|
Revised August 31, 2007
MORE AMERICANS, INCLUDING MORE CHILDREN,
NOW LACK HEALTH INSURANCE
The number of uninsured Americans rose for the sixth consecutive year in 2006, to 47.0 million,[1], [2] and the number of uninsured children rose for the second straight year, to 8.7 million, according to Census data released on August 28. Between 1998, the year the State Children’s Health Insurance Program (SCHIP) was implemented, and 2004, the number of uninsured children fell every year. But since 2004, as the availability of funding for SCHIP expansion has tightened and as a restrictive Medicaid policy enacted in early 2006 has taken effect, progress in enrolling uninsured children in SCHIP and Medicaid has stalled. (Other factors very likely contributed to this outcome, as well.) With employer-based coverage continuing to erode, the number of uninsured children under 18 has jumped by 1 million over the past two years — from 7.7 million uninsured children in 2004 to 8.7 million in 2006.
“The number of uninsured children fell when the federal government and states worked together to increase coverage for children under SCHIP and Medicaid,” noted Robert Greenstein, executive director of the Center on Budget and Policy Priorities. “Now, progress has stalled and begun to reverse. Moreover, the Administration has announced a new policy that further weakens children’s coverage under SCHIP by placing coverage of as many as several hundred thousand children at risk. The new Census data underscore the need for Congress to complete work on — and the President to sign — a strong SCHIP reauthorization bill before the program expires on September 30.”
The House and Senate have both passed SCHIP reauthorization bills that would make substantial progress in this area. The Congressional Budget Office (CBO) estimates the bills would allow 3.2 to 4.2 million uninsured children to gain coverage by 2012, and also prevent 800,000 now-insured children from losing coverage. The President, however, has threatened to veto both bills. “The disturbing Census data on the rising numbers of uninsured children should prompt President Bush to reconsider his hard-line stance,” Greenstein said.
Overall Findings from the New Census Data
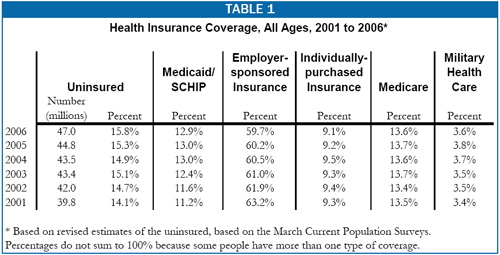
- The new Census reports find that 47.0 million Americans were uninsured in 2006, an increase of 2.2 million over the number of uninsured in 2005 (44.8 million). Although it has been five years since the 2001 recession, the number of uninsured Americans has continued to climb and is more than 7 million higher than when the recession hit bottom that year. (See Table 1.)
- The percentage of Americans without insurance climbed to 15.8 percent in 2006, above the 15.3 percent level in 2005 and considerably above the 14.1 percent level in 2001. The percentage of Americans without insurance has increased largely because employer-sponsored insurance coverage has continued to erode.
- People with low incomes are much more likely to be uninsured. Some 25 percent of people with incomes below $25,000 were uninsured in 2006, almost triple the 8.5 percent rate among people with incomes over $75,000.
- The percent of full-time working adults who lack health insurance rose to 17.9 percent in 2006, up from 17.2 percent. The number of full-time working adults who are uninsured climbed by 1.2 million, to 22.0 million.
- African-Americans (20.5 percent uninsured) and Hispanics (34 percent) are much more likely to be uninsured than non-Hispanic whites (10.8 percent). The percentage of African-Americans and Hispanics who are uninsured rose in 2006.
- Non-citizen immigrants were much more likely to be uninsured (45 percent uninsured) than native-born citizens (13 percent). The percentage of both native-born citizens and non-citizen immigrants who are uninsured increased in 2006.
- Unlike in prior years, the Census Bureau has not yet published data that show the extent to which health insurance coverage has changed at the state level. Because of technical revisions, analysts should be cautious in making comparisons to previously published state estimates.
Findings about Children
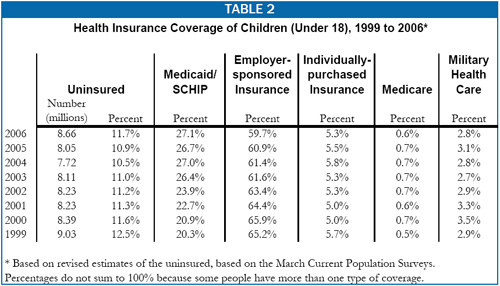
- The number of uninsured children under age 18 rose by 600,000, from 8.05 million in 2005 to 8.66 million in 2006. The percentage of children who lack health insurance also rose from 10.9 percent to 11.7 percent.
- As Table 2 indicates, the number and percentage of children who are uninsured declined from 1999 through 2004, but that trend stopped and began to reverse in 2005.[3]
- Rising enrollment in SCHIP and Medicaid was the main factor that drove down the number and percentage of uninsured children from 1998 to 2004. These enrollment increases more than offset the declines in employer-based coverage of children that began in 2000.
- From 2004 to 2006, the percentage of children covered by public insurance remained unchanged and thus could not offset the continued reduction in the percentage of children covered by employer-sponsored insurance. The result was an overall reduction in children’s coverage.
|
What Do the Census Health Insurance Data Measure?
Each March, the Census Bureau asks what types of health insurance people ever had in the previous calendar year and whether someone was uninsured for the entire year. However, the Census Bureau, CBO and other analysts note that the responses provided appear to correspond more closely to health insurance coverage at a given point in time. As with any household survey, the estimates are subject to misunderstanding by respondents or misreporting.
The Census Bureau recently revised its estimates of the number of uninsured people after it detected that a technical error had been resulting in a slight undercount of the number of dependents with private health coverage. The Census Bureau has revised its data for the years 1996 through 2005 to reflect this correction and has applied the modification to the new 2006 data. The revisions slightly reduce the number and percentage of Americans who are uninsured, but are similar for each year, so there is little effect on trends over time. (Cheryl Lee and Sharon Stern, “Health Insurance Estimates from the U.S. Census Bureau: Background for a New Historical Series, Census Bureau, June 2007) |
Insurance Coverage and the Debate over SCHIP
The main reason that both children and adults have been losing ground in health insurance coverage is the erosion of employer-sponsored insurance. Job-based coverage is falling primarily because of the high cost of health care, which has been rising faster than the economy has been growing. As a result, both employers and employees are having greater difficulty affording health insurance.
Some, like President Bush and HHS Secretary Michael Leavitt, believe that expanding public coverage is counterproductive because it “crowd outs” private health insurance. Most leading experts reject this simplistic formulation, noting that any effort to subsidize health insurance coverage — including subsidies provided through the tax code as the President has proposed — will substitute in part for expenditures for health coverage that are already being made. As M.I.T. health economist Jonathan Gruber, whose work on SCHIP crowd-out is widely cited by Administration officials and conservative think tanks, has emphasized, expanding coverage through programs like SCHIP or Medicaid is far more efficient — and results in substantially greater gains in insurance coverage — than tax-subsidy approaches. Gruber has written that “public insurance expansions like SCHIP remain the most cost-effective means of expanding health insurance coverage.”[4]
Similarly, Congressional Budget Office director Peter Orszag has commented that the approaches taken under the Senate and House SCHIP reauthorization bills — under which several million children who otherwise would be uninsured would gain coverage, with relatively modest “crowd-out” efforts)[5] — are probably about as efficient a way as possible to achieve coverage expansions of this magnitude.[6]
|
Federal Policy Actions and Inactions
Apparently Contributed to Drop in Children’s Coverage
Two problems, among others, may have contributed to the reduction in children’s health coverage in 2005 and 2006. (Both of these problems would be addressed by the SCHIP reauthorization bills recently approved by the House and Senate.)
- Shortfalls in SCHIP Funding. In fiscal years 2006 and 2007, a number of states had insufficient federal SCHIP funding to sustain their existing programs (in part due to the fact that Congress and the Administration let $1.4 billion in SCHIP funds that had not yet been spent be returned to the Treasury at the end of fiscal years 2004 and 2005). The federal government ultimately stepped in to make funding adjustments needed to fill these states’ shortfalls, but it was slow in doing so. The funding adjustments needed for fiscal year 2006 were not enacted until February 2006, five months into the fiscal year. The adjustments for fiscal year 2007 were not completed until May 2007, eight months into the fiscal year. These shortfalls and overall uncertainty about the adequacy of SCHIP funding may have discouraged some states from continuing to promote children’s enrollment as intensively. (An important goal of the SCHIP reauthorization bills the Senate and House have approved is to provide stable and predictable funding levels that enable states to strengthen children’s enrollment.)
Medicaid Enrollment Barriers Due to Citizenship Documentation. The Deficit Reduction Act of 2005 required that, starting in July 2006, most children and parents applying for, or seeking to remain enrolled in, Medicaid provide birth certificates, passports, or similar documents to prove their citizenship. Reports by the Government Accountability Office (GAO), the Center on Budget and Policy Priorities, and the House Oversight and Government Reform Committee, based on data from the states, have all found that large numbers of otherwise-eligible children and parents have been removed from Medicaid, denied entry into the program, or had their entry delayed because they did not have such documents readily available. The GAO found that 22 of 44 states responding to its survey reported that Medicaid enrollment has fallen because of these new requirements, and administrative data reported by the states indicate that Medicaid enrollment nationally fell by more than 500,000 people in the last six months of 2006.2 (Much of this drop may ultimately show up in the Census data for 2007, rather than in the recently released data for 2006.) State data reported by the Center on Budget and Policy Priorities also indicate that tens of thousands of low-income citizen children (or possibly a larger number) have lost coverage as a result of the requirement. (The House and Senate SCHIP bills would provide states with more flexibility in assessing the citizenship status of Medicaid beneficiaries so states can use procedures that do not deprive eligible citizen children of coverage.)
_______________________
1. Government Accountability Office, States Reported That Citizenship Documentation Resulted in Enrollment Declines for Eligible Citizens and Posed Administrative Burdens, GAO-07-889, June 2007; Committee on Oversight and Government Reform, majority staff, “Medicaid Citizenship Documentation Requirements Deny Coverage to Citizens and Cost Taxpayers Millions,” July 24, 2007; Donna Cohen Ross, “New Medicaid Citizenship Documentation Requirement Is Taking a Toll,” Center on Budget And Policy Priorities, March 13, 2007; and “Medicaid Requirement Disproportionately Harms Non-Hispanics, State Data Show,” Center on Budget and Policy Priorities, July 10, 2007.
2 Total Medicaid enrollment, as reported in Medicaid managed care enrollment reports. This includes all Medicaid beneficiaries and does not break out children. However, children constitute about half of all Medicaid enrollees, however, and clearly account for a major share of the enrollment reduction. Most elderly and disabled Medicaid beneficiaries are exempt from the requirement. In addition, at the same time that Medicaid enrollment was falling by 500,000 people in the last half of 2006, participation in the Food Stamp Program, which does not contain a similar requirement, was rising by almost 400,000 people. |
The Administration’s New SCHIP Policy
On August 17, the Administration announced a controversial new policy that effectively bars states from providing SCHIP coverage to children with incomes above 250 percent of the poverty line ($42,925 per year for a family of three).[7] Governors have objected to the new policy on a bipartisan basis and asked that it be withdrawn. Under the new policy, states cannot continue to cover children above 250 percent of the poverty line (or expand their programs to cover children above this income level) unless they meet certain other requirements, including a requirement that 95 percent of the children eligible for Medicaid and SCHIP in the state who have incomes below 200 percent of the poverty line must be enrolled. No state in the country meets the 95 percent participation rate criterion, a standard that significantly exceeds the participation rate in virtually every means-tested program in the country and is essentially unattainable. Since this criterion generally cannot be met, states that already serve these children will have to cut their programs back, and various states now planning to expand SCHIP coverage will be prevented from doing so.
The Congressional Research Service has reported that in fiscal year 2006, about 10 percent of the children enrolled in SCHIP had family incomes above 200 percent of the poverty line.[8] While we do not have specific data on the number of children in SCHIP who have incomes above 250 percent of the poverty line, the CRS estimates (and the fact that several states have enacted legislation since fiscal year 2006 to extend coverage to some children above this level), suggest that the number of children adversely affected by this new policy would be as many as several hundred thousand. Unless the policy is withdrawn or substantially modified, it will increase the number of uninsured children over time, as states comply with the policy and reduce their SCHIP eligibility limits.
End Notes:
[1] Carmen DeNavas-Walt, et al., “Income, Poverty and Health Insurance Coverage in the United States: 2006,” U.S. Census Bureau, Aug. 28, 2007.
[2] The Census Bureau recently announced it has slightly revised its estimates of health insurance coverage because of a technical error that affected many years of previously published data. This technical revision is discussed in the box on page 4. Our analyses are based on the Census Bureau’s new 2006 data and Census’ revised data for previous years.
[3] The Census data and findings from the Center for Disease Control and Prevention’s National Health Interview Survey reveal similar trends, although there are some differences in details. For example, the Census data found that children’s health insurance began to fall in 2005, while the CDC data did not show a reduction until 2006
[4] Gruber continued: “I have undertaken a number of analyses to compare the public sector costs of public sector expansions such as SCHIP to alternatives such as tax credits. I find that the public sector provides much more insurance coverage at a much lower cost under SCHIP than these alternatives. Tax subsidies mostly operate to “buy out the base” of insured without providing much new coverage.” Letter from Jonathan Gruber to Representative John Dingell, Chairman of the House Energy and Commerce Committee, March 2007.
[5] The Congressional Budget Office estimates that under the Senate and House SCHIP bills, about two-thirds of the children gaining SCHIP or Medicaid coverage would otherwise be uninsured, while about one-third otherwise would have private coverage. In contrast, analysis by Jonathan Gruber of M.I.T. of the health-insurance tax proposals that the Administration included in its budget last year found that 77 percent of the benefits would go to people who already were insured and there could be a slight net increase, rather than a reduction, in the number of uninsured people.
[6] During Senate Finance Committee consideration of the SCHIP legislation on July 17, 2007, Orszag stated in response to a question that, to reach several million uninsured children, the approach reflected in the Senate legislation is “pretty much as efficient as you can possibly get.”
[7] Christopher Lee, “New Bush Policies Limit Reach of Child Insurance Plan,” Washington Post, Aug. 21, 2007. Robert Pear, “New Rules May Limit Health Care Program Aiding Children,” New York Times, Aug. 21, 2007. Kevin Freking, “State Officials Disagree with New Federal Policy on Children's Insurance” Associated Press, Aug. 23, 2007.
[8] Memorandum from Chris Peterson and Elicia Herz, Congressional Research Service, March 13, 2007. |