost through 2016 and at least 90 percent thereafter. The federal share will average roughly 95 percent from 2016 to 2025, the Congressional Budget Office (CBO) estimates. CBO estimates also show that states will spend just 1.6 percent more on Medicaid and the Children’s Health Insurance Program (CHIP) with the expansion than they would have without health reform, if most states adopt the expansion (see graph).
For many states, in fact, the expansion has produced net savings. One reason is that demand for entirely state-funded services that serve the uninsured (such as mental health and behavioral health programs) has fallen as more low-income residents have gained health coverage. In addition, expansion states are collecting more revenue from existing taxes on health plans and providers, such as the managed care plans that serve Medicaid beneficiaries in many states, which have experienced a surge in enrollment due to expansion.
While some critics argue that the federal government will someday renege on its commitment to finance nearly all expansion costs, history shows that’s unlikely. Congress has only modified Medicaid’s overall matching rate three times over the last three and a half decades, and the most recent changes were temporary increases to aid states during the last two economic downturns.
Learn more about how Medicaid works for children, families, and seniors across the country: www.cbpp.org/medicaid-works.