BEYOND THE NUMBERS
House GOP Medicaid Provisions Would Shift $370 Billion in Costs to States Over Decade
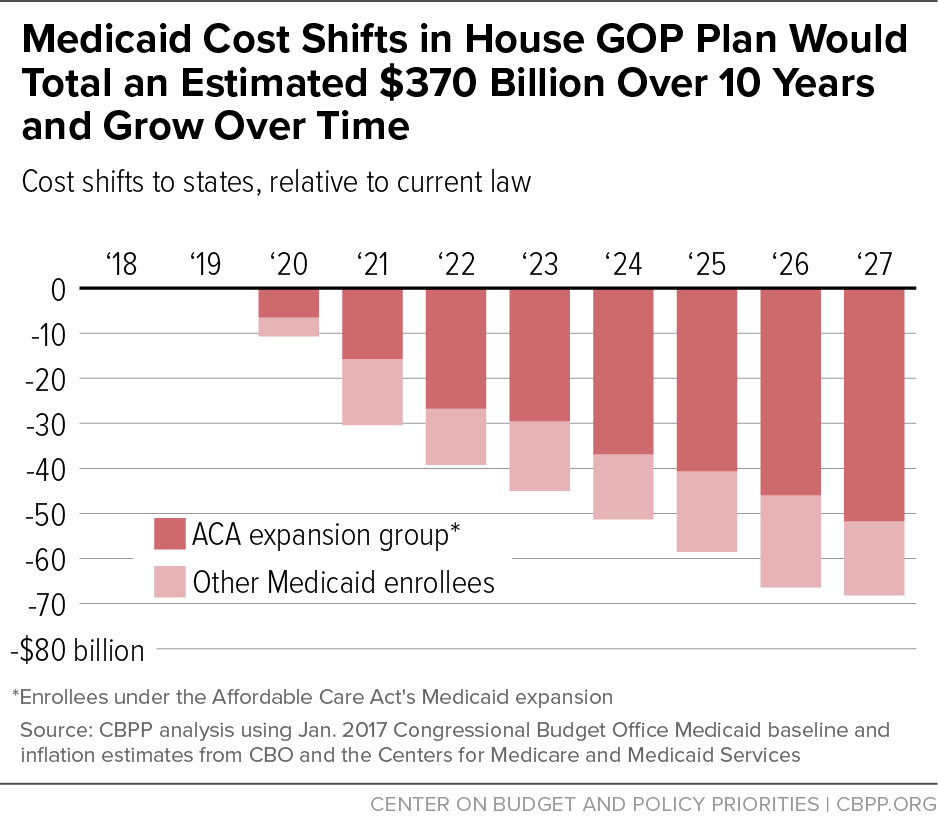
The new House Republican health plan would shift an estimated $370 billion in Medicaid costs to states over the next ten years, effectively ending the Affordable Care Act’s (ACA) Medicaid expansion for 11 million people while also harming tens of millions of additional seniors, people with disabilities, and children and parents who rely on Medicaid today. (See chart.)
The legislation, which the House Energy and Commerce Committee is scheduled to consider on March 8, would:
End the Medicaid expansion. Starting in 2020, states would receive only the regular federal Medicaid matching rate — on average, 57 percent of Medicaid costs, with states covering the other 43 percent — for any new enrollees under the expansion instead of the ACA’s matching rate of 90 percent. This means that expansion states would have to pay 2.8 to 5 times more in terms of their own costs.
While states could still get the expansion matching rate for beneficiaries who were enrolled before the end of 2019 and stayed enrolled without a break in coverage, the large majority of beneficiaries now on Medicaid under the expansion would likely fall off the program after two years, with further continued declines after that. As four GOP senators from expansion states wrote to Majority Leader Mitch McConnell yesterday, commenting on an earlier leaked House draft featuring a virtually identical Medicaid expansion proposal, “many [Medicaid beneficiaries] cycle on and off Medicaid due to frequent changes in income, family situations, and living environments.”
Thus, within just a few years, the overwhelming share of Medicaid expansion spending would eventually be subject to the regular matching rate. To maintain the expansion as it’s now operating in the expansion states, we estimate that these states would have to increase their share of costs by about $253 billion over ten years. (This figure includes the added effect of applying a per capita cap — as described below — to the Medicaid expansion.)
In seven states, expansion coverage would automatically end because state law requires their expansion to end if the federal Medicaid matching rate falls or requires the state to take steps to prevent its Medicaid costs from rising. As a practical matter, most or all of the other 25 expansion states (including the District of Columbia) also would have to end their expansions. This means that the actual cut in federal Medicaid spending resulting from the reduction in the expansion rate would likely be much larger than $253 billion, as states drop the expansion entirely. It also means that the 11 million low-income adults in 32 states who gained Medicaid coverage through the expansion would lose it; most would likely become uninsured.
Convert Medicaid to a per capita cap. The House proposal would cap federal funding on a per-beneficiary basis for virtually all of Medicaid (including the Medicaid expansion) starting in 2020. The caps would be based on states’ per-beneficiary spending in fiscal year 2016 and would rise annually to match growth in the medical care component of the Consumer Price Index (M-CPI).
Because Medicaid costs per beneficiary are expected to rise by about 0.2 percentage points faster each year than states’ capped amounts, states would get less federal funding than under current law, with the cuts growing each year. We estimate that this provision would cut federal Medicaid spending by an additional $116 billion over the next decade — on top of the $253 billion in cuts to the Medicaid expansion as described above.
Moreover, this estimate assumes state Medicaid costs will grow as the Congressional Budget Office now forecasts in its baseline. In reality, the cost-shift to states under a per capita cap could be much larger. That’s because states would be responsible for 100 percent of any costs in excess of the per capita cap, whether due to unanticipated health care cost growth or to demographic changes that a per capita cap wouldn’t account for. For example, states would be responsible for all costs due to an epidemic, a new treatment, or higher costs as seniors on Medicaid move from young-old age to old-old age and have much greater medical and long-term care needs and costs.
Converting Medicaid to a per capita cap would also make the program highly vulnerable to more cuts in the future. If the President and Congress delink federal Medicaid funding from the actual cost of providing health care to vulnerable Americans, they or future federal policymakers could come back and ratchet down the already arbitrary per beneficiary caps — by, for example, lowering the annual growth rate for the cap amounts — to pay for other priorities.
In response, states would have to contribute much more of their own funding or, far likelier, substantially cut eligibility, benefits, and provider payments, with those cuts growing more severe each year. Along with those who’ve gained coverage under the Medicaid expansion who would lose it, the remaining 63 million children and families, seniors, and people with disabilities who rely on Medicaid today would face the significant risk of ending up uninsured or losing access to needed care.