FUTURE MEDICAID GROWTH IS NOT DUE TO FLAWS IN THE PROGRAM'S DESIGN, BUT TO DEMOGRAPHIC TRENDS AND GENERAL INCREASES IN HEALTH CARE COSTS
| PDF of full report |
| If you cannot access the files through the links, right-click on the underlined text, click "Save Link As," download to your directory, and open the document in Adobe Acrobat Reader. |
New Health and Human Services Secretary Mike Leavitt has begun discussing plans for $60 billion in Medicaid cuts over the next ten years as part of the Administration’s federal budget proposal for fiscal year 2006, which will be released on Monday, February 7. A key rationale for the effort to cut Medicaid is that the program’s costs are expected to grow faster than the general economy in the future, leading to the belief that Medicaid growth is “unsustainable.” This brief report attempts to sort out the reasons for this rise, as well as the consequences of attempting to curtail this trend without addressing its underlying causes.[1]
In short, the rise in Medicaid costs is not due to the design of the Medicaid program. Rather, it is due to two broader trends — increases in health care costs that are affecting the U.S. health care system as a whole, including the private sector, and the aging of the population. Specifically:
- Eligibility or benefit expansions have not contributed to Medicaid cost growth for some time. To the contrary, states have instituted an unprecedented series of Medicaid budget cuts and cost containment practices in recent years. States pay nearly half of the costs of Medicaid and have a powerful incentive to run the program efficiently and to hold down Medicaid expenditures. Indeed, millions of low-income Americans do not meet the stringent eligibility criteria set for Medicaid in their state and remain uninsured, while Medicaid payments to health care providers often are well below those that Medicare and the private sector pay.
- Projected increases in Medicaid costs reflect the steady rise in health care costs that affect private insurance, Medicare, and Medicaid alike. This rise in costs throughout the U.S. health care system is driven in substantial part by advances in medical technology that improve health and prolong life, but increase health care costs.
-
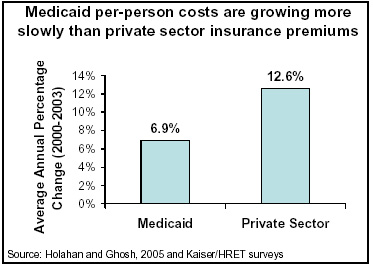 In terms of their costs per
beneficiary, Medicaid costs have risen much more slowly in recent years
than private insurance costs. A just-published study by two Urban Institute
researchers, commissioned by the Kaiser Family Foundation, found that Medicaid
acute care costs per enrollee rose an average of 6.9 percent per year from
2000 to 2003. This is little more than half the 12.6 percent per year growth
in the cost of private health insurance premiums found by a survey by the
Kaiser Foundation.[2]
(These growth figures do not include an inflation adjustment; relative to the
overall change in the cost of living, Medicaid acute costs per enrollee rose
an average of 4.6 percent per year from 2000 to 2003.)
In terms of their costs per
beneficiary, Medicaid costs have risen much more slowly in recent years
than private insurance costs. A just-published study by two Urban Institute
researchers, commissioned by the Kaiser Family Foundation, found that Medicaid
acute care costs per enrollee rose an average of 6.9 percent per year from
2000 to 2003. This is little more than half the 12.6 percent per year growth
in the cost of private health insurance premiums found by a survey by the
Kaiser Foundation.[2]
(These growth figures do not include an inflation adjustment; relative to the
overall change in the cost of living, Medicaid acute costs per enrollee rose
an average of 4.6 percent per year from 2000 to 2003.)
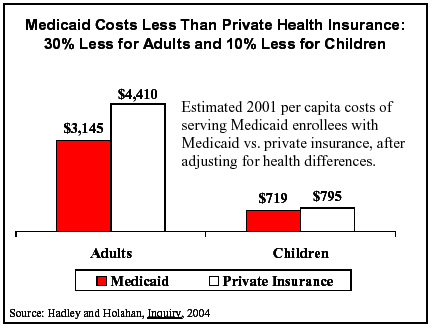
- Moreover, Medicaid costs per person are substantially lower than those for private health insurance. Another recent Urban Institute study found that, after adjusting for differences in health status and other characteristics, average medical expenditures for adults enrolled in Medicaid were nearly 30 percent lower than medical costs would be under private health insurance. Similarly, average medical expenditures for children enrolled in Medicaid were 10 percent lower than costs would be under private insurance (Figure 4).[3]
-
 Of further interest, the provision of health
care to low-income people who are elderly or have serious disabilities
accounts for the bulk — 70 percent — of Medicaid costs. And more than
40 percent of Medicaid costs are for low-income elderly or disabled people
who also are enrolled in Medicare.
Of further interest, the provision of health
care to low-income people who are elderly or have serious disabilities
accounts for the bulk — 70 percent — of Medicaid costs. And more than
40 percent of Medicaid costs are for low-income elderly or disabled people
who also are enrolled in Medicare.
A substantial share of these Medicaid costs stem from gaps in Medicare coverage. For example, Medicare generally does not cover nursing home care. Medicare’s lack of nursing home coverage forces Medicaid to pick up nursing home care costs not only for individuals who already are poor, but also for the much larger number of elderly and disabled people who deplete their assets in paying for nursing home care, fall into poverty at some point after entering a nursing home, and qualify for Medicaid from that time forward. Medicaid picks up nearly half — 46 percent — of all costs of nursing home care in the country.
Most of the remaining 30 percent of Medicaid costs goes for coverage of low-income children and pregnant women.
- Another reason that Medicaid costs
have grown in recent years is that Medicaid has picked up coverage for
substantial numbers of low-income families that have lost insurance because of
the erosion of employer-based coverage or because they lost their jobs in the
economic downturn and have not found new jobs that offer employer-based
insurance. Had Medicaid and SCHIP[4]
enrollment not grown, there would now be millions more uninsured children and
adults.
This type of enrollment growth is expected to subside as the economy and the labor market improve. The only area of Medicaid enrollment growth anticipated by the Congressional Budget Office over the next decade is a slight growth in the number of elderly or disabled beneficiaries due to the aging of the population.
As this discussion indicates, meaningful relief from rising Medicaid costs rests upon broader efforts to address health care cost increases throughout the U.S. health care system and to close gaps in Medicare coverage. In the absence of such broader efforts, reductions in the federal contribution for Medicaid costs would have adverse consequences.
Such reductions would shift health care costs from the federal government to states and localities. State and local governments would then be faced with choosing between two undesirable alternatives. They could either try to maintain current health care coverage with fewer federal funds (which would compound problems in the rest of their budgets and likely lead to cuts in other programs such as education unless they raised taxes) or they could cut back on health care coverage for low-income families, seniors, and people with disabilities, and cause increases in the ranks of the uninsured and the underinsured. Federal cutbacks to Medicaid also would shift costs to health care providers to the degree that providers furnish care for which they do not receive compensation, and to low-income people to the degree that they are forced to shoulder more of their medical bills out of their poverty-level incomes and to cut back on expenditures for other items such as food.
- Reductions in Medicaid funding without accompanying action to reduce the rate of health-care cost growth systemwide or to close gaps in Medicare coverage would inevitably lead to a swelling of the ranks of the uninsured, since reduced federal Medicaid contributions almost certainly would lead many states to restrict Medicaid eligibility and to remove some low-income people from the program. Research indicates that increases in the number of uninsured individuals would ultimately lead to poorer access to health care and higher levels of avoidable illness and mortality among vulnerable populations. For low-income children, lack of insurance and access to care could increase the number of days missed from school due to illness and ultimately impair educational opportunities.
- Some contend that increasing state flexibility in Medicaid, such as by allowing states to increase the amounts they can require low-income beneficiaries to pay to access health care, could help reduce costs without adverse consequences for beneficiaries. Experience indicates such claims should be treated with considerable skepticism. For example, the state of Oregon was recently given flexibility to impose premiums in its Medicaid program. The resulting premiums were as low as $4 per person per month. Yet many poor Oregon residents could not afford these premiums, and the number of people enrolled in Medicaid fell by half.[5] Most of those who lost Medicaid coverage became uninsured.
- A rise in the number of uninsured people also would trigger increases in uncompensated health care costs, as some people without insurance would come to emergency rooms when they became ill or sustained serious injuries. Such costs would end up being borne in part by state and local government hospitals and clinics, and in part by increases in the amount that hospitals and clinics charge private health insurers through cost-shifting. Increases in the ranks of the uninsured thus would likely trigger increases both in state and local government costs and in private health insurance costs.
- Efforts to hold growth in per-person Medicaid costs well below growth in private-sector health-care costs over an extended period of time eventually would lead to a two-tier system of health care, with Medicaid beneficiaries relegated to the lower tier. Since the rise in health care costs is driven primarily by advances in medical technology and treatments, it is not possible to hold Medicaid cost growth well below general health care cost growth year after year without steadily cutting back on the number of people that Medicaid insures or the health care services and treatments it covers. Unless we are willing to tolerate a steadily growing population of uninsured low-income Americans, holding Medicaid cost growth year after year to levels well below health-care cost growth in the private sector would mean that low-income Americans would eventually have to be denied the benefits of some medical advances that are available to other Americans.
- Federal cutbacks also would likely lead to reductions in Medicaid payments to health care providers. Such payments already are substantially lower in many states than the payments that private health insurance makes. Further reductions in such payments would likely cause fewer providers to accept Medicaid patients.
End Notes:
[1] This report has also been released, in slightly altered form, as an appendix to the report, “Cuts To Low-Income Programs May Far Exceed The Contribution Of These Programs To Deficit’s Return,” by Isaac Shapiro and Robert Greeenstein, Center on Budget and Policy Priorities, Feb. 5, 2005. Leighton Ku and Victoria Wachino also contributed to these analyses.
[2] John Holahan (director of the Urban Institute’s Health Policy Center) and Arunabh Ghosh, “Understanding the Recent Growth in Medicaid Spending, 2000-2003,” Health Affairs, January 26, 2005; Kaiser Family Foundation, news release, “A Sharp Rise in Enrollment During the Economic Downturn Triggered Medicaid Spending to Increase by One-Third from FY 2000-03,” January 26, 2005.
[3] This study also found that people with Medicaid and people with private insurance used health services at roughly comparable levels. Jack Hadley and John Holahan, “Is health care spending higher under Medicaid or private insurance?” Inquiry, 40:323-42, Winter 2003/2004. Similar findings were reached by federal researchers: see Edward Miller, Jessica Banthin, and John Moeller, “Covering the Uninsured: Estimates of the Impact on Total Health Expenditures for 2002,” Agency for Healthcare Research and Quality Working Paper No. 04407, November 2004.
[4] SCHIP stands for State Children’s Health Insurance Program; for children in low-income working families, SCHIP complements the Medicaid program.
[5] Oregon Health Research and Evaluation Collaborative, “Research Brief: Changes in Enrollment of OHP Standard Clients,” January 2004, and “Research Brief: The Impact of Program Changes in Health Care for the Oregon Health Plan Standard Population: Early Results from a Population Cohort Study,” March 2004.